Aesthetic considerations
There are a number of factors that contribute to dental aesthetics, and it is beyond the scope or intention of this article to discuss these at length. The reader is referred to standard texts on the subject for further information and a useful reference is A Clinical Guide to Anterior Dental Aesthetics,1,2,3,4,5 a series of articles, which have been collated into a book for publication.
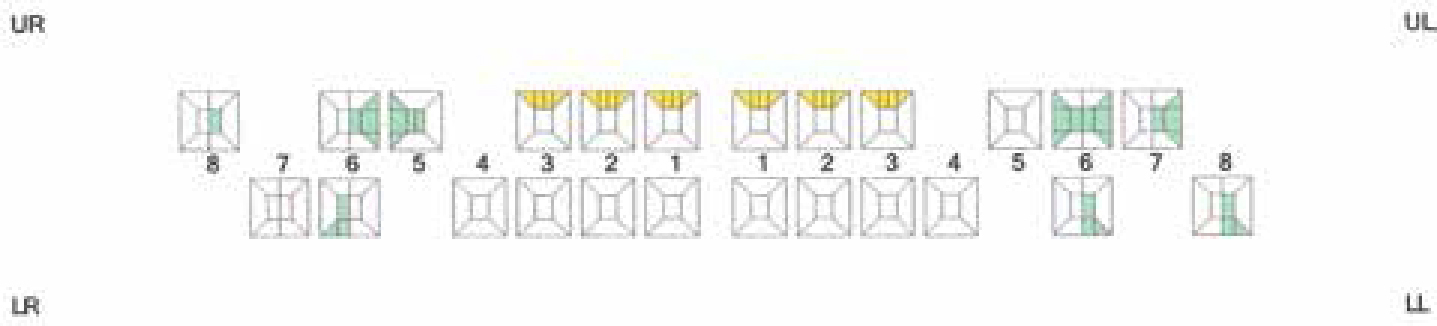
In order to achieve the patient's objectives in this case, the following changes were planned.
Crown-lengthening surgery
This presented the opportunity to:
Reduce the excessive gingival display;
Correct the gingival level discrepancies between the lateral incisors;
Enable the central incisors to be proportioned more correctly;
Central incisors form the focal point of the smile and the width/height ratio should be approximately 0.75–0.8 for unworn maxillary incisors.6 Raising the gingival level allowed for the height of the central incisors to be increased and modified to approximate this proportion, thus reducing their ‘squareness’.
Replacement veneers
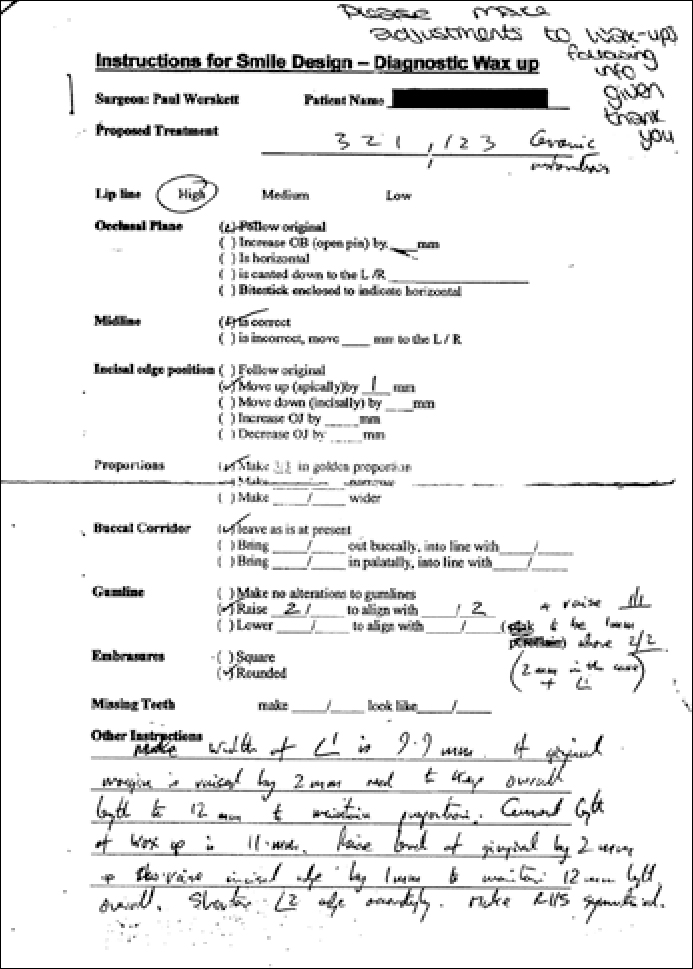
The design for the new veneers was prescribed to the laboratory by using a ‘diagnostic wax-up prescription form’ which the author uses in his practice. This directs the technician to construct the wax-ups in line with the clinician's requirements, rather than the technician's assumptions. As a result, the veneers were designed to achieve symmetry, balance and harmony, with consideration for golden proportion in line with generally accepted principles of anterior dental aesthetics.7,8,9,10,11
Clinical considerations
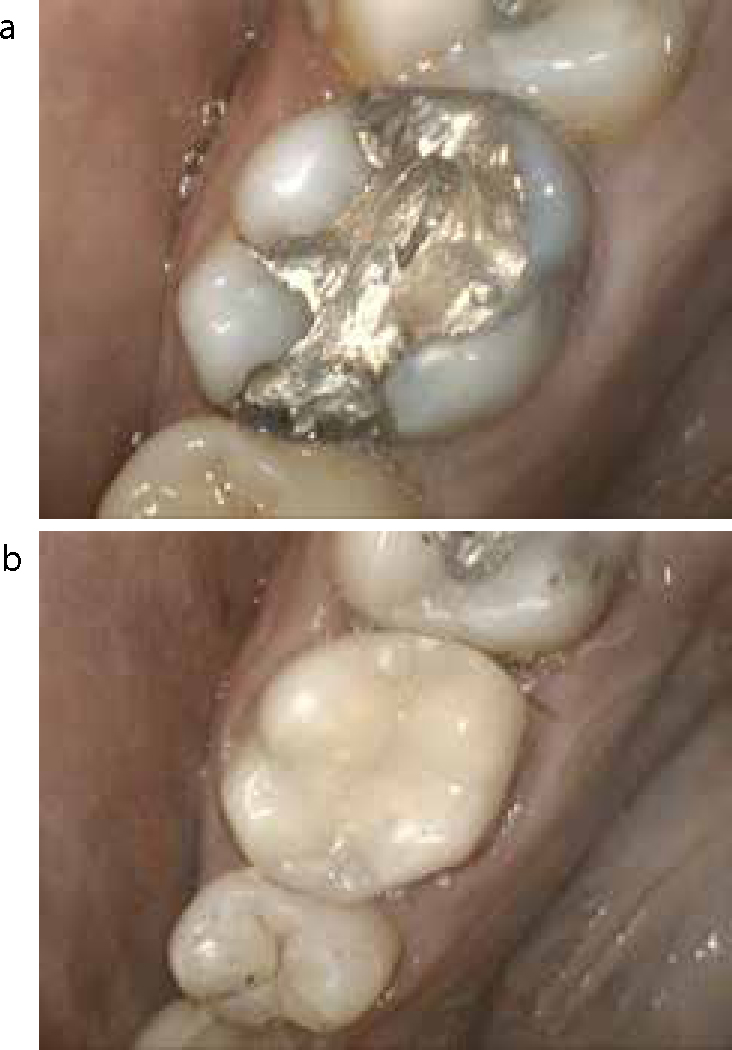
It is unfortunate that the patient had already been committed to porcelain veneers, as these are irreversible restorations. With the benefit of hindsight, other treatment alternatives might have been considered which may have provided a more conservative solution. These might have included orthodontics, to improve the tooth positions and close spaces, if the natural teeth were otherwise satisfactory in appearance and condition; and composite resin restorations, which can achieve satisfactory short to medium term results and have documented satisfactory performance. Success rates for composite resin restorations have been quoted at 50% survival at 8–9 years,12 although this may be as low as 6 years in toothwear cases.13 However, composite resin restorations are not necessarily invasive and avoid the tooth destruction associated with veneer preparation. Unfortunately, there was no other option in this case but to replace the failed porcelain restorations with new porcelain veneers.
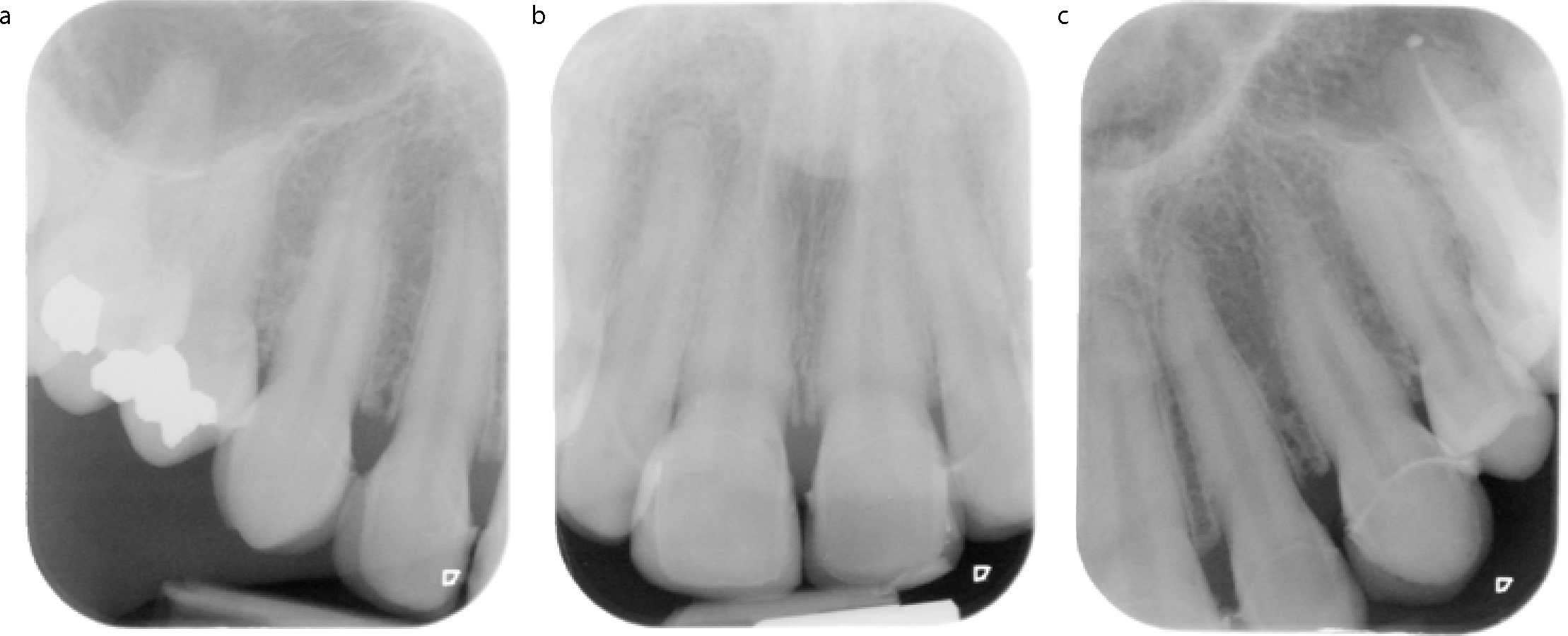
The use of porcelain laminate veneers were first described in 1983 as a method of restoring teeth14 and has become a common treatment modality over the years as a means of improving the appearance of the anterior teeth. In England and Wales, porcelain veneers placed under NHS regulations achieved a 53% survival rate over 10 years.15 When planned well and executed with care and precision, treatment results can be very satisfactory and the longevity can also be acceptable, although the chances of success are improved when preparation margins do not extend beyond enamel.16, 17 When the finishing margin is in dentine, the success of veneers is reduced, with an increased risk of fracture, poorer marginal integrity and greater discoloration.18 However, the success rate for veneers may be more than 90% over 10 years and as much as 93% over 15 years.16,18,19 Unfortunately, even when performed to high standards, irreversible damage is inflicted on the dental hard tissues, which can only compromise the long-term survival of the teeth. When performed poorly, and with little regard for occlusal function and health of the dental tissues, significant damage can result. The risk of irreversible pulp damage due to tooth preparation may be around 20%.20 Furthermore, the restorations themselves may fail. A significant reason for failure of porcelain veneers is fracture of the porcelain.16 In this particular case, different types of porcelain fracture were noted. At UR2, a longitudinal fracture indicated a static fracture. This may be due to occlusal loading, cyclical fatigue or polymerization shrinkage.16 Incisal edge fractures are an example of a cohesive fracture, which in this case was likely due to excessive occlusal loading.16 In some patients, bruxism may be a cause of fracture and tooth surface loss and, in such cases, consideration should be given to protecting restorations from occlusal dysfunction, where possible.21 This can be achieved with an acrylic occlusal stabilization splint, which will also achieve muscle relaxation and reduce the tendency for bruxism.22,23
In this particular case, the use of diagnostic wax-ups enabled the design of an occlusal scheme whereby the occlusion of the anterior teeth was protected from interference in lateral excursion by directing the guidance away from the incisal edges of the anterior maxillary incisors in excursive movements. The provisional restorations were designed with the same morphology to allow a period of evaluation in the mouth. Following successful review, the successful occlusal scheme could then be copied into the final porcelain restorations by making a study cast of the provisional restorations and creating a custom incisal guidance table so that the laboratory could duplicate the occlusal scheme.23
Poorly planned and executed treatment not only compromises the patient's oral health, but can also cause dissatisfaction and unhappiness for the patient. To add further insult, the treatment also brings with it financial compromise due not only to the cost of the original treatment, but also the costs involved in corrective treatment. Therefore, before embarking on elective treatment, such as aesthetic treatment which is not clinically necessary, it is imperative that patients are made fully aware of the significance and consequences of any proposed treatment and the possible long-term implications with respect to further treatment need and the costs which would be incurred, both financial and clinical. Only when this has been done can the patient give full and complete informed consent to the treatment, as required by the General Dental Council,24 safe in the knowledge that they understand the risks that they are accepting by embarking on the treatment. For the ethical practitioner, this is an essential approach to patient care, not only as a professional duty of care, but also to reduce the possibility of a potentially damaging litigation claim.