Article



Specialist referral may be indicated if the Practitioner feels:
Antral disease
Paranasal sinuses are air-filled cavities in the dense portions of the bones of the skull lined with a ciliated mucosa, the mucus from which drains via openings (ostia) into the nose. The main sinuses are frontal, ethmoid, sphenoid and maxillary. Their main disorders are inflammatory and neoplastic. This section focuses on the maxillary sinus (antrum).
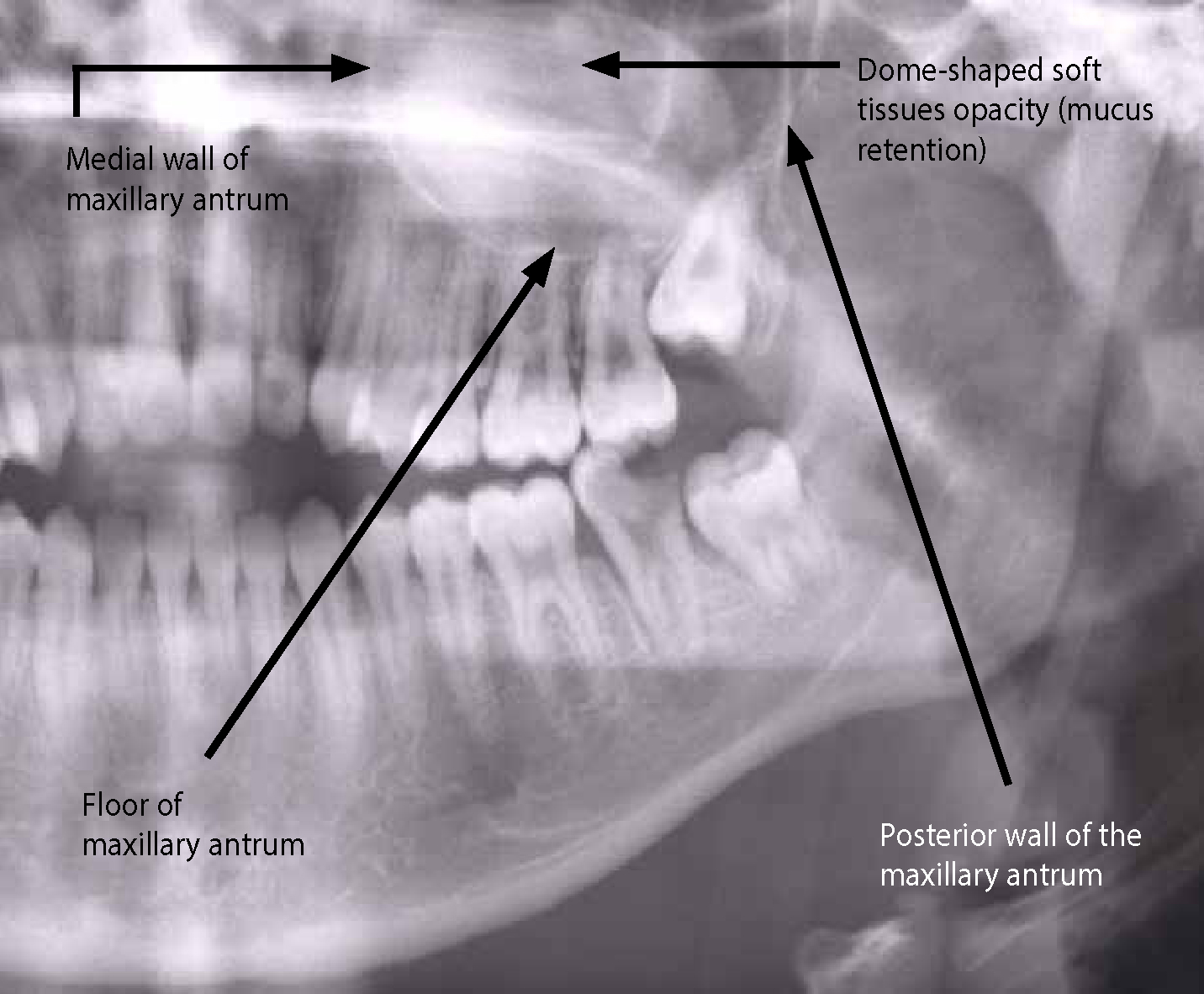
The floor of the maxillary antrum will be visualized in maxillary intra-oral films and in DPTs – where the medial and posterior wall can also be assessed (Figure 1).
Sinusitis
|
|
Bacteria are most commonly the cause, and incriminated are:
Diagnostic features
History
Symptoms can include nasal drainage (rhinorrhea or post nasal drip), nasal blockage, the sensation of swelling in nose or sinuses, ear symptoms, pain in teeth worse on biting or leaning over, halitosis, headache, fever, cough, malaise, etc (Table 2). Symptoms are typically less severe in chronic sinusitis.
| Location | Location of pain | Other features |
|---|---|---|
| Maxillary | Cheek and/or upper teeth | Tenderness over antra |
| Frontal | Over frontal sinuses | Tenderness of sides of nose |
| Ethmoidal | Between eyes | Anosmia, eyelid swelling |
| Sphenoidal | Ear, neck, and at top or centre of head |
Clinical features
There may be nasal turbinate swelling, erythema and injection (dilated blood vessels), mucus, sinus tenderness, allergic ‘shiners’ (dark circles around eyes), pharyngeal erythema, otitis, etc.
Diagnosis is from the history, plus sinus tenderness and dullness on transillumination. Nasendoscopy can visualize the mucosal surface inside the maxillary or sphenoid sinus in over 50% of patients. Nasal cytology with a rhinoprobe may help and ear examination is important.
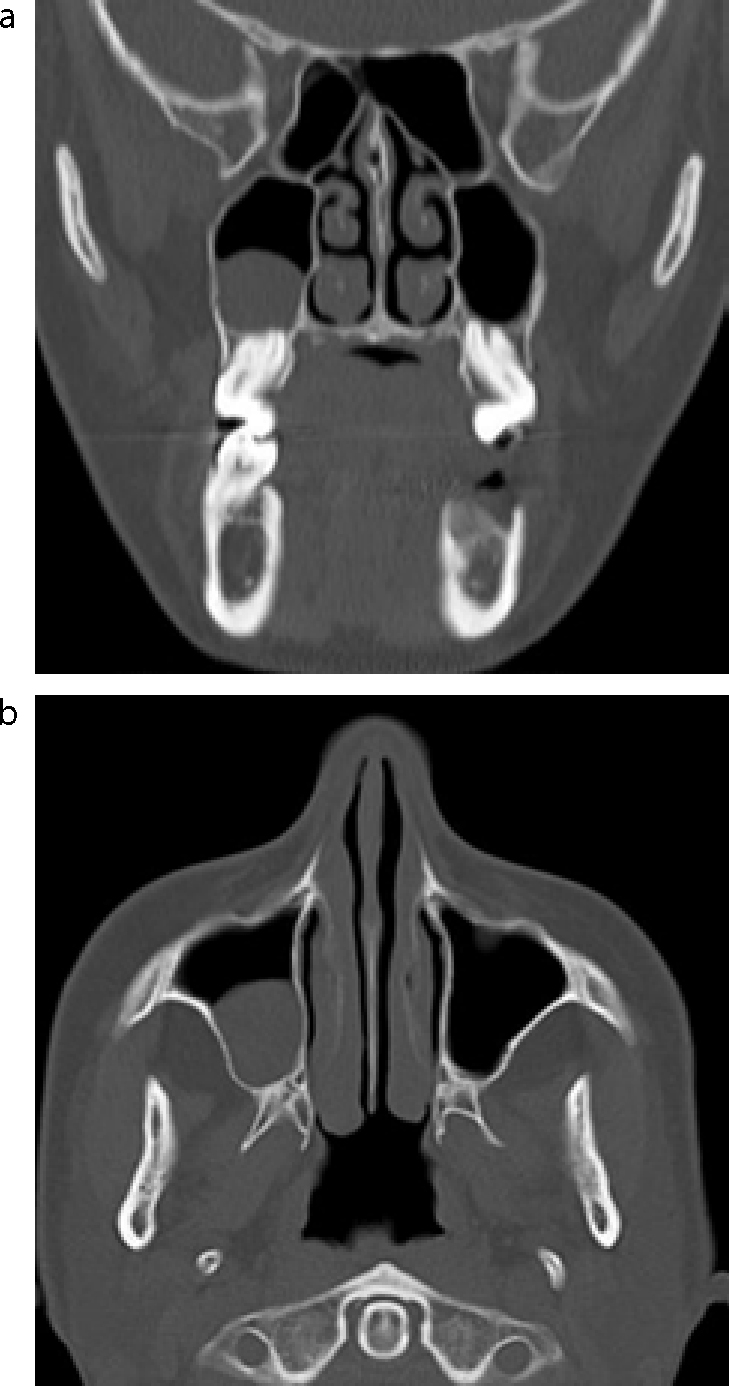
Acute sinusitis is diagnosed and treated clinically and does not require imaging. If symptoms persist after 10 days of treatment, CT is recommended when the results may affect management. Plain films are not recommended as the findings are usually non-specific. Differentiating between sinusitis and URTI is difficult. Antral radio-opacities in children under age 6 years can be difficult to evaluate since they are seen in up to 50%. In adults, a sinus radio-opacity may be due to mucosal thickening or a mucous retention cyst (Figures 2 and 3) but a fluid level is highly suggestive of acute sinusitis. Corticated opacities occurring in the maxillary antrum indicate that the aetiology of the opacity is extrinsic to the antrum, eg an apical radicular cyst (Figure 4). MRI may be recommended if there are complications such as peri-orbital infection, or to rule out malignancy.


It may sometimes be necessary to perform a needle aspiration sinus to confirm the diagnosis, and sample infected material to culture to determine what micro-organism is responsible.
In patients with recurrent or recalcitrant sinusitis, cystic fibrosis and immunodeficiencies may need to be excluded.
Management
Acute sinusitis resolves spontaneously in about 50%, but analgesics are often indicated and other therapies may be required, especially if symptoms persist or there is a purulent discharge.
Intranasal steroids are helpful in many patients, although studies evaluating the efficacy have not been conclusive. Antihistamines are used for patients with significant allergic symptoms. Oral decongestants help, but typically may be used for 3–7 days only as longer use may cause rebound and rhinitis medicamentosa. Guaifenesin helps thin and increase clearance of secretion. Buffered saline lavage may help in clearing secretions. Hot steam is often helpful.
Antibiotic treatment for at least two weeks in acute sinusitis and at least three weeks in chronic sinusitis is commonly required. Treatment for acute sinusitis is amoxicillin, ampicillin or co-amoxiclav (erythromycin if penicillin-allergic), or a tetracycline such as doxycycline or clindamycin. Chronic sinusitis responds better to drainage by functional endoscopic sinus surgery (FESS), plus antimicrobials (metronidazole with amoxicillin, erythromycin, clindamycin or a cephalosporin). Open procedures including the classical Caldwell-Luc operation are generally outmoded.
Neoplasms
Diagnostic features
These tumours can remain undetected until late. When they infiltrate branches of the trigeminal nerve they cause maxillary pain. As the tumour expands the effects of expansion and infiltration of adjacent tissues become apparent as intra-oral alveolar swelling, ulceration of the palate or buccal sulcus; swelling of the cheek; unilateral nasal obstruction often associated with a blood-stained discharge; obstruction of the nasolacrimal duct with epiphora; hypo-or anaesthesia of the cheek; proptosis and ophthalmoplegia consequent on invasion of the orbit and trismus from infiltration of the muscles of mastication.
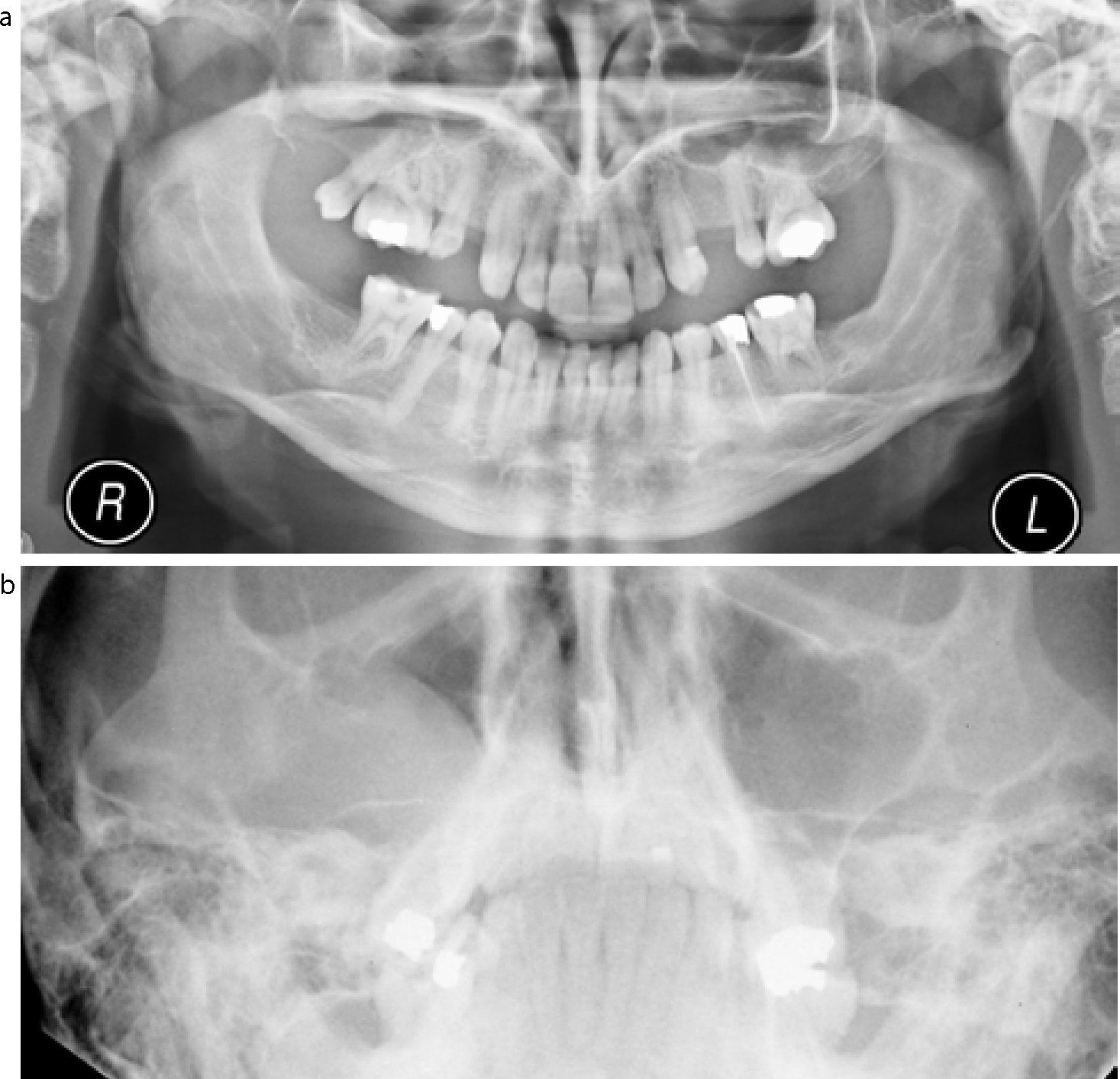
Diagnosis is supported by endoscopy, radiography (Figures 5a and b), magnetic resonance imaging and biopsy.
Management
Combinations of surgery and radio-chemotherapy are usually required.
Prognosis is poor with a < 30% 5-year survival.

