Abstract
Parts 1 and 2 of this article addressed the care of children with cleft of the lip and/or palate until age 10. The third part of this article discusses their care until adulthood.
From Volume 41, Issue 10, December 2014 | Pages 876-881
Parts 1 and 2 of this article addressed the care of children with cleft of the lip and/or palate until age 10. The third part of this article discusses their care until adulthood.

Just as at age 5, a series of audit records are undertaken at age 10 (Table 3, Part 1) including an assessment of speech, hearing and psychology, with parent and patient satisfaction and the outcome of alveolar bone grafting being recorded on the audit database.
The psychological health of children (and indeed their family) is crucial to overall health. As children begin early adolescence, they become more interested in their appearance. Body image concerns resulting from lip scars, abnormal dentofacial relationships and negative self-perception, in addition to speech problems and difficulties with hearing, can affect self-confidence and relationship building.1 Where there are any concerns about psychological well-being, psychological support and intervention may be necessary during childhood and adolescence and, on occasion, in adulthood as well to help the patient and family develop coping strategies. The transitions between these stages are often the times at which input from a clinical psychologist is most desirable as transitioning involves establishing new relationships, among other challenges. Unfortunately, in some geographic areas of the UK, clinical psychology services for cleft lip and palate care are poorly resourced. However, other members of the multidisciplinary team offer help and advice where possible.
Charities, such as the Cleft Lip and Palate Association (CLAPA), Changing Faces (www.changingfaces.org.uk), Let's Face It (www.lets-face-it.org.uk), and Contact a Family (www.cafamily.org.uk) provide invaluable resources and support for individuals and families. All provide their information in different formats with different levels of interactivity to suit their primary users and, with the ability to browse web pages and social media on mobile devices, there is non-NHS psychological support available for all. The ability for patients to get involved in fundraising and supporting other families through these charities and local CLAPA groups is often humbling for members of the multidisciplinary cleft team.
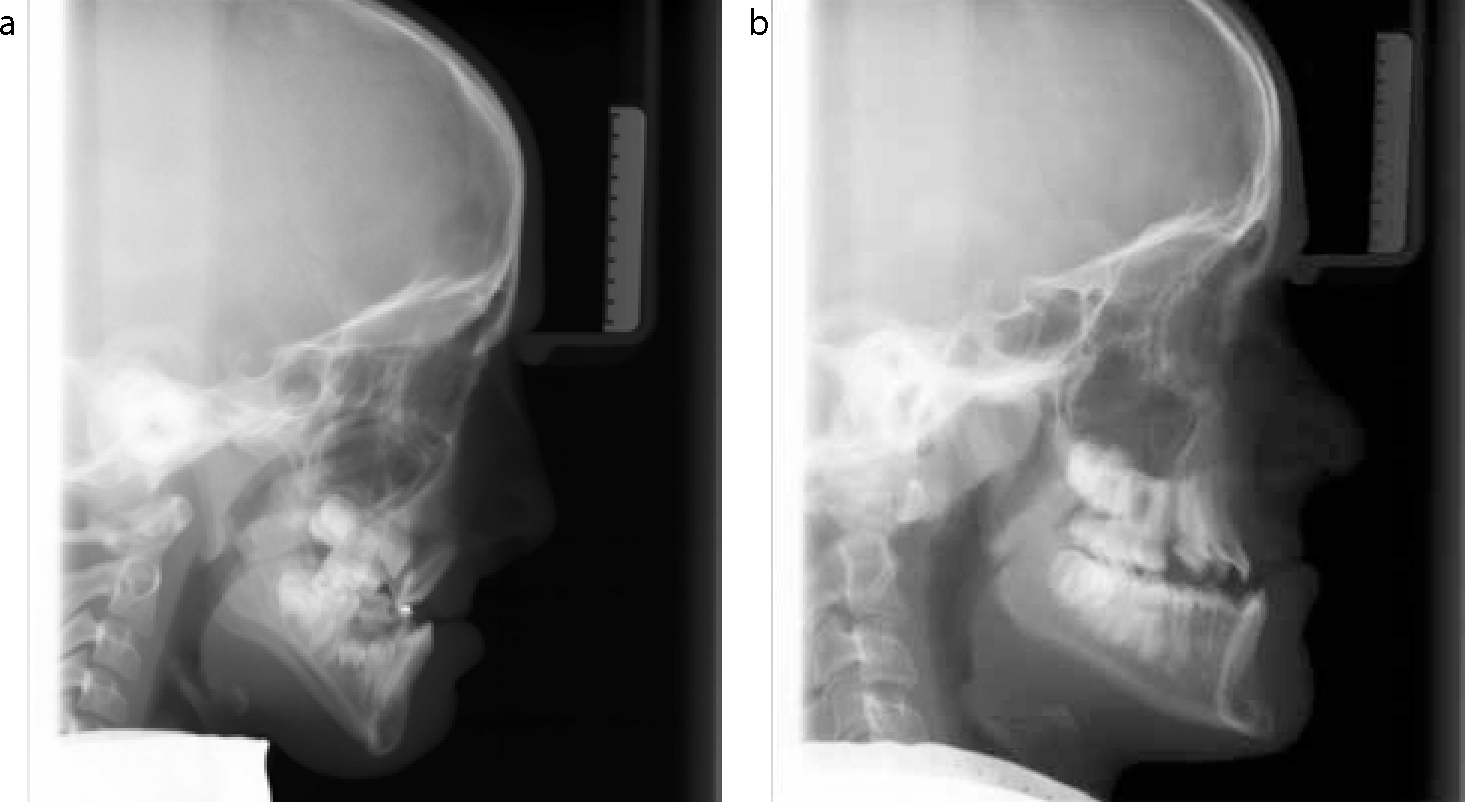
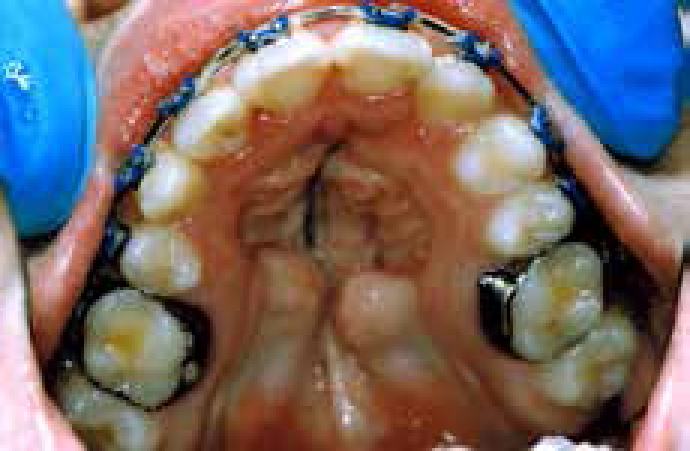
All children with a cleft involving the alveolus and most children with other types of cleft will require orthodontic treatment. Severely rotated incisors, hypoplasia/microdontia (Figure 1), hypodontia (Figure 2), supernumerary teeth and delayed eruption of permanent teeth are frequent occlusal anomalies in children with alveolar clefts. While those with isolated lip or palate clefts usually have localized occlusal anomalies, such as incisor rotations, crowding or crossbites, there is an increased prevalence of Class III malocclusions and underlying Class III skeletal discrepancies among children with clefts (Figure 3 a, b). The growth disturbance is thought to be in part as a consequence of primary surgery, although other non-cleft family members may also have Class III relationships. When set against a background of non-cleft orthodontic problems, such as loss of arch length from extraction of deciduous teeth, impacted incisors/premolars/molars, generalized crowding, etc, the orthodontic management for children with clefts is complex. Some patients with clefts have impacted canines despite alveolar bone grafting (Figure 4), requiring exposure and orthodontic traction. Parents are reassured that all children with a cleft of the lip and/or palate score 5p on the Dental Health Component of the Index of Orthodontic Treatment Need (IOTN), irrespective of any other occlusal traits, and are therefore eligible for fully funded NHS treatment in the UK.


Treatment should be co-ordinated by the cleft orthodontist to ensure orthodontic treatment does not conflict with other ongoing care (eg speech and language therapy) and also to minimize the burden of care by integrating audit record collection with active orthodontic treatment. Tooth movement will invariably involve fixed appliances (Figure 5) and extraction planning can be complex, particularly where there are issues with tooth morphology, tooth position and/or tooth quality. In cases with a missing permanent maxillary lateral incisor tooth, a decision will need to be made about opening space for a bridge or implant-retained crown or, alternatively, closing the space and re-shaping the permanent canine (Figure 6).2 Where a marked Class III malocclusion is emerging, alignment of the upper arch may be undertaken in isolation, with the patient and parents being informed of the potential requirement for adjunctive orthognathic surgery at the completion of skeletal growth.
Speech and language therapy may be required for articulation disorders that transpire, whilst velopharyngeal insufficiency (VPI) issues that develop with further growth require further assessment and surgical care where appropriate. Audiological problems are also addressed as they arise and regular contact with the audiologist/ENT specialist via the multidisciplinary clinic can identify issues that require further investigation. Chronic otitis media can result in destruction of the middle ear bones and ear drum. In such cases, conventional hearing aids are unlikely to offer any hearing improvement and a bone-anchored hearing aid (BAHA) may be considered. Clearly, regular input from the primary care dentist to ensure good oral health is important, particularly during periods of active orthodontic treatment. Dietary counselling by the primary care dentist is required where any caries or erosion is detected. Second permanent molars and premolars should be fissure-sealed and a fluoride-containing mouthwash prescribed for children at high risk of further caries, while good communication with the cleft orthodontist is essential where there are teeth of poor prognosis requiring extraction.3 Adolescent patients with clefts will take an increasing interest in dental aesthetics and can be disappointed to discover that any advanced restorative dentistry may need to be postponed until other aspects of care/facial growth are complete. Composite resin build-ups can, however, be used to improve dental aesthetics on a short- to medium-term basis. Advice should be sought at this stage about the need for further bone grafting should an implant-retained crown be under consideration for a missing permanent maxillary lateral incisor, which occurs in 50% of cases with alveolar clefts.4
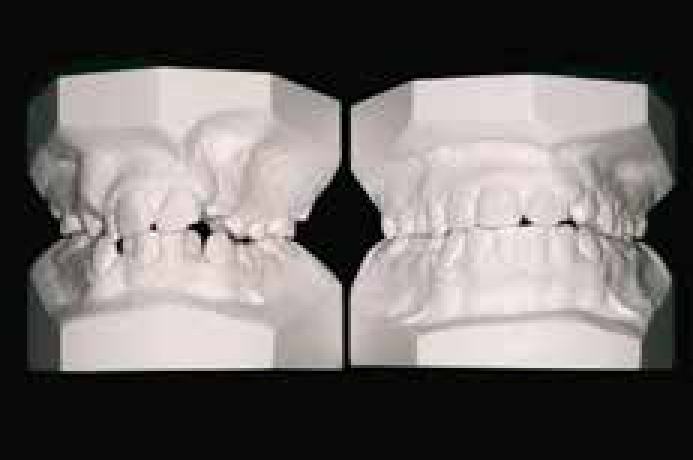
During the adolescent years, the underlying dentoskeletal relationships will become established and, as described above, any marked discrepancy will have been identified by the cleft orthodontist. Patients and parents are often eager to find out what treatment will be possible to correct severe Class III occlusal and skeletal relationships (Figure 7). Therefore, an orthognathic surgery consultation is worth considering at an early stage in order to provide general information on the interaction and sequence of treatment. This will usually indicate that, as skeletal growth is being completed, a follow-up consultation to discuss the proposed treatment in more detail will be required. As most patients with a cleft and a severe Class III malocclusion will require a maxillary advancement, arrangements will be made at this point for an assessment of the velopharyngeal function using lateral videofluoroscopy (Figure 4, Part 2) and nasendoscopy. This will help determine the effects of any maxillary advancement on the speech quality and resonance and, where the patient is considered to be at high risk of VPI post-orthogathic surgery, advice will be given about corrective velopharyngeal surgery afterwards. Pre-surgical orthodontic treatment involves fixed appliances (Figure 8) and, although full decompensation will be desirable (in order to achieve the maximal surgical change), issues such as tooth morphology and extent of alveolar bone may limit this. As the surgical procedure is more complex than in a non-cleft patient due to scarring and underlying anatomical variations, distraction osteogenesis may be considered to minimize the effect of the maxillary advancement on the soft-palate function for speech. Post-surgery, the case is completed with a continuation of the orthodontic treatment to establish as near as possible an ideal occlusion, with the retention phase being monitored closely as the potential for surgical and orthodontic relapse following an orthodontic/orthognathic case is increased in patients with a cleft. Finally, a follow-up velopharyngeal function assessment is undertaken at six months post-surgery to determine the impact on speech, with any further speech surgery being discussed with the patient.


Any revision surgery is planned, as necessary, for the individual patient. A lip revision or dermal filler may be considered where there is any aesthetic impairment at rest or during function from earlier surgery. Many patients will request a rhinoplasty to improve nasal symmetry and projection (Figure 9). This must, however, be deferred until after the orthognathic surgery has been completed as the effect of any maxillary surgery on nasal projection is impossible to determine. Finally, any residual fistulae that are symptomatic should be closed at this stage and problems with velopharyngeal insufficiency should be investigated and treated as necessary. For some patients with VPI, where surgery is not indicated, a palatal lift appliance (Figure 10) will be indicated to ‘lift’ the soft palate to improve speech quality.


All aspects of care provided by the multidisciplinary cleft team should be complete by age 20 and although, in general, no formal arrangements are made for follow-up after this point, most teams are more than happy to provide ongoing care, as necessary, for patients with a cleft. This may involve further aesthetic and functional surgery, speech and language therapy and audiological support and orthodontic advice and treatment, as necessary. The primary care dentist will be able to continue to provide ongoing dental care and either carry out, or refer the patient for, advanced restorative dentistry, as necessary, particularly where dental implants are under consideration. It is unfortunate that, in some areas of the UK, advanced restorative dentistry in secondary care is not fully funded for patients with clefts. Finally, most cleft teams will offer a clinical genetics referral to all patients around age 20 in order that they have appropriate family planning information regarding the recurrence risk in any children they may have.
It is important that the patient is offered an opportunity to discuss any remaining concerns with the clinical psychologist at the end of the schedule of co-ordinated care, particularly around the time when orthognathic surgery is being considered.1 Psychosocial problems involving perceived poor facial appearance and personality stereotyping may contribute to poor social standing and poor social interaction and, in addition, may contribute to the breakdown of family relationships. These can be compounded by social difficulties due to speech and hearing problems, which can result in high levels of negative self-perception and complex body image issues. It is known that educational achievement in people with clefts is lower,5 whilst employability and economic performance are sadly reduced. The prospects for fulfilling personal and romantic relationships can sometimes be severely adversely affected. Of note is the fact that the rate of suicide is higher for young adults with clefts than in the general population.6 Therefore, where there are significant psychological issues, the clinical psychologist will aim to up-skill the patient to engender resilience to deal with the challenges of day-to-day life through a ‘person first, cleft second’ strategy. In time it is hoped that social networking will be able to provide 1:1 psychological support for patients with psychological issues.
Multidisciplinary cleft teams also provide care for a cohort of non-standard patients, including those with submucous cleft palate, non-cleft velopharyngeal insufficiency and migrant families.
Submucous cleft palate occurs where there is mucosal continuity, but submucosally the posterior aspect of the hard palate and soft palate have a cleft. This is nearly impossible to diagnose in babies and can be difficult to diagnose in young children, but poor speech development can be an indicator. Following diagnosis via digital palpation of the hard and soft palate and other tests, as necessary, treatment follows the same principles as detailed earlier.
Children without a cleft can suffer from non-cleft velopharyngeal insufficiency and account for around 20% of the overall caseload of a multidisciplinary cleft team. In the absence of any neurogenic cause (eg dysarthia, stroke, cranial nerve injury), patients may not demonstrate any other phenotypic signs and the aetiology is considered to be structural, resulting from a tissue deficiency. In other cases, subtle phenotypic features can lead the cleft team to a potential diagnosis of syndromic VPI, such as velocardiofacial syndrome or DiGeorge syndrome. Confirmation of one of the chromosome 22q11 microdeletion syndromes by the clinical geneticist can be very useful for the family in co-ordinating other aspects of medical care (eg cardiac anomalies, autoimmune disorders, seizures due to hypocalcaemia, etc) and accessing learning support for educational difficulties and learning disabilities at school. Diagnosis of other syndromes may require the assistance of a dysmorphology database where there are less common phenotypic features. For these patients, surgical and speech and language therapy follows the principles outlined above, although intellectual impairment may impact on the overall outcome of care.
Where Stickler syndrome is confirmed by a clinical geneticist, referral to an ophthalmic surgeon for an assessment of retinal health (vitreoretinal changes such as thinning of the retina are characteristic of Stickler syndrome) and the potential for retinal detachment is essential. As Stickler syndrome is an autosomal dominant condition, consideration should be given for an assessment by the ophthalmic surgeon of other family members as well.
In earlier sections of this article, electropalatography and palatal lift appliances have been described and can also be of use in older patients to assist with speech. In some patients, surgical closure of the palatal cleft is not possible due to a lack of soft tissue to close the defect fully and, in other cases, medical complications preclude surgery. Furthermore, there is a small group of gerodontic patients who were never offered a comprehensive surgical service. For these patients, an obturator may be considered to close the defect and, in certain cases, this can be incorporated in a complete upper denture (Figure 11).

Families moving within the UK can access care in a relatively seamless manner, however, where transfer of care between multidisciplinary teams fails, the primary care dentist should refer the patient to the new multidisciplinary team to ensure overall cleft care continues. Multidisciplinary cleft teams find patients from other areas of the globe, especially the developing world, a challenge, particularly where there are poor records of the presenting phenotype/care provided to date. This is in addition to the communication issues where the first language is not English, which has added complexities for speech and language therapy.
The care of patients with clefts of the lip and/or palate is challenging and requires input from a diverse group of medical, surgical, dental and parasurgical specialties. Co-ordination of care is of paramount importance to ensure that patients receive the right care at the right time delivered by the right professional in the correct location. In addition to individual patient care, the multidisciplinary cleft team has a role in monitoring care through defined audit programmes and reconfiguring services, where necessary, to ensure public sector resources are used as effectively as possible.
The primary care dentist has an important role in the overall management of patients with clefts, both in relation to prevention of caries, erosion and periodontal disease, and also in monitoring developing occlusal problems, undertaking extractions and in providing routine and advanced restorative dentistry, as appropriate for the patient. Because the dentist-patient/parent relationship is of a long-term nature, the primary care dentist can also provide useful support and advice for families as they progress through the care pathway.