References
The orthodontic/endodontic interface part 4
From Volume 45, Issue 11, December 2018 | Pages 1024-1031
Article

Orthodontic outcomes on the vital tooth
More patients are undergoing orthodontic treatment and mild external root resorption is a common finding.1, 2 This is usually not clinically significant with a root length reduction commonly of 1−2 mm.3 Severe root resorption in which more than one quarter of the root length is lost has been reported in 3% of orthodontic patients.4 The greatest amount of resorption is seen in the anterior maxillary region, especially the maxillary lateral incisors.5 The most significant factors affecting root resorption appear to be the duration of orthodontic treatment and the distance that teeth are moved.6
As the stimulus to this process is the orthodontic forces and these are time-limited and finite, the extent of resorption is usually minimal and healing will follow. This is not regeneration but rather reformation of the cementum and periodontal ligament on a modified and invariably blunted root surface. Nonetheless, teeth with a history of trauma or deep restorations present with other risk factors for root resorption that may not be controlled by the cessation of orthodontic forces. As such, it is sensible to take peri-apical radiographs beforehand and apply more gentle forces in these high risk cases.
Root resorption
Resorption has been defined as a condition associated with either a physiological or a pathologic loss of dentine through the continued action of osteoblasts.7 Several distinct categories of resorption occur (Table 1):
| Internal Resorption | External Resorption: Surface Resorption | External Resorption: Inflammatory Resorption | External Resorption: Replacement Resorption |
|---|---|---|---|
| Rare, but usually associated with infected/necrotic pulp | Associated with trauma or damage to cementum | Associated with injury to the periodontal ligament (PDL) | Associated with loss of vitality of the PDL |
| Resorptive process requiring vital tissue | May be transient or progressive | Communication with dentinal tubules following surface resorption | Tooth structure is replaced with alveolar bone fused to dentine |
| Clinically detectable due to discoloration of tooth | Mild, affecting small areas of root surface | Can lead to necrosis | Clinically detectable with dull percussion |
| Can be detected on plain film radiographs | Usually not detected on radiographs | Usually can be detected on plain film radiographs depending on size of lesion | Difficult to detect on plain film radiographs |
The earliest sign of replacement root resorption tends to be a dull percussion note which can be detected once 20% of the root surface is affected by replacement resorption.11 This can lead to ankylosis and commonly occurs on the buccal and palatal root surfaces, which can lead to the process not being detectable on plain film radiographs for up to a year.
Orthodontic management of root-filled teeth
There have been many conflicting reports on the impact of orthodontic tooth movement on endodontically treated teeth. Some authors have reported increased risks and rates of root resorption, whilst others have reported equal or reduced risks.12, 13, 14, 15, 16
Animal studies have often been used when researching the orthodontic tooth movement in both vital and non-vital teeth. These have shown that, in both cases, teeth moved similar distances when subjected to the same forces.17 Histologically, it was shown that root-filled teeth showed greater loss of cementum compared to vital teeth. However, more importantly, there was no significant difference in root length.
A more recent retrospective study was undertaken to investigate the radiographic findings of root resorption amongst patients undergoing orthodontic treatment who had one maxillary incisor which was root-filled. The amount of root resorption was compared to the contra-lateral vital control tooth and it was shown that there was no statistically significant difference in the amount of apical root resorption amongst vital and root-filled teeth.18
Therefore, from the available evidence, it can be concluded that there is no difference in the root resorption of endodontically treated teeth when compared to vital teeth that are subjected to the same force.
There has been little investigation into the remaining root canal filling material following external root resorption of an endodontically treated tooth. Many possibilities exist:
If the root canal treatment is adequately condensed laterally, then the resorptive process should not affect the apical seal of the tooth.
It has been outlined by the European Society of Endodontology that endodontic treatment can be considered a success one year post-obturation when there is absence of pain or swelling, no sinus tract, no loss of function and radiographic signs of a normal periodontal ligament space around the tooth.20
Treatment approach when endodontically treating teeth undergoing orthodontic treatment
There has been much debate regarding the obturation material of choice when endodontically treating teeth undergoing orthodontic treatment. The initial approach was to dress the affected tooth with non-setting calcium hydroxide during orthodontic tooth movement.21 Once orthodontic treatment was completed, the root canal(s) would subsequently be obturated with gutta percha. However, animal studies have shown that teeth obturated with gutta percha are at no increased risk of resorption during orthodontic treatment.22 Therefore, a definitively obturated tooth with an adequate coronal seal is at no increased risk of resorption compared to that dressed with calcium hydroxide during orthodontic tooth movement.
Teeth dressed with calcium hydroxide have an increased risk of fracture, with the dentine fracture resistance strength reduced by 44% 84 days after placement of the dressing.23 This evidence would further support the recommendation of completing the root canal treatment, definitively obturating the tooth and providing a coronal seal prior to commencing orthodontic tooth movement.
An exception to this recommendation would be teeth that show signs of external inflammatory resorption during treatment. Placement of a calcium hydroxide dressing for up to 12-weeks prior to obturation has been shown to have a significant difference in promoting root healing with new cementum.24
Observation period post-endodontic treatment
There is limited evidence available as to the recommended observation periods post-endodontic treatment, before commencing orthodontic tooth movement. Guidance is often based on expert opinions. Animal studies have shown that orthodontic forces applied to endodontically treated teeth delay the peri-apical healing process but do not prevent this process from occurring.25 It has been suggested that, in cases where root canal treatment has been undertaken due to pulpal necrosis secondary to caries, orthodontic tooth movement can be commenced immediately post obturation.26 Where there have been areas of extensive bone loss, orthodontic tooth movement should be delayed until there are radiographic signs of healing and a minimal interval of 6-months has been suggested. Following dental trauma, an observation period of 12 months has been suggested prior to commencing tooth movement in order to decrease the risk of ankylosis. It has been shown that even a 12-month delay cannot always stop ankylosis from occurring and thus patients should always be warned of this possibility.27
Orthodontic management and dental trauma during treatment
If a patient suffers dental trauma undertaking orthodontic treatment, some protection may be offered by the stabilizing effect of the orthodontic appliance itself. However, the management is dependent on the type and severity of the injury.
Types of injuries
Intrusion injuries
Intrusion injuries can often be difficult to manage due to effects on the pulpal tissues, periodontal ligament and alveolar bone. They account for 1.7% of traumatic injuries.28 Mild intrusion injuries can often lead to spontaneous regeneration of the periodontal ligament. Thus for mild intrusion injuries in teeth with closed apices, it has been recommended to allow a 2-week period for spontaneous re-eruption.29 Moderate and severe injuries require interdisciplinary management. With the increased severity of the intrusion injury, there is a greater risk of pulpal necrosis and the possibility of replacement resorption occurring, as described above. There are further risks including loss of alveolar bone and infraocclusion.
It has been recommended by the Dental Trauma Guide that orthodontic repositioning may be appropriate when a tooth has been intruded by 3-7 mm. Any intrusion greater than this would indicate surgical repositioning. Simply put, the tooth may not even be visible to bond a bracket to! It may be necessary to apply gentle luxation forces prior to orthodontic repositioning in cases where the tooth has become locked in the alveolar bone. This should be promptly followed by extirpation and root canal treatment to prevent inflammatory resorption from occurring. Endodontic treatment should be initiated immediately on all teeth with avulsion or intrusion injuries. This is due to the higher prevalence of root resorption reported in severe intrusion injuries in teeth with closed apices.30
Animal studies have shown that inducing light occlusal stimuli can promote periodontal healing and prevent replacement resorption from occurring. In a study undertaken on mice, it was shown that, with heavier occlusal stimuli, there was an increased risk of root resorption.31 This indicates that placement of a light aligning orthodontic wire to reposition teeth may reduce the risks of ankylosis and root resorption following an intrusion injury. An example of management of intrusion injuries is demonstrated in Case 2.
Extrusion injuries
Extrusion injuries are less common. Mostly, these can be treated by cleaning the exposed root surface with saline prior to repositioning the tooth with gentle axial pressure. This is followed by stabilizing the tooth with a flexible splint for 2 weeks.32 However, in cases where there is a large extrusive displacement, the prognosis of the tooth is reduced. Orthodontic alignment at an early stage may be required to align the tooth prior to any root resorption occurring. This is followed by endodontic treatment to prevent internal resorption. This process is highlighted in Case 3.
Root fractures
Root fractures have an incidence of 0.5−7%.33 They present as complete or incomplete, and horizontal or vertical fractures. In the majority of root fractures the apical fragment of tooth remains vital. The aim of treatment is to attempt to preserve the vitality of the coronal fragment of the tooth and an extended period of splinting is required to promote a hard tissue of dental callus between the two fragments. If any orthodontic tooth movement is required, it is essential that the presence of this hard tissue barrier is radiographically confirmed.34 If, however, the tooth has healed with a connective tissue barrier between the fragments, the tooth has to be considered as having a short root. Provisions need to be undertaken to prevent any further apical root resorption and thus light orthodontic forces are advocated. When there are signs of granulation tissue between the two fragments, following necrosis of the coronal fragment, then endodontic treatment is required prior to orthodontic tooth movement. An observation period of 1−2 years has been suggested prior to orthodontic tooth movement following root fracture.27
Avulsions
Avulsion injuries account for 1−6% of all dental trauma injuries.8 It is well reported that the outcome of such injuries is poor unless they are stored in a physiologic medium, such as milk or saliva, and subsequently re-implanted immediately. Thus avulsion injuries often lead to pulpal necrosis and have a poor long-term prognosis. In cases of delayed re-implantation, ankylosis is unavoidable. Removal of necrotic pulp and endodontic treatment will minimize the risk of root resorption and ankylosis following re-implantation. Thus avulsed teeth with a closed apex should be treated endodontically and be kept under review to ensure that there is no subsequent resorption prior to attempting any orthodontic tooth movement.
Ankylosis
As outlined in Table 1, loss of vitality of the periodontal ligament due to trauma can lead to replacement resorption and ankylosis of a tooth. Ankylosed teeth cannot be moved with orthodontic appliances. This can provide a range of options to manage the tooth, including accepting the position and allowing restorative correction at the end of orthodontic treatment or loss of the ankylosed unit. Ankylosed teeth can often be used to reinforce anchorage during orthodontic treatment. There have been many case reports involving luxation of the ankylosed tooth and subsequent tooth movement has been successful. Luxation of the ankylosed tooth can lead to pulpal necrosis and thus endodontic treatment is required to remove necrotic pulpal tissue prior to commencing orthodontic tooth movement.
Case studies
Three short case studies have been summarized, highlighting patients requiring endodontic intervention post-orthodontic treatment.
Case 1
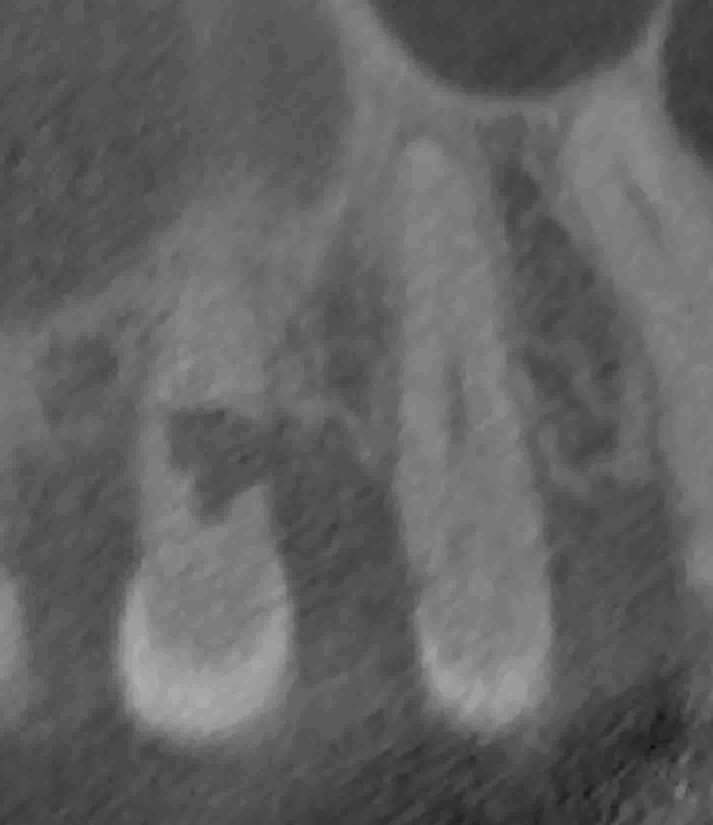
This case demonstrates a 16-year-old female who presented with inflammatory root resorption affecting UR3 following completion of orthodontic treatment with fixed appliances. As discussed above, external root resorption is a known risk of orthodontic treatment. Although it is not the primary focus of this paper to discuss the endodontic management of resorption, a brief overview of treatment can be seen in Figure 1. The extent of the lesion can be seen in the CBCT image in Figure 1a. Endodontic management was undertaken using techniques outlined in previous literature.35 To summarize, initially this involved conventional obturation with gutta percha (Figure 1b). This was followed by surgical access of the lesion, with curettage to allow direct removal of osteoclastic cells (Figure 1c). Finally, a definitive restoration with Biodentine® (Septodont, Maidstone, UK) was placed over the affected lesion (Figure 1d). This treatment approach stabilized the resorptive lesion and, on follow-up, no further resorption was noted.
Case 2
A 14-year-old patient was referred by his GDP for an orthodontic assessment, following trauma to all upper incisor teeth. UR1 was avulsed and re-implanted at a local hospital. UR1 and UL2 were also intruded relative to UL1 (Figure 2). An OPG and periapical radiographs were taken (Figure 2c–e) which showed radiographic signs of internal and external root resorption affecting UL1; the long-term prognosis of this tooth was deemed to be very poor. The patient was informed regarding the poor prognosis of all upper incisor teeth and, in particular, about the high possibility of ankylosis of UR1 and UL2. In addition, he also presented with large carious lesions in all his first permanent molars.

Orthodontic treatment was outlined with upper and lower fixed appliances in an attempt to align the intruded upper incisors. This would also help to determine the possibility of ankylosis of the affected teeth. If the teeth were to respond to orthodontic alignment, the patient would need possible endodontic treatment of UR1 and UL2 to prevent any internal resorption in the long term. The patient was warned about the possibility of implant replacement of all upper incisors at the end of orthodontic treatment.
End of treatment views (Figures 3a and b) show all the upper incisors were aligned with orthodontic treatment. However, the periapical radiographs taken during orthodontic treatment (Figures 3c and d) show all upper incisors had suffered from varying degrees of root resorption, with UL1 and UR1 roots indicating a poor long-term prognosis. After a joint consultation with the restorative dentist, a treatment plan involving implant replacement of UR1 and UL1 and endodontic treatment on UR2 and UL2 was formulated.
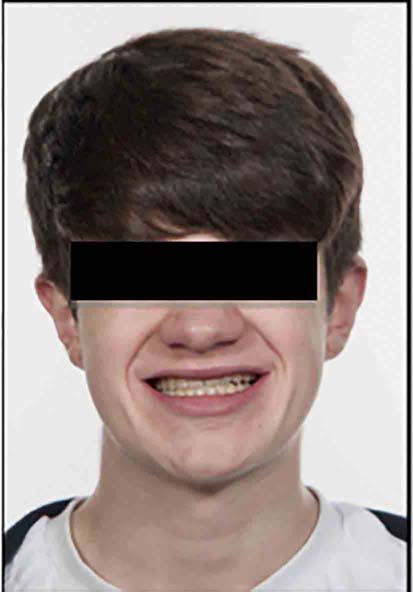
This case demonstrates the high risk of inflammatory and replacement resorption following intrusion injuries and the difficulties in managing such complications. Furthermore, it highlights the interdisciplinary management required between orthodontics, endodontics and restorative dentistry when aiming to achieve optimal aesthetics and function.
Case 3
A 17-year-old patient presented following trauma to UL1. The patient was in active orthodontic alignment treatment with upper and lower fixed appliances. UL1 was significantly extruded (Figure 4a). The tooth was gently intruded back into its correct position. It can be seen from the peri-apical radiograph (Figure 4b) taken after intrusion of the tooth that there was apical root resorption in the region of 2−3 mm. Towards the end of orthodontic treatment, there were clinical signs of pulpal necrosis and thus, to prevent any further root resorption, the tooth was treated endodontically and obturated with GP following debond of the orthodontic appliances (Figure 4c). This case highlights the risks of extrusion injuries and the combined need for orthodontic intrusion and endodontic treatment to manage such complications.

Conclusion
The interrelations of pulpal health, osteoclastic activity and orthodontic treatment are complex and poorly understood. All patients should be consented to some reduction in root length following orthodontic treatment but some require greater care and observation. When disease is present, endodontic treatment should be undertaken in advance of orthodontic treatment and these teeth monitored closely for healing and signs of resorption. Practitioners should, however, feel confident that endodontic treatment itself should have no impact on the outcomes of the orthodontic treatment, Cases presenting with trauma mid-orthodontic treatment should be managed more conservatively; orthodontic treatment should be stopped and all pathology controlled before recommencing care.

