Article
Sir, we wish to highlight an unusual post-operative complication resulting from a submandibular and submental dental abscess, which presented to the accident and emergency department at King's College Hospital. A 49-year-old male patient presented with a three-day history of a right-sided facial swelling, arising from the lower right first and second molars (Figure 1). The patient presented with symptoms that included hoarseness of the voice and difficulty in swallowing. There was no history of trauma or illness preceding the swelling and no relevant medical history was present.

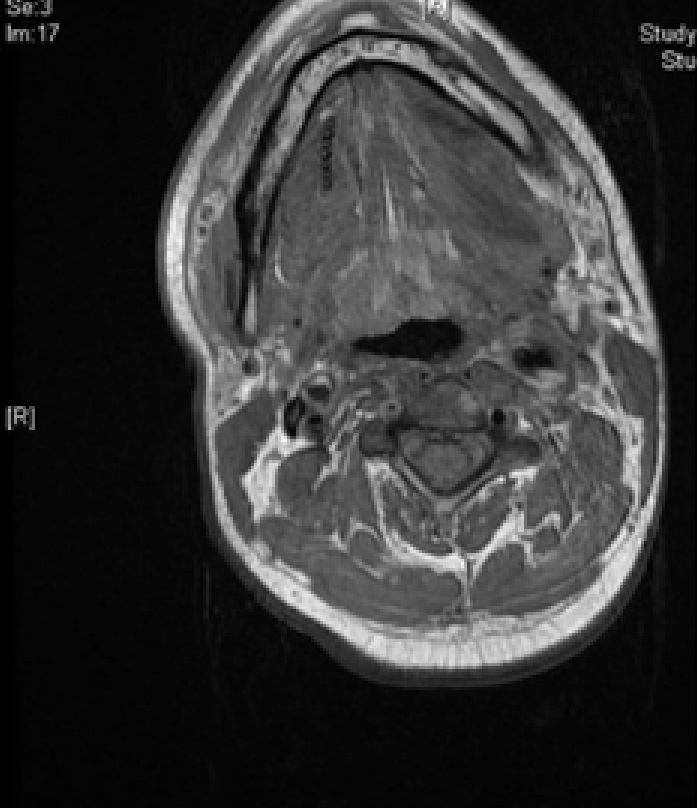
Extractions of the lower right molars and incision and drainage of the abscess were carried out under general anaesthetic. The patient remained intubated for 24 hours post-operatively due to laryngeal oedema. After extubation the patient continued to have difficulty in swallowing and also developed slurred speech. Upon further investigation, the collection had spread involving the left parapharyngeal space, requiring a return to theatre for further exploration and drainage (Figure 2). Subsequently, the patient developed bilateral hypoglossal nerve palsy necessitating a tracheostomy and PEG tube placement. He had an inability to swallow his own saliva and move the tongue.
Bilateral hypoglossal nerve palsy is an extremely rare condition. Several causes are attributed to its aetiology, such as infection, vascular injury and neuropathy.1 Cases of hypoglossal nerve palsy following tooth extraction have also been reported. In this case, the palsy may have been caused by the infected molars or as a result of surgery.2,3,4 In the following months the bilateral hypoglossal nerve palsy continued to improve.
This letter highlights the potential for post-operative complications arising from a dental abscess. This illustrates the importance of early recognition and treatment of abscesses in order to reduce such complications.

