Abstract
The rates of syphilis in the UK are rising. Syphilis is a bacterial sexually transmitted infection caused by
From Volume 49, Issue 9, October 2022 | Pages 738-740
The rates of syphilis in the UK are rising. Syphilis is a bacterial sexually transmitted infection caused by
Syphilis is a contagious bacterial infection caused by the Treponema pallidum spirochete. It can be acquired or congenital.
The UK has experienced a resurgence in syphilis rates over the past decade.1,2 In 2019, 7982 new cases of syphilis were diagnosed in the UK, marking the highest incidence since the 1940s.1 London, Brighton and Manchester experienced the greatest increase in prevalence.
Between 2015 and 2019, the rate of syphilis diagnoses rose by 50%.3 The cohort of 25–34 year old men who have sex with men (MSM) showed the greatest increase in cases,3,4 and 40% of those diagnosed with syphilis had concurrent HIV infection,5 which is not surprising as syphilis is known to facilitate HIV acquisition and transmission.6 The oral cavity is the most commonly affected extragenital site for primary syphilis.7
Syphilis has been termed ‘the great imitator’ because it has diverse clinical manifestations, mimicking other conditions, and is thus vulnerable to misdiagnosis.8 Dental professionals should therefore be well trained in recognizing the oral manifestations of the disease, which are more prevalent in the primary and secondary stages.
Acquired syphilis is caused by the spirochete directly entering the body through a break in the skin or mucosa. This most commonly occurs due to direct sexual contact (usually vaginal, anal or oral) or by the sharing of contaminated sex toys; or less commonly by non-sexual contact, intravenous (IV) drug use or infected blood transfusions.5 Without treatment, syphilis can progress from primary, to secondary, latent and tertiary stages. Different clinical signs and symptoms are associated with each stage.
The incubation period is 10–90 days (mean 21 days) following which, clinical signs and symptoms of infection may start to manifest.10 Primary syphilis is characterized by a chancre and regional lymphadenopathy.2,7 A chancre is typically a solitary, indurated, painless ulcer that develops after inoculation at the site of entry of T. pallidum. They may present on the tongue, lips, tonsils or anogenital region.9,11,12 The chancre spontaneously heals within 3–8 weeks.5 If left untreated during this period, the T. pallidum haematogenously disseminates throughout the body and progresses to the secondary stage.
Secondary syphilis occurs 2–24 weeks (mean 2–12 weeks) after innoculation.9 Typical presentation involves a maculopapular rash mainly affecting the palms and soles, generalized lymphadenopathy, a sore throat and flu-like symptoms.4,5,8,12,13
Oral lesions can present as irregular, linear mucosal erosions which coalesce to form ‘snail track’ lesions.8 Condylomata lata are verrucous plaques resembling viral papillomas and can arise on the tongue, buccal mucosa or in the oropharyngeal region. Split papules, also known as ‘split-pea’ lesions, manifest as a red macule at the oral commissure, which becomes fissured. Hairy leukoplakia-like lesions affecting the tongue may also be present. All of these lesions are all highly infectious.5
Symptoms can spontaneously resolve and if left untreated, the disease enters the latent stage.5
The latency stage is asymptomatic, less infectious, and typically lasts 10–40 years.12 This subclinical infection can only be detected serologically.2,8 Without treatment, one-third of patients will develop tertiary syphilis.5,12
Tertiary syphilis typically presents 20–40 years following infection and can affect one-third of untreated cases.5 This destructive stage manifests as gummata, cardiovascular and neurological complications.4,5,9,11,12 Oral manifestations may present as diffuse atrophic glossitis owing to the atrophy of the filiform and fungiform papillae, leukoplakia-like lesions or locally destructive granulomatous gummata, with the latter typically affecting the hard palate.2
Congenital syphilis is contracted via the transplacental route. Infection in pregnancy can result in miscarriage, stillbirth or neonatal death.12 Babies who survive are more likely to be premature or of low birth weight. Congenital syphilis is also categorized into early (within 2 years of birth) and late stages.5 Some cases may be asymptomatic, and therefore do not present until the late stage.12
Late syphilis commonly presents with the Hutchinson's triad of malformed teeth (Hutchinson incisors and mulberry molars), interstitial ocular keratitis and deafness due to vestibulocochlear nerve damage.5 Hutchinson incisors are peg-shaped and notched, whereas mulberry molars are dwarfed molars with cusps covered with globular enamel growths. Other craniofacial manifestations include frontal bossing, saddle nose, high arched palate, palatal perforations, rhagades (deep fissuring at the angles of the mouth and nose), a prognathic mandible and a hypoplastic maxilla.5
In the UK, rates of congenital syphilis remain low (0.069% prevalence) as pregnant women are routinely screened for syphilis during the first trimester.1
Diagnosis of syphilis can be difficult. First, its clinical presentations vary widely. Secondly, it is not possible to culture T. pallidum on artificial media as it requires a human host to survive. Thirdly, histological features of syphilitic lesions tend to be non-specific and can mimic other conditions.2, 16
The UK Standards for Microbiology Investigations provide guidance on syphilis testing.15 Investigations involve a combination of direct tests such as polymerase chain reaction and dark field microscopy, which demonstrate the presence of T. pallidum in the syphilitic lesion. Serology tests are also used to detect treponemal IgG and IgM, although false-negative results in the primary stage of disease can make diagnosis challenging.
Syphilis has been coined ‘the great imitator’ as it can mimic other diseases. Table 1 provides some examples of this. These conditions should be considered in the list of differential diagnoses.
| Ulcers | Traumatic ulceration |
| Malignancy | Squamous cell carcinoma |
| Reactive | Necrotizing sialometaplasia |
| Autoimmune | Oral lichen planus |
| Bacterial | Tuberculosis |
| Viral | Herpes simplex virus |
| Fungal | Candidosis |
Owing to the broad spectrum of syphilitic manifestations, a high level of suspicion is prudent, and prompt referral should be undertaken if pathology of unknown cause is identified.
A 54-year-old man was referred to the local oral and maxillofacial department by his general dental practitioner, with a 2-week history of a non-healing ulcer on his tongue. The ulcer was painless, but had increased in size since initial presentation. He did not recall any trauma to the area and denied the presence of any similar lesions in the past.
The patient was otherwise fit and healthy and was not taking any medications. He had no known allergies. He was a non-smoker and rarely drank alcohol.
Clinical examination revealed a well-defined, depapillated, round ulcer surrounded by a white halo on the left dorsal surface of his tongue (Figure 1). There was no other intra-oral pathology to note and no cervical lymphadenopathy. The patient wore a partial denture, which he did not remove at night.
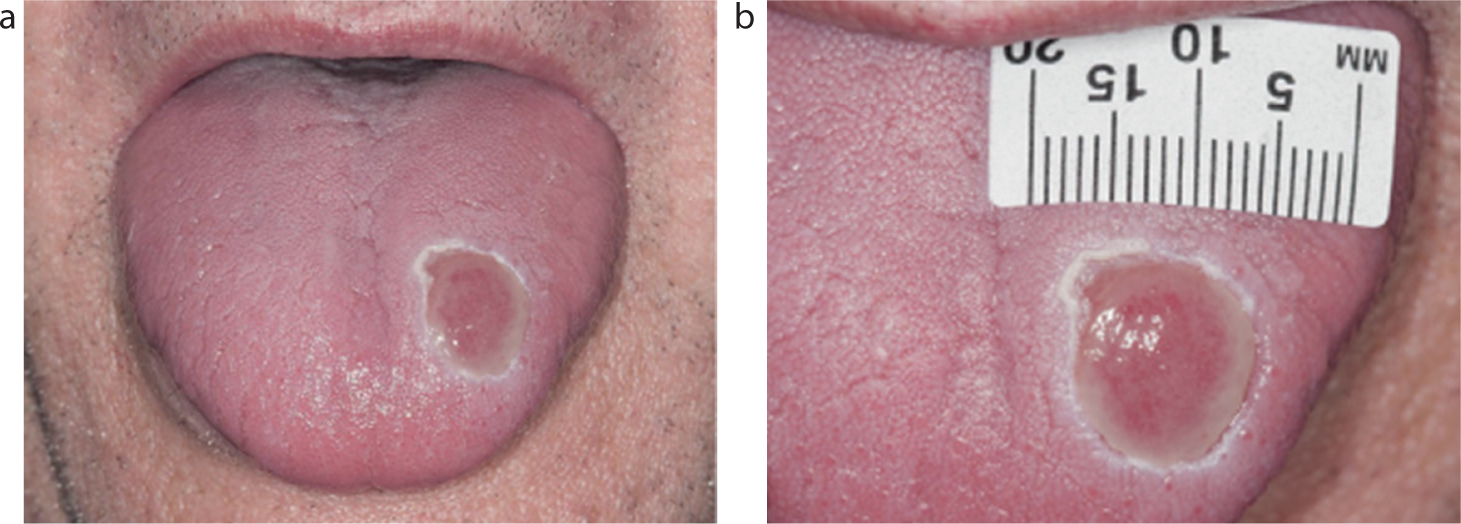
At this stage, the clinical impression and provisional diagnosis was that of a non-specific healing ulcer of unaccountable cause. Initial treatment involved denture hygiene instruction, warm salty mouthwashes and fluconazole, following a microbial swab of the ulcer which showed a heavy growth of Candida albicans. Unfortunately, this did not result in any improvement and an increase in the size of the ulcer was observed. A punch biopsy of the ulcer was therefore performed.
Histopathological examination revealed loss of the surface epithelium, and the deep connective tissues showed dense plasma cell aggregates with a perivascular distribution. These features, although non-specific, were deemed unusual for a traumatic ulcer and raised suspicion of syphilis. Immunohistochemistry for T. pallidum showed scattered positivity within the inflammatory infiltrate. These features were consistent with a syphilitic ulcer.
The patient failed to attend his follow up appointment for his biopsy result because he reported that the ulcer had completely healed. Further management of his condition was therefore promptly arranged with the genitourinary medicine team. Here, the patient was given advice regarding his diagnosis. A full sexual history and contact tracing was carried out and he was offered screening for other sexually transmitted infections (STIs), including HIV. The first line of treatment for syphilis is a course of penicillin (doxycycline can be used as an alternative) and the patient was advised to abstain from sexual contact for 2 weeks after treatment was completed. It further transpired that he had previously been treated for syphilis and had not volunteered this information at his initial appointments. He was also currently being followed up for serological testing to monitor for re-infection at another nearby hospital.
STIs can often have oral manifestations. Dental care professionals are in a unique position because they regularly examine the oral cavity and therefore have the opportunity to recognize the oral signs of syphilis, and refer the patient accordingly. This allows for prompt treatment and prevention of the complications associated with the later stages of syphilis. However, it may be considered inappropriate by some patients to have a sexual history taken by a dental practitioner or indeed some dental care professionals may feel uncomfortable taking this history.
In this case, the patient did not appear surprised by his diagnosis, and subsequently volunteered information that he had previously been treated for syphilis. This information would have been beneficial at the initial consultation and would have raised suspicion, prompting earlier serological testing to be undertaken. This highlights the importance of taking a sexual history, including previous STI diagnoses for atypical oral presentations.
An additional point of interest is that the patient cancelled his follow-up appointment following his biopsy as his ulcer had resolved. There is a relatively narrow window when syphilitic signs present clinically, emphasizing the importance of taking a thorough history and examination and referring promptly. Clinical photographs provide a valuable record, as most oral lesions in the primary and secondary stages will spontaneously resolve.
Diagnosing syphilis can be a challenge owing to the broad range of clinical presentations. For non-specific clinical signs and symptoms, a high index of suspicion should be maintained. It is beneficial to be aware of the common oral manifestations, so syphilis can be included in the list of differential diagnoses. If suspected, a low threshold for referral is essential.
In conclusion, syphilis has many oral manifestations and it should be considered in the differential diagnosis of suspicious oral lesions. If left, the lesions will undergo spontaneous remission. Therefore, syphilis may go unnoticed and enter the latency stage, potentially resulting in the life-threatening complications of tertiary syphilis. Dental care professionals therefore play an important role in identifying cases and thus stopping the resurgence of this preventable and curable epidemic.