References
The options for a tooth that requires root canal treatment
From Volume 45, Issue 3, March 2018 | Pages 182-195
Article

In this age of increasing emphasis on body image and youthful appearance, the perfect white smile is fast becoming a norm by which people are judged.1,2,3 This may influence the retention of natural teeth, however, there is a possibility that the natural tooth is being replaced when complex restorative dental treatment is required, possibly in order to achieve the ideal appearance more easily. When the public and some of the profession consider implants a panacea, what are the options for a tooth that requires root canal treatment? Is there a place for providing dentistry to retain a natural tooth?
The effect of tooth loss on a person's quality of life has been investigated in several studies,4,5,6,7,89 with a general consensus that tooth loss had a negative impact on quality of life, and patients citing reduction in chewing ability following the loss of teeth as a cause. However, the prospect of tooth loss is less dramatic in recent times because of the variety of options available for filling the space or spaces. With the reported success rates of implants, there is a possible departure towards replacing teeth with implants if complex restorative work is required to maintain the tooth in situ. A number of articles have described the virtues of maintaining a natural tooth in relation to accepting a space or providing a prosthetic replacement.10,11,1213,14,15,16
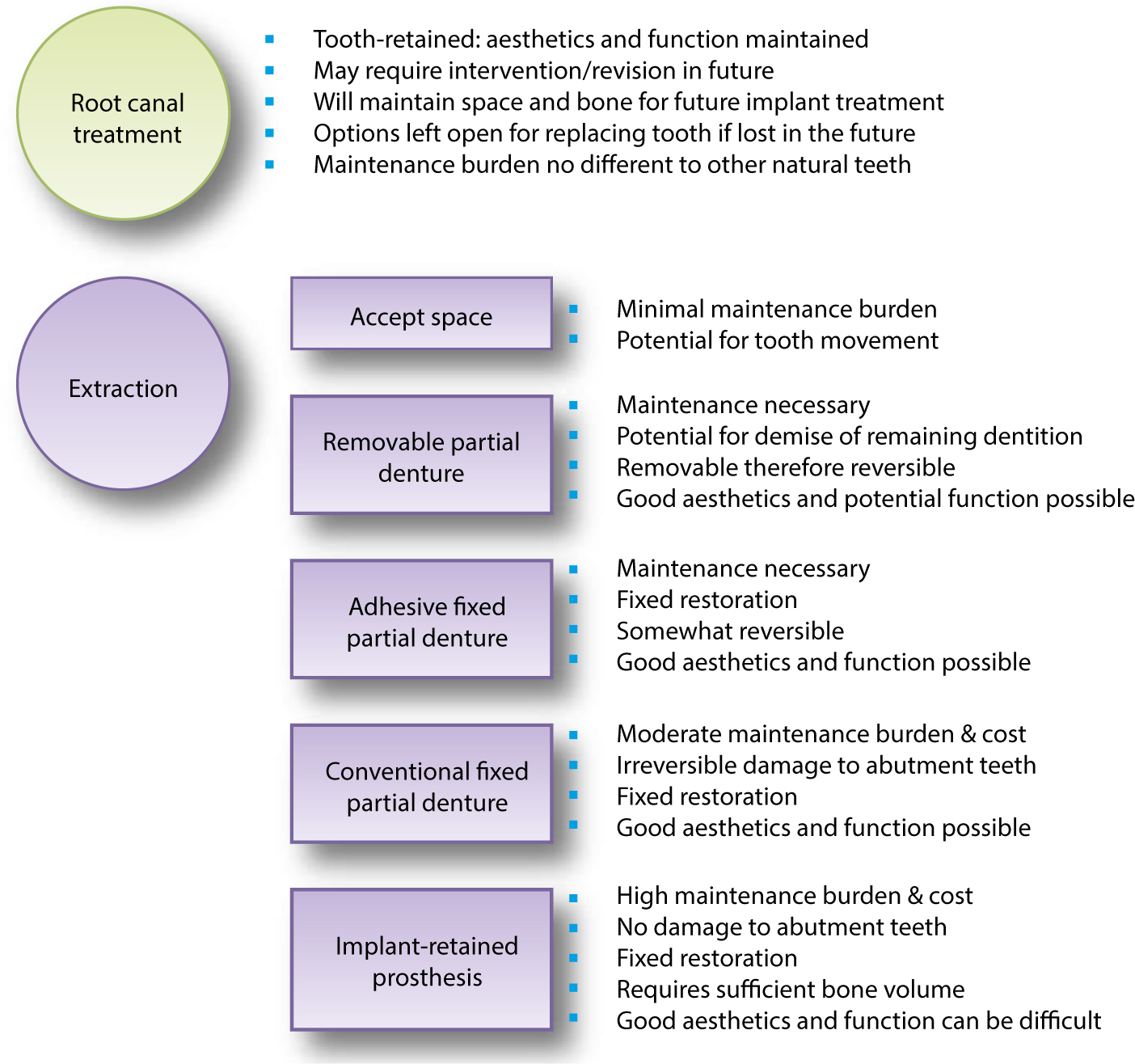
This article summarizes the available evidence for root canal treatment and maintenance of teeth, and potential options for restoring a space when a tooth is lost. The virtues of maintaining teeth where possible, even with complex restorative treatment, especially root canal treatment, is discussed. The options for spaces resulting from tooth loss include accepting the space, removable and fixed prosthodontics (both tooth- and implant-supported), and range from the least invasive (root canal treatment and maintenance of a tooth) to potentially the most invasive (extraction and replacement with conventional fixed prosthodontics or implants). This article should inform decision-making discussion with patients, especially with regard to maintenance/failure of teeth and restorations in the long term.
Root canal treatment and maintenance of the natural tooth
Root canal treatment and maintenance of the natural tooth has high success rates17,18,19 and high survival rates.14, 20,21,22,23,24,25,26 The natural tooth will maintain alveolar bone and soft tissue contours,27,28,29 enabling future restoration of the space using dental implants. The main advantage of root canal treatment was reported as the ability to manage non-healing, resulting in tooth retention with fewer interventions than with implant-supported prostheses.30 Root canal treatment can avoid extractions in medically compromised patients, such as those who have undergone radiotherapy to the head and neck, those taking bisphosphonates, or who have blood dyscrasias where special precautions or avoiding extraction may be favoured.31
However, root canal treatment is a lengthy and complex procedure, which is only possible when there is enough remaining tooth structure for restoration after root canal treatment.32 A minimum number of radiographs are required33 and can take more than one appointment to complete, depending on complexity. The cost implications to the dentist, such as time and the cost of single use root canal instruments,34 are often reflected in the fee presented to the patient. The cost to the patient also includes the purchasing of a definitive restoration for the tooth after root canal treatment. Long-term review is usually a minimal intervention, unless symptoms arise and patient-related outcomes are similar with root canal treated teeth and implant-supported single crowns.35
Insurance companies and dental public health bodies are inclined to present only the retention or survival of the tooth following root canal treatment.2021,22,23,24,25,36 These studies do not address the quality of treatment or the clinical signs and symptoms, but only assess the presence or absence of further treatment or extraction of the tooth as the end point. They do not give any indication of the clinical or radiographic status of the tooth (Table 1).
| Study | Country and type of service evaluated | Years data collected | No of teeth included | Survival rates | |
|---|---|---|---|---|---|
| Lazarski et al, 200120 | USA Private practice of generalists & specialists | 1993–1998 | 109,542 | 94.4% at 3.5 years | |
| Salehrabi & Rotstein 2004,21 | USA Private practice of generalists & endodontists | 1995–2002 | 1,462,936 | 97% at 8 years | |
| Chen et al 2007,22 | Taiwan Private practice | 1998 | 1,557,547 | 91.1%–95.4% at 5 years | |
| Lumley et al, 200823 | UK (NHS) General dental practice | 1991–2001 | 30,843 | 74% at 10 years | |
| Tickle et al, 200824 | UK (NHS) General dental practice | 1998–2003 | 174 | 90.8% at 5 years | |
| Ng et al, 201025 | Mix of countries and settings (Review – pooled success) | (Meta-analysis of 14 studies) | 86% (95%CI, 75%–98%) at 2–3 years |
The reported survival of root canal treated teeth include 8-year survival of 97% in the United States,21 5-year retention rates of 91.1%–95.4% in Taiwan,22 and 3.5-year survival of 94.44% in the United States.20 In the UK, there have been similar studies, with 10-year survival rates of 74% in NHS General Dental Practice.23 These studies have not examined the quality of treatment provided, or the state of the treated tooth in the mouth following treatment. The absence of further treatment of the tooth alone was deemed success. When success was assessed in the UK, outcome of root canal treatment performed in the Royal Air Force had a significantly higher success rate of 85%, using radiographic and clinical signs to define success and failure, with the review period grouped into <3 years and >3 years since root treatment.37
A retrospective cohort study of patients (n = 174) treated in NHS general practice (n = 12) in the UK, on the survival of mandibular first permanent molars that were root canal-treated within the state-funded National Health Service, also assessed the quality of the root fillings by the radiographic appearance of the root filling.24 Root canal treatments were assessed radiographically by an endodontist and deemed ‘optimal’ or ‘sub-optimal’ (in accordance with the Consensus report of the European Society of Endodontology on quality guidelines for root canal treatment38), or the radiograph was classed as missing/unreadable. Training, calibration and reliability of this examiner was not reported. Healing as seen radiographically was not assessed. Failure was defined as extraction, replacement of the root filling or periradicular surgery performed on the tooth. The review period varied up to 7.7 years with <10% failure rate. Similar failure rates were seen in ‘optimally filled’, ‘sub-optimally filled’ and ‘unreadable/missing radiographs’ groups. The majority of the failures were within the first year following treatment. Root canal treated teeth restored with crowns had a lower risk of failure than those restored with intra-coronal restorations. It was assumed that these ‘successful’ teeth were free of signs and symptoms of infection and that is why they were not extracted, re-treated or surgically treated. This paper was considered controversial as it implied an acceptance of ‘sub-optimal’ root fillings, as survival rates were still high as long as prompt definitive restoration of the tooth is carried out.39,40
Recent detailed and comprehensive systematic reviews by Ng et al17,18,41 attempted to collate the various outcome findings. Ng et al examined the effects of study characteristics on probability of success of primary root canal treatment.41 They used the presence or absence of clinical signs and symptoms as well as ‘strict’ (absence of apical radiolucency at recall) and ‘loose’ (reduction in size of apical radiolucency at recall) criteria for radiographic interpretation in describing success. Clinically, root canal treated teeth should be compared with what is described to be normal, ie the lack of pain, swelling, sinus tracts, tenderness to palpation and percussion, tenderness in function and mobility.11,42
Root canal treatment is described as ‘primary root canal treatment’ if it is the first time root canal treatment is provided for a tooth. If the root canal treatment is redone or revised, it is termed ‘secondary root canal treatment’. Ng et al investigated the influence of clinical factors on the probability of success of primary root canal treatment.17 The review set out to examine the influence of numerous patient and operator factors. Four conditions were found to improve the outcome of primary root canal treatment significantly: pre-operative absence of periapical radiolucency, root filling with no voids, root fillings extending to two millimetres from the radiographic apex and remaining within the root canal system, and satisfactory coronal seal. In this meta-analysis,17 which used both ‘strict’ and ‘loose’ criteria, estimated pooled success rates of primary root canal treatment was 74.7% (95% CI, 69.8%–79.5%) under ‘strict’ criteria and 85.2% (95%CI, 82.2%–88.3%) under ‘loose’ criteria, during a review period of six months to 30 years. The idea that, since technology and materials have improved over time, the success rates should also improve, was explored, but no supportive evidence was seen. It is thought that this lack of increase in success rate is as a result of ‘more adventurous case selection fuelled by confidence in better skills and outcomes’.41
Ng et al also carried out a similar systematic review on the outcome of secondary root canal treatment with a pooled weighted success rate based on ‘strict’ criteria of 76.7% (95% CI, 73.6%–89.6%) and that based on ‘loose’ criteria of 77.2% (95% CI, 61.1%–88.1%).18 The conditions for success were similar to those for primary root canal treatment. The success rates from studies carried out in the 2000s were the lowest whether ‘strict’ or ‘loose’ criteria were used. Treatment carried out by specialists surprisingly had the lowest estimates of success regardless of the use of ‘strict’ or ‘loose’ criteria, which is thought to be as a result of specialists possibly managing more complex cases. The qualifications of the operator had no significant influence on the outcome of secondary root canal treatment. The weighted pooled success rate for teeth without periapical lesions pre-operatively was 28% higher than for those with pre-operative periapical lesions. The systematic reviews on outcomes of primary and secondary root canal treatment17,18 both suggest that the size of pre-operative periapical lesions are not relevant as long as enough time is given for healing. The weighted pooled success rate for teeth without pre-operative perforation was 32% higher than that for teeth with pre-operative perforation. Root fillings extended beyond the apex had the lowest success rate regardless of the presence or absence of a periapical lesion. Due to lack of adequate data,17,18 a meta-analysis relating to many related aspects of root canal treatment was not performed. These aspects included the effect of canal obturation, the use of rubber dam, apical instrumentation, size of apical preparation, canal taper, separation of instrument during root canal treatment, medicament used, root-filling techniques and materials, quality of root-filling and number of treatment visits on the outcome of root canal treatment. The summary of success rates from the two systematic reviews is shown in Table 2.
| Success rate of primary root canal treatment, ie root canal treatment done for the first time in a tooth (Ng et al, 2008a)17 | Success rate of secondary root canal treatment, ie revision root canal treatment (Ng et al, 2008b)18 | |
| Using ‘strict’ criteria | 74.7% (95% CI, 69.8%–79.5%) | 76.7% (95% CI, 73.6%–89.6%) |
| Using ‘loose’ criteria | 85.2% (95% CI, 82.2%–88.3%) | 77.2% (95% CI, 61.1%–88.1%) |
Cheung and Chan43 investigated the survival of primary root canal treatment carried out by undergraduates and postgraduates in a dental hospital in Hong Kong using a retrospective longitudinal design. They found a 50% success rate at 9.2 years, with the survival of root-filled teeth being significantly influenced by the tooth type (maxillary and mandibular molar teeth faired worse than anterior and premolar teeth), pre-operative periapical status (better if there was no evidence of periradicular pathology prior to treatment) and the type of coronal restoration (teeth with crowns survived significantly longer than those with intra-coronal plastic restorations only.43,44
Ng et al carried out a systematic review on tooth survival following non-surgical root canal treatment.25 Although 14 studies were included (10 retrospective and 4 prospective), a direct comparison was hindered by the heterogeneity of the studies. The pooled percentage of reported tooth survival over 2–3 years was 86% (95% CI, 75%–98%), over 4–5 years was 93% (95% CI, 92%–94%) and over 8–10 years was 87% (95% CI, 82%–92%). In descending order of influence, the factors seen to be effecting survival were: a crown restoration after root canal treatment, the tooth having both the mesial and distal proximal contacts, tooth not functioning as an abutment for removable or fixed prostheses and tooth type (non-molar teeth). Similar findings have been supported by other publications.36,45,46 The most recent publications from Ng et al relate to the findings from a prospective study of the factors affecting outcomes of non-surgical root canal treatment19,26 (Table 3).
| Study | Conditions found to improve periapical healing |
|---|---|
| Success rate of primary root canal treatment 83% (95% CI, 81%–85%) (Ng et al, 2011a)19 |
|
| Success rate of secondary root canal treatment 80% (95% CI, 78%–82%) (Ng et al., 2011b)26 |
In terms of root canal outcome in primary care versus secondary in the UK, the success rate of primary root canal treatment in one secondary care unit in the UK was 83% (95% CI, 81%–85%) and that for secondary root canal treatment was 80% (95% CI, 78%–82%).19 The 4-year cumulative tooth survival rates for primary root canal treatment was 95.4%(95% CI, 93.6%–96.8%) and that for secondary root canal treatment was 95.3% (95% CI, 93.6%–96.5%).26 For comparison, no outcome data are available for the success of root canal treatments performed in primary dental care in the UK. The survival of root canal treated teeth has been estimated at 90.8% at five years24 and 74% at 10 years.23
Since the introduction of UDAs in April 2006,47 it is no longer possible to calculate the numbers of root canal treatments carried out in the NHS as this banding system groups together types of treatment rather than recording individual items of treatment.
Root canal treatment carried out by postgraduate students and specialists had the highest weighted pooled success rate irrespective of strict or loose criteria being used to measure success.41 It has been said that educational background of the operator may have an impact on dentists' decision-making or case selection.48,49 Other studies have suggested that the background or experience of the operator can have an influence on the technical outcome of endodontic procedures.50,51 A clinical study by Alley et al showed endodontic treatments by specialists were significantly more successful than those carried out by GDPs.52 The difference in outcome between generalists and root canal specialists is less clear in some studies. For example, of 29,895 non-surgical root canal treatments performed by non-endodontists, 1,390 (4.65%) required subsequent retreatment or periradicular surgery. In comparison, of 14,718 non-surgical endodontic treatments carried out by endodontists, 597 (4.06%) cases required subsequent retreatment or periradicular surgery.20 Ng et al highlight the lack of tools or methodology to objectively quantify operator skills, the need to balance between technical skill and ‘understanding of the problem and the motivation and integrity with which the procedure is performed’.41
The assumption is that a well-condensed and well-extended root-filling, as seen radiographically, may mean a job well done by a conscientious clinician, with appropriate isolation, access and irrigation. However, it is not appropriate always to make this assumption. Published data suggest that a large percentage of general dental practitioners use endodontic techniques with no evidence of clinical effectiveness. The survival rate of root-filled teeth if rubber dam is used during treatment has been shown to be statistically significantly higher than if rubber dam was not used,53 and yet rubber dam was used by between 0.9% and 47% of dentists surveyed using questionnaires.54,55,56,57,58,59,60,61,62,63,64,65,66 Electronic Apex Locators were being used by between 2.7% and 70% of dentists surveyed.56,57,60,61,62,63,67,68,69 Reported rates of sodium hypochlorite use for irrigation is between 33% and 95% of responding dentists.54,55,57,58,59,60,61,62,63,70,71
A longitudinal study by Dugas et al reported on the Quality of Life (QoL) and satisfaction outcomes of root canal treatment on two Canadian populations aged 25–40 years in two different dental schools.72 Seventeen questions chosen from Oral Health Impact Profile (OHIP) 49 were used with a five-point Likert scale. The subjects acted as their own controls by reporting how the disease pre- and post-root canal treatment affected the quality of life. In this study population, almost all of the subjects reported pain prior to root canal treatment, but less than 50% reported a form of functional limitation.
Subjects who had experienced ‘painful aching’ prior to root canal treatment reported the highest rate of improvement and those who had difficulty with ‘pronouncing words’ reported the lowest rate of improvement. The logistic regression model for ‘predicting improvement in the ability to perform usual jobs’ in this study predicted that the subjects are five times more likely to perceive improvement if the subjects had a high school education.
Improvement in ‘physical pain’ and ‘social disability’ were significantly higher if treated by an endodontist than a generalist. The logistic regression model for ‘predicting improvement in the ability to perform ‘usual jobs’ in this study predicted that the subjects are seven times as likely to perceive improvement in the ability to perform ‘usual jobs’ when the treatment was provided by an endodontist than a generalist. The logistic regression model for ‘predicting improvement in temperature sensitivity’ showed that patients were 2.7 times more likely to perceive an improvement if the treatment was completed by an endodontist.72 Hamasha and Hatiwsh73 used the same questionnaire used by Dugas et al72 and found no significant differences in the improvement of oral health between patients treated by undergraduates, postgraduates and specialists in some domains and improvements in favour of specialists in other domains. For example, satisfaction was higher when treated by a specialist in relation to ‘time involved, intra-operative pain, pleasantness and general satisfaction’ when compared to treatment by undergraduate students. However, there was least satisfaction with the treatment cost when compared to treatment by postgraduate or undergraduate students.73
As long as there is sufficient tooth structure to restore the tooth, it is possible to revise the root canal treatment if there is a flare up years later, as it is accepted that no material provides a perfect seal for indefinite periods of time. The long-term maintenance of the tooth will be no different to maintenance of the rest of the dentition, with emphasis on prevention of caries and periodontal disease. Subjects who had an anterior tooth root canal treated rather than extracted reported the peak satisfaction of 100%.72 Gatten et al35 compared QoL relating to patients with endodontically-treated teeth with implant treatment. Both cohorts reported similar QoL and satisfaction; however, patients recommended preserving the natural dentition wherever possible.35 Where it is not possible to restore a tooth, extraction and one of the following options may be more appropriate.
Accepting a space
The simplest option is to accept the space left by the extraction of a tooth, as no further treatment is required. This is somewhat reversible, as the options for filling the space are still potentially available. When posterior teeth are lost, function has been said to be adequate as long as there are four opposing posterior units (one molar tooth being equivalent to two premolar units) and this has been termed a shortened dental arch.74 Although dated, this is considered a seminal study, which assessed the oral function of 118 patients attending a dental school in Nijmegen (Netherlands), grouped into six classes according to the degree and distribution of contacting posterior units. Twenty four percent of subjects possessed a complete dentition and 82% of patients were functioning with a shortened dental arch for more than 5 years. The largest number of subjects was in the fully dentate group, with an even distribution in the other five groups. Oral function was measured using a ‘chewing test’, where light-absorbing materials were released from raw carrots during chewing. The number of chewing strokes and patient complaints with oral function were recorded. A shortened dental arch was not shown to lead to craniomandibular dysfunction or oral discomfort.75,76,77 However, with decreasing number of occluding units, the chewing strokes needed for swallowing increased.74,78
The drifting of adjacent teeth and overeruption of opposing teeth leading to loss of inter-occlusal or restorative space is a possibility, although the movement is largely clinically insignificant in periodontally healthy adult patients, and long-term stability is possible.79,80,81,82,83,84,85 Some studies have found that the movement of unopposed teeth was more than 2 mm in only 24% of subjects81 and more than 3 mm in only 6% of subjects.82 Occlusal collapse was not seen in those with shortened dental arches.83 While not randomized controlled trials, these studies compare groups with shortened dental arches with control groups to measure clinically important parameters.
Accepting a space may not be preferred to saving a tooth of strategic importance.86 Additionally, the loss of a tooth may lead to further alveolar bone loss.87,88 In the upper jaw, a shortened dental arch was viewed negatively due to aesthetics, therefore accepting a space is unlikely to be possible in the anterior zone.74,89 The long-term maintenance of a space may be the easiest option from a dental point of view, however, the psychological impact of having a space in the mouth has been recognized for quite some time, with some reports of patients likening the distress of a space left by a missing tooth being as severe as the distress to one's wellbeing when having ‘trouble with relatives’.90 If maintaining a space is unacceptable, there are options for removable prostheses (dentures) and fixed prostheses (bridges or implants).
Removable partial dentures
The partial denture is, in most cases, the next least destructive alternative to accepting a space. The advantages of partial dentures include restoring of appearance, mastication and function, and the disadvantages include potential damage to hard and soft tissues.91,92 This, however, may not be ideal in patients with periodontal disease or recurrent carious lesions as poor oral hygiene and plaque trapping around the removable prosthesis may lead to adverse consequences for the remaining dentition.93,94 Removable prostheses are a largely reversible method of restoring spaces, although there is potential for damage to abutment teeth if excellent oral health is not adhered to. Long-term review and maintenance is needed for prevention of further dental disease of the remaining dentition, with replacement of the prosthesis with changing anatomy as required. With the ageing population, dentures have the advantage of being removed and no longer used, should abutment teeth start to deteriorate or if it becomes difficult to maintain optimal oral hygiene.
Denture construction is time consuming and may take four to six visits to deliver with associated laboratory costs. Long-term maintenance is likely to include caries prevention and maintenance of periodontal stability, as well as replacement of the prosthesis. Patients may encounter social issues with wearing a removable appliance, and fail to internalize (psychologically accept) a removable appliance, therefore choosing not to wear removable appliances, especially if only posterior teeth are missing.95,96,97,98,99 It should be noted that, while healing after extraction occurs, there is possible need for temporary wear of an immediate denture, even if the definitive restoration is likely to be a bridge or implant-retained prosthesis.
No significant differences have been found in patient-related outcomes with provision of a removable denture and acceptance of a shortened dental arch in a pilot multi-centre, randomized controlled trial in 14 dental schools in Germany including only 34 patients.100
Conventional and adhesive fixed partial dentures
Full preparation and adhesive fixed prostheses include cantilevered and fixed-fixed designs of bridges using natural teeth as abutments to restore spaces, with full or minimal preparation of abutment teeth. Bridges are well tolerated by patients.101,102,103,104 These studies utilized self-completed patient questionnaires prior to and after providing prostheses of conventional and resin-retained designs, mainly in dental hospital settings. Sample sizes varied between 33 and 192 patients. These were usually cross-sectional studies and not randomized controlled trials. Some used an OHIP questionnaire101,102 and some used other non-validated questionnaires.103,104
For conventional bridgework, there is a requirement for tooth preparation, potential for de-cementation of restorations, and the need for replacement of restorations.105 Results of a cross-sectional study of 77 teeth, that were vital before bridge placement, showed the long-term damage to abutment teeth has been approximated at 30% losing vitality at 10 years and 35% at 15 years after placement of various fixed-fixed conventional bridge designs between 1981 and 1989 in a dental school in Hong Kong, reviewed at 187 +/- 23 months.106 It was not clear who carried out the clinical examination, but the radiographic examination was carried out by two pre-calibrated independent examiners with inter-examiner Kappa scores of 0.79. The study was not ideal as there was reliance on accurate record-keeping prior to treatment. Some patients who failed to attend a review were questioned by telephone rather than clinically examined, with the limitations of assessing pulp vitality clinically and radiographically while restored with bridges. However, there are no better studies, especially from the UK.
A minimum of two appointments is needed for construction of the definitive prosthesis, with an interim temporary restoration. Again, laboratory costs with long-term maintenance and replacement costs need consideration. A meta-analysis of data from a systematic review of the literature (19 studies of prospective and retrospective designs, with clinical examination at least at 5-year follow-up) revealed that conventional fixed-fixed bridges have a 10-year probability of survival of 89% and 10-year probability of success of 71%.107 A meta-analysis of a systematic review of cantilevered bridges (13 studies with a minimum follow-up time of 5 years and with clinical examination at follow-up) had a reported survival of 82% and success rate of 63% at 10 years, with the most common cause of complications being loss of pulp vitality of the abutment tooth.108 In these studies, various bridge designs have been combined, however, details of each study were available within the systematic reviews.
For adhesive bridgework, in which the tooth preparation is minimal or not needed,109,110 there is potential for de-cementation. The reported median survival for cantilever designs is 9.8 years, for fixed-fixed designs is 7.8 years.109 In no-preparation cantilever designs the abutment tooth is left unharmed even if the bridge fails. Djemal et al, in a cross-sectional study, assessed 832 restorations in 593 patients in a postgraduate dental institute setting.109 The technique, operator, materials and bridge designs were not controlled for. Where patients did not attend follow-up, the patient or general dental practitioner caring for the patient was contacted to ascertain if the restoration was still in service. The restorations were assessed by three of the authors with no mention of calibration, training or inter/intra-examiner reliability. A third of restorations were placed in patients with hypodontia (missing teeth), who usually also have small potential abutment teeth. Despite the heterogeneity of the sample, details for each design of bridge can be extracted from the publication. Other studies have reported a 65% survival at 10 years, where all designs of resin-retained bridges were pooled in a systematic review of retrospective and prospective cohort studies with a minimal follow-up time of 5 years.111
Seventeen studies reporting 16 different cohorts were included for meta-analysis, the oldest of which was carried out in 1991. The studies were heterogeneous, with a variety of bridge designs, operators, settings (mostly universities or specialist clinics) and materials being included. Many studies were excluded due to not meeting the minimum requirement of 5-year follow-up. The most recent publication still reports on patients treated between 1994 and 2001, where the outcome of 771 resin-retained bridges performed at a dental school were reported to have 80% survival rate at 10 years.110 Bridge design and materials were standardized, operators were various and the follow-up examinations were carried out by one of the authors without mention of training or intra-examiner reliability.
Patient perceptions of resin-retained bridgework are limited, with published studies comparing patients who have undergone restoration of spaces with those who have not yet completed treatment.112
Implant-supported prostheses
The alternative fixed option is implant-supported prostheses to restore spaces. There is a need for a surgical phase, with possible grafting procedures if there is a lack of bone or appropriate soft tissue,113 with good survival rates reported in a systematic review of the literature involving 39 studies including three randomized controlled trials.114 Complication rates and failure of implant have been reported as higher in smokers and those prone to periodontal disease, without professional maintenance,115 as well as those suffering from diabetes, those having undergone radiation therapy to the head and neck and postmenopausal oestrogen therapy.116 There may be difficulty with achieving ideal aesthetics in the anterior region, and there may be potential risk of damage to other structures (roots of adjacent teeth, antrum and inferior dental, lingual and mental nerves), such that implant therapy may not always be possible.117 There is a need for long-term maintenance of implant-supported prostheses, as biological and technical complications may occur.105,115,118,119,120,122 Some studies have reported similar failure rates for both root canal treated teeth and implant-retained prosthesis, however, intervention is required more often for implant-related prosthesis to achieve survival when compared to root canal treated teeth.13,30,123
The reported survival rate at 10 years for implant-supported fixed partial dentures is 87%; that for implant-supported single crowns in 98%.124 The economic costs are higher than that of root canal treatment and removable prostheses; however comparable or lower than that for tooth-supported conventional prostheses in the long term.14 Therefore, it may be prudent to consider the retention of natural teeth for as long as possible, to ensure that the lifetime of restorations to replace missing teeth start later, reducing the number of times these restorations need to be serviced or replaced in a patient's lifetime.
It is also noteworthy that specialists often provide implants and general dental practitioners most often provide root canal treatment.125 Survival rates of implants provided by inexperienced practitioners have been reported as 20% lower when compared to that provided by implant specialists.126,127,128 In comparison, root canal treatment provided by specialists has a higher success rate than that provided by generalists (98.1% and 89.7%, respectively) at five years after treatment.129
Studies have reported no significant difference in the survival rates of root-filled teeth and of implant-supported single crowns.13,30,123,130,131 Therefore, conventional root canal treatment or retreatment is the clinical procedure of choice whenever a tooth is restorable but suffers endodontic pathology. Morris et al stated that the difficulty in making this comparison between implants and natural teeth is that implants are measured often in terms of survival (implant is still present despite associated problems), whereas root-filled teeth are measured in terms of success (the tooth is present with signs of clinical and radiographic healing).131
Patient perception of quality of life improves with dental implant provision.35 The quality of life of patients treated with implant-retained dentures (measured by OHIP) have shown satisfaction with their prostheses.112,132,133 Other studies assessed quality of life before and one month after restoration of implants and reported some improvements in aesthetic and functional aspects when anterior teeth were replaced using dental implants.134 Research in primary dental care within the UK also supports the view that quality of life is improved with dental implants, as measured by OHIP 49 in 107 patients.135
Discussion
There are no randomized controlled studies comparing the outcomes of accepting a space, conventional and implant-based removable and fixed partial dentures and the outcome of root canal treatment. A systematic review revealed weighted success and survival rates of implant-supported single crowns; fixed-partial dentures (bridges) and root-filled teeth, as shown in Table 4.14
| Years of follow-upx | Implant-supported single crown | Fixed-partial dentures (tooth-borne bridges) | Root-filled teeth | |||
|---|---|---|---|---|---|---|
| Success | Survival | Success | Survival | Success | Survival | |
| 2–4 years | 99% | 96% | 78% | 94% | 89% | 94% |
| 4–6 years | 98% | 97% | 76% | 93% | 94% | 94% |
| 6+ years | 95% | 97% | 80% | 82% | 84% | 97% |
Although, carried out in accordance with guidance for systematic reviews, the included studies were not randomized controlled trials, were heterogeneous, and limited to publications in English. This was still a thorough summary of the available literature. The success rates of root-filled teeth are comparable to the success of fixed-partial dentures at more than 6 years follow-up, and the survival of root-filled teeth is comparable to that of implant-supported single crowns at more than 6 years follow-up.14
Whether success or survival rates are taken into consideration, it is clear that it is worth providing endodontic treatment, as success and survival rates are comparable to extraction and replacement of the space with a denture, bridge or implant. These alternatives have other disadvantages and a more significant maintenance cost than with endodontic treatment, as summarized in Figure 1. Maintenance of the tooth has been shown to be the most cost-effective first line treatment option, following the failure of which, replacement with a single implant-retained restoration is the most cost-effective.136
A systematic review of the literature explored patient perceived benefit (oral health-related quality of life and patient satisfaction) of reconstructive dentistry.137
Although the available evidence was of variable quality, there were general trends showing patient perceived benefit when complete dentures and implant-retained overdentures were provided, with more significant improvements with implant-retained prostheses. Studies included revealed general satisfaction with resin-bonded bridgework. There was little reported difference in quality of life when patients with shortened dental arches were compared to those with removable partial dentures. Concluding remarks suggested the lack of suitable evidence to assess changes in quality of life in relation to restorative dental procedures, with the exception of edentulous mandibles treated with conventional and implant-retained prostheses.137
Where complex fixed partial dentures are provided, requiring significant manual dexterity to be able to maintain good oral hygiene, it must be borne in mind that the potential difficulties of maintaining oral health in an ageing population, where deteriorating motor skills, visual impairment and osteoarthritis may hinder manual cleaning of the oral cavity and dementia, may prevent patients adhering to changing oral healthcare regimens.138,139,140 Access to care for these patients may change and motivation to maintain oral health may deteriorate.141,142 Carers may not always be able to provide the level of oral care required, even when the method is demonstrated to them. Patients may not be able to tolerate lengthy dental treatment with increasing age and accumulation of medical ailments. Being rendered edentulous later in life may mean reduced ability to adapt to or tolerate dentures. Often, dental failures occur in older people due to caries, therefore having complex fixed restorations maintained by natural teeth can lead to fast deterioration when dietary changes occur and oral hygiene becomes less than optimal.143 Extractions may be contra-indicated due to previous or current medical treatment or disease. Implant treatment in older people is at risk of failure due to peri-implant disease resulting from deterioration of oral hygiene.144 These complications related to implants may be more difficult and costly to resolve than those associated with tooth-borne restorations. It may be most appropriate to maintain the natural dentition for as long as possible to reduce long-term, maintenance-related complications and costs.14 Patients should be involved in informed decision-making that affects their future dentition and maintenance.
Conclusion
When outcomes of alternatives to maintaining a natural tooth are considered, including the biological, financial, and psychological concerns of patients, it is better to spend available resources to maintain a natural tooth for as long as possible, in order to ensure that the commencement of the lifetime of the alternative to maintaining a space is delayed.

