Abstract
Given the number of perceived myths and fallacies in relation to tooth substance loss, this article seeks to address these using a wide variety of clinical cases as examples and by way of scientific references.
From Volume 48, Issue 5, May 2021 | Pages 343-356
Given the number of perceived myths and fallacies in relation to tooth substance loss, this article seeks to address these using a wide variety of clinical cases as examples and by way of scientific references.

In Part 1 some of the follies of using McNamara's fallacies were outlined. Fallacies are errors in reasoning, and not necessarily errors about truth or falsity. This part will highlight the ‘measurement and monitor’ approach to patients with tooth surface loss to illustrate some points made in Part 1 and it will expose some other unfortunate fallacies that have also affected UK dentistry.
One shibboleth is that tooth surface loss is always multifactorial. That is true sometimes – but not often – and certainly not always. For instance, one simple diagnostic clue is that if the length of the anterior maxillary teeth is reduced to be about the same, or less than their width, but the opposing lower incisors have a normal height to width ratio, then the main cause must have been chemical erosion.
The reasoning behind being able to make that important diagnosis confidently is that the appearance mismatch in the different heights of the teeth versus their widths must have been caused by a low pH acid eroding the upper teeth preferentially. That erosion is often due to hydrochloric acid with a pH of 1–2, coming up from the stomach, probably due to bulimia or gastro-oesophageal reflux disease (GORD). However, it could be due to multiple acid attacks coming in from the diet, and passing over the palatal and incisal aspects of the upper teeth, or sometimes a combination of both.
However, in any of those variations of acid attacks, the tongue sits on, and protects the lower teeth, but not the upper teeth, from the damaging effects of the variably erosive acids. That is why the lower incisor teeth maintain their normal height to width ratios, but the lengths of the upper anterior teeth become visibly shorter relative to their widths.1 The clincher for the diagnosis being due mainly to chemical erosion and not physical attrition is that, if indeed the patient had been rubbing the tips of their much smaller lower incisor teeth forcefully and consistently against the much greater surface area of the bigger upper incisor teeth (such as during extensive parafunction/bruxism), then the much smaller lower teeth would have come off worse and, therefore, be more worn on clinical examination.
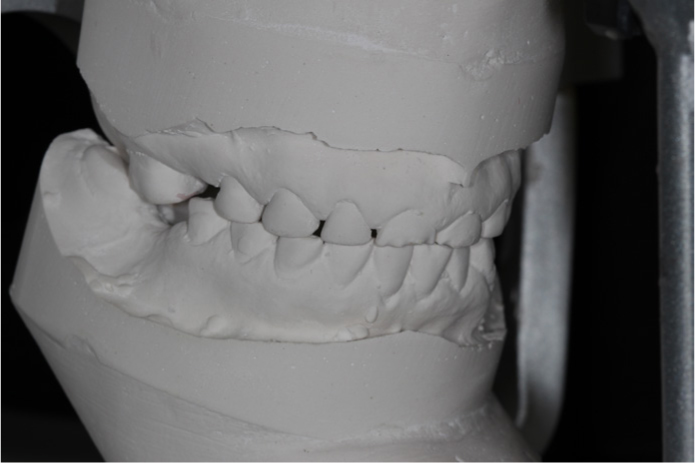
In the scenario described in Figures 1 and 2, that had not happened and, therefore, the reduced height to width ratio of the upper anterior teeth could not have been caused mainly by physical attrition. There was probably a little attrition of the acid softened incisal tip surfaces here, but that was very much secondary to the chemical dissolution of their enamel matrix.


The clinical implications of making that simple diagnosis early on are profound. It means that any protective resin composite material that is added to the eroded maxillary teeth to lengthen them, repair them and protect them against further acid damage then only needs to resist further chemical attack in the future, and not withstand massive physical forces. In that regard, resin composite is very resistant to chemical dissolution, unlike enamel which is damaged by any pH below 5.5 (remember your Stephan curves?) That means that resin composite is the material of choice to replace the missing tooth structure and to protect the marginal ridges of the eroded upper teeth, where most of the strength of teeth is still to be found.2
Figures 1 and 2 show the combination of erosion and arrested decay, probably mainly due to long-term sipping of highly addictive, full-sugar Coca Cola through the V-shaped ring-pull area in its can.3 Coca Cola has a pH of 3.15, with citric acid, phosphoric acid, carbonic acid and ascorbic acids being the main erosive acids that are present. The sugar present was responsible for the arrested decay, causing the yellow-brown colour of the labial aspects of maxillary teeth, which is visible in Figure 2. Please note that the length of the upper anterior teeth had been reduced locally, and this was limited largely to where the erosive acids had passed across them frequently – while the tongue protected the lower incisors from those erosive fluids.1
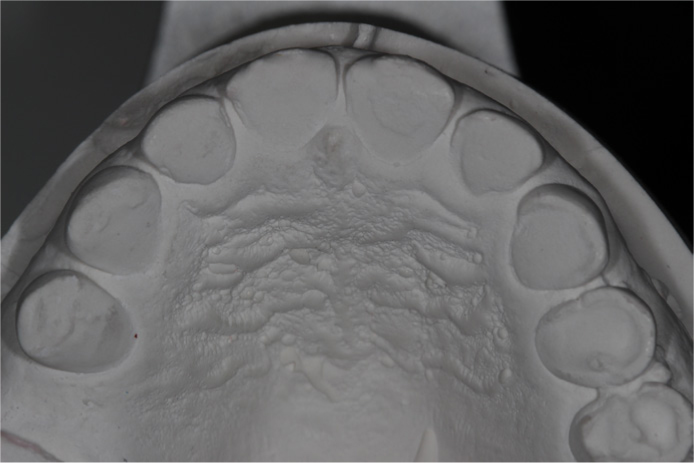
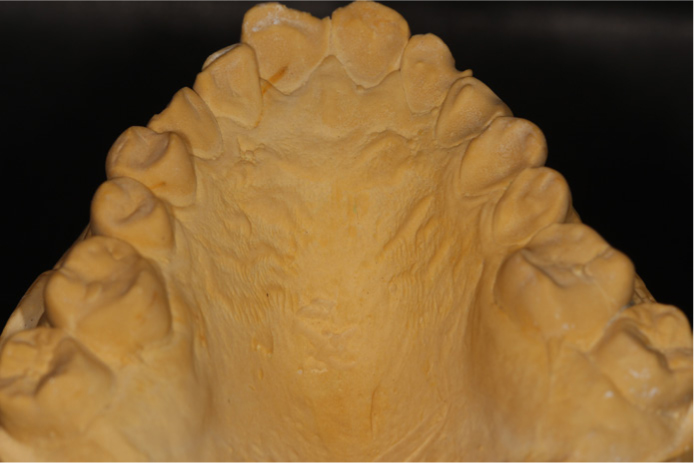
The obviously eroded palatal enamel, as well as the ‘enamel ring of confidence’ near the cervical areas can be seen in Figure 3.

The ‘enamel ring of confidence’ means that one can get very predictable bond strengths from the residual enamel left in that area, but only provided that one does not bevel it, which would destroy it in seconds. That enamel ring follows the outline of the palatal gingival tissues including the interdental papillae. That typical appearance in cases of chemical erosion is due to the presence of salivary glycoprotein in those regions, as well as neutralization of the eroding acids by the secretion of the gingival crevicular fluids. That appearance is a diagnostic feature of the problems having been caused by chemical dissolution, mainly of the palatal enamel, which was well away from the protective effects of that gingival crevicular fluid.3 The pejorative term for this classic clinical appearance of very localized palatal erosion limited to the upper incisors, and not present on the palatal aspects of the other maxillary teeth is ‘Sipper's gob’. (Incidentally, before some hypersensitive woke warrior kicks off, ‘gob’ is a ninth century Irish word meaning mouth or beak).
The fractured tips in Figure 3 were due to decay from the sugar in the Coca Cola undermining the very important marginal ridges and the less important incisal tips, which then fractured and had been repaired. Treatment of this patient was as follows.
Selective night guard vital bleaching was undertaken using 10% carbamide peroxide of the ‘framing side teeth’. That means that the maxillary canines and premolars were bleached alone first. Once the patient was happy with their colour, and 1 week after cessation of the bleaching, this was followed by direct, free-hand, non-layered bonding using a three-bottle bonding system, along with a chilled hybrid composite to repair the anterior teeth at an arbitrary increased anterior vertical dimension. Chilling hybrid composite stops it slumping, which makes it easier to sculpt to any desired shape before it is cured. That means one does not need tedious plaster models or a diagnostic wax-up, or a matrix based on that, in order to do that pragmatic treatment quite quickly.
Figures 4 and 5 show the clinical position at the start and the result 16 years later with minimal further treatment. The bleaching and bonding approach left all the remaining sound structure intact for that person's long-term requirements.1


Communication for valid consent reasons is important. In cases of tooth surface loss, it can be helpful to do a swift composite mock-up on their worn unetched teeth in advance to show the patient the proposed outcome in their case. Doing that in the chair allows the clinician to assess the patient's reaction to it, and to ascertain their views about possible length, shape and colour. If it is reasonably satisfactory, the composite can be photographed on their smart phone and then flicked off. Other photographs of what things look like before any treatment can be taken for immediate and much later comparison to allow the patient time to reflect on their options, but with a realistic view of what could be done. If one senses that the patient's expectations are even vaguely unrealistic, then that is the time to ‘bail out’ quite smartly.
As part of the discussions, many patients need to understand that avoiding drilling down their already worn teeth to place full crowns is better long term for their teeth.1 It is sensible to emphasize that the composite is neither perfect nor permanent, but then again, as human beings, nor are they, and nor are their dentists, and nor are any of their teeth ‘permanent’. Composite is weak if it is placed in thin sections, and if it gets twisted by shear forces, but it is very good if the material is in thick section and it is loaded in compression. That is the reason why one often covers the worn teeth in a ‘composite bandage’ that is stuck on the inside and the outside of their worn teeth to protect them. Some patients like that expression as an explanation of what is being proposed as being just one of their treatment options. Others prefer the description that their damaged teeth ‘will be the filler in the new protective composite sandwich’. Either explanation (or others) is fine provided it is recorded in the notes. Simple explanations using everyday words often help patients to understand the thinking involved in offering to treat their damaged teeth with an ‘additive’ approach (rather than a ‘subtractive’ one) by using expendable, repairable and renewable protective resin composite material.
It is an obvious fallacy that dentists could offer all that time for discussions and keeping records of them, as well as doing a clinical composite mock-up to obtain valid consent, and then undertake that sort of biologically sensible treatment regularly, for three lousy UDAs. Perhaps some altruists might wish to try to do so, but only if they really did fancy bankruptcy as their ultimate career goal.4
The rationale for direct resin composite bonding early on, rather than unpredictable ‘monitoring’ of significant tooth surface loss, is that the missing tooth tissue is not going to re-grow ever and, therefore, that the limited clinical time available is probably better spent protecting whatever is left. In terms of predictability of the effects of preventive advice, it is important to recognize that information transfer from any healthcare professional to any patient about any health-related issue, does not guarantee compliance with that advice. Noble as that aspiration is, it is another fallacy to suggest that it will always do so.
That is particularly the case if the perceived problems are due to uncontrollable behaviour at that time (eg bulimia) or illness (eg refractory GORD, even after triple therapy) or due to addiction (such as to erosive fizzy or some other drinks or substances). In practical management terms, once much of the enamel is breached, particularly at a relatively young age, one is probably better off protecting the remaining strength of the teeth by maintaining their vitally important marginal ridges by bonding appropriate protective material to their palatal, labial and/or incisal areas as appropriate. That pragmatic and practical approach seems to many compassionate clinicians to be more sensible than assuming that there will be compliance with good preventive advice, and then putting all one's faith in aspirational, time consuming, but unproven, ‘observo-dontics’ while the remaining invaluable sound tooth tissue can be slipping away.1
It is another fallacy that it is always practical to measure and, thereby, ‘monitor’ tooth surface loss effectively. The reality is that this dogmatic approach is unproven scientifically, very time consuming, almost impossible to do so reproducibly, or reliably, or cost effectively, or in any internationally agreed way. Over the years, various methods have been described to try to measure tooth surface loss problems in detail. These have included using clinical descriptions to produce different tooth wear indices, making sequential plaster casts at arbitrary intervals, taking clinical photographs of variable reproducibility, and/or using digital scanning, or some other research device.
Over the last 40-odd years, difficulties in trying to measure tooth surface loss reproducibly have resulted in a variety of indices, each one criticizing, or modifying, a previous one. It might be helpful to briefly review the history of some of the changes in indices describing tooth surface loss or tooth wear.
In 1979, Eccles, who was originally from Northern Ireland, but was a professor in Cardiff, developed a tooth surface loss index with a scale of 0 to 3, with the description of level 3 having further subsections of 3a, 3b, 3c and 3d, denoting increasing severity of the problems.5
Eccles' index was based on the extent of the tooth surface loss that was visible on clinical examination with zero/nought (0) meaning none.
In 1984, in London, Smith and Knight's Tooth Wear Index (TWI) modified Eccles' classification.6 Basically, it changed the Eccles 3c, 3d sub-classification to a single number, 4. The number 4 was to be used to record that the pulp, or the reparative dentine overlying where it used to be, could now be seen on clinical examination. Each surface of each tooth was to be scored from 1 to 4 using the TWI.
In 2008, Bardsley in Liverpool, described the development and publication of many other classifications of tooth surface loss, which were used in different countries. She highlighted the lack of consensus, or acceptance by general dentists of these indices, as well as the practical problems of those monitoring approaches in real life general dental practice.7
It might be pertinent (or perhaps cynical) to point out that one way for an academic in dentistry to increase their personal citation in academic journals is to invent, or modify, an index of some sort, which can then be named after them and cited in any further papers.
Lussi and co-workers subsequently described an index of 1 to 3. They used the visible clinical exposure of half, rather than one-third, of the dentine as their arbitrarily chosen cut-off point between calling the tooth surface loss level 2 or level 3.8
Bartlett, Ganss and Lussi (2008) described a version of Lussi's earlier work as the basis for what they termed the ‘Basic Erosive Wear Examination’ (BEWE). This was intended as a screening method for general dental practice and was intended to be like recording a BPE and supposedly be easy to record for legal as well as clinical care reasons.9
To anyone interested in the semantics of tooth surface loss, the term ‘BEWE’ has a hint of the oxymoronic about it. Erosion is due to chemical loss of tooth structure whereas, traditionally, wear has a connotation of it being caused by something physical, such as attrition (eg bruxism/parafunction) or tooth abrasion by some external, rough material. Which is it, please? Does the ‘BEWE’ term vaguely help to sustain the fallacy that it is always too difficult for any interested dentist to diagnose the main cause of the problem of that individual patient's tooth surface loss? Does that assumption then lead on to the rather dogmatic statements being made about giving preventive advice (which is very sensible) and then monitoring things with, for example, models (which is more dubious). That alleged ‘monitoring approach’ is definitely questionable when the tooth surface loss has resulted in the loss of up to half of the tooth structure, such as in BEWE 13.
Interestingly, the BEWE term has been heavily advertised recently by toothpaste manufacturers, in various commercial magazines and dental journals. Some might think that there could be some conflict of interests in toothpaste manufacturers possibly sponsoring research,10 or advertising BEWE so heavily, as part of their commercial promotion of their various toothpastes. Conceivably, that intensive and expensive advertising might seduce some unwary dental professionals into believing that ‘measuring and monitoring’ is THE most appropriate approach to managing tooth surface loss. The accidental, or intentional, subliminal message for dental professionals might be to advise patients about their acid issues and to emphasize prevention, but then to ‘monitor the wear, but please do get the patient to use one of the preferred toothpastes’. BEWE is only one of many ways of recording a patient's tooth surface loss. Other indices are listed above. Photographs, models or scans are also methods of recording the clinical situation at any specified time. The clinical notes should reflect the patient was aware of their problems.
Advice about prevention is great, and to be encouraged enthusiastically, but, from an individual patient's perspective, ‘monitoring and measuring’ their wear until they are missing about half their invaluable sound tissue in many sextants (as in BEWE 13) before considering any protective restorations, might well not be in their long-term best interests.9 In fact, the BEWE advice deprecates the use of any restorations, even with a score of BEWE 14.9 It does not even mention the possibility of additive, non-destructive or protective ones being used, which many caring clinicians would regard as being part of preventing future problems. A 2019 article alluded to potentially very high costs of possible treatment, presumably for full-mouth rehabilitation, along with a suggestion for specialist referral at BEWE 14.11 In fact, it is another fallacy that patients need destructive dentistry to be done in order to provide full crowns on all their teeth for supposed full-mouth rehabilitation (spelled ‘full mouth mutilectomy’). That 2019 paper did not even mention preventive resin additions being bonded to eroded teeth at an increased anterior vertical dimension, even when up to 50% of the surface of the teeth was missing (BEWE 13). Rather worryingly, that paper had some seriously heavyweight co-authors on it, and so it is likely to be perceived as definitive advice by many UK dentists.11
However, other concerned and compassionate clinicians feel that the BEWE-based dogmatic advice ought to be challenged more vigorously on a variety of grounds, such as practicality, predictability, cost-effectiveness and/or professional responsibility. Their view is that much earlier additive composite bonding techniques would prevent a lot of later problems for many vulnerable patients (eg those with bulimia) and would do so more cost-effectively than expending scarce resources on multiple time-consuming reviews and taking dubious plaster models.1
In the case of patients with serious tooth surface loss associated with bulimia, it is fallacious to imply that monitoring with BEWE is without potential downsides, including possibly being later accused of supervised neglect. So, just why are people watching the invaluable enamel for bonding disappear, probably in an uncontrolled way, and what exactly are they waiting for? Is it so that someone, sometime, can do full coverage crowns on the even more eroded teeth, on some sunny day, and thereby do about 40 years' worth of abrasive tooth damage in a few minutes to those now even more badly damaged teeth?
In the mid-1990s, one of the main reasons for the acceptance by some of the ‘measure and monitor’ approach to tooth surface loss caused by bulimia was that one dogmatic group had insisted that despite ‘catastrophic tooth surface loss’ no veneers of any type (eg composite) were advised to be used. ‘Instead, full coverage crowns, if timed appropriately’ was held to be the treatment of choice.12 Even in 1995 that was (and it remains) a nonsensical approach, and lacks compassion for patients suffering from bulimia. However, by way of evidence as to why that fallacious view probably became the accepted approach for many, one section from that publication in the British Dental Journal is quoted below:
‘The erosion in the vomiting group was often clinically catastrophic, both in the extent and the probable rate of progress. It was not uncommon to find teenage girls with complete loss of the palatal enamel of the upper anterior teeth. This produces a poor and declining appearance and a very difficult restorative problem. In relatively immature girls with an obsession about appearance this could be a factor in perpetuating the psychological problems. Relatively short-term solutions, such as palatal veneers, while the underlying condition continues, may do more physical harm than psychological good. This deterioration may expose rough surfaces that will produce rapid wear of the opposing teeth. If the treatment can be timed appropriately, full crowns can significantly improve the appearance and give a therapeutic psychological boost.’12
This author believed then, as he does now, that this dogmatic statement was bereft of compassion and was utter nonsense. Unfortunately, once it was published in the British Dental Journal, it came to be accepted by many unquestioning acolytes as being the infallible truth.
This patient presented with significant shortening of her upper teeth and a dead, discoloured upper left central incisor, which had been root filled some years previously and was asymptomatic (Figures 6 and 7). She had been referred with some mounted study casts, and many other dated study casts (Figures 8 and 9), with the request for a ‘full mouth rehabilitation to establish the correct vertical dimension and occlusion’.


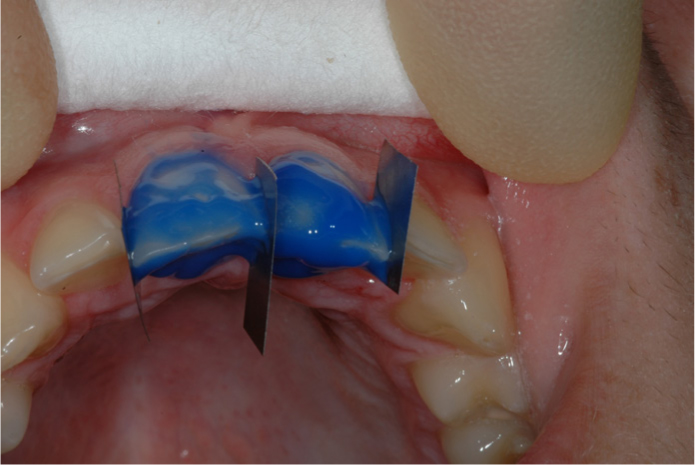
The patient readily admitted to many episodes of bulimia for years for which she was ‘being monitored’. After some interesting discussions and explanations, which were followed by a direct resin composite temporary ‘mock-up’ on the unetched teeth, the patient elected to have a couple of days and nights of inside–outside bleaching undertaken at her discoloured upper left central incisor. One week later, that was followed by a single session of chilled direct resin composite resin being applied freehand, without a matrix or a wax-up, from the upper right premolar to the upper left premolar, and then modified to her specifications (Figure 10). The main purpose of the resin composite additions was to protect the remaining tooth structure from further hydrochloric acid attacks, but there was some limited improvement in the appearance of her allegedly ‘BEWE monitored’, but now badly eroded, teeth (Figures 6, 7 and 10).

This case of the patient suffering from bulimia raises several questions, such as: if it happened to be caries that was seriously threatening the vulnerable teeth, would most responsible dentists choose to wait until that amount of the structure of the teeth was heavily compromised before using protective restorations? Really? If it was your daughter?13 Many compassionate and experienced dentists, if they were able to do so without incurring a financial penalty, or other risk, would intervene earlier than at BEWE 13 with non-destructive sealant restorations at an increased anterior vertical dimension. That could be particularly the case if it happened to be their own daughter who had that severity of tooth surface problem before it got to the situation shown in Figure 6.13
The dogmatic ‘give advice, get them to use an unproven xyz toothpaste and then measure only’ is just another McNamara's fallacy – making important something one can try to measure, rather than measuring important things. The important things often include just how long does that patient have to live with their tooth surface loss problem? What happens if it gets much worse and/or what might make more cost-effective management sense for them? What are the hidden costs inherent in multiple expensive review visits?1
The apparent antipathy to placing any protective and/or reparative resin composite restorations, even when the enamel has been breached significantly, which is a corollary of the ‘wait until worse than BEWE 13’ in the BEWE measurement philosophy, is troubling. That is partly because it has been adopted unquestioningly by so many dentists. The corrupting UDA measurement system probably is also involved because there is no obvious reason for any NHS dentist to risk time-consuming intervention for three UDAs. However, to some other independent clinicians, who were and are, dealing with a lot of patients with tooth surface loss, the dogmatic approach to ‘monitoring and advising only’ (aka ‘observo-dontics’) appears to be rather lacking in compassion to help practically with those unfortunate patient problems – even when one could do so quite easily, based on good relevant clinical evidence.14,15,16,17
For very many years there has been overwhelming evidence available that resin composite, once it is bonded at an increased anterior vertical dimension, and shaped to the patient's satisfaction, is successful and adequately durable.14,15,16,17
The composite addition restorations are popular with patients, have minimal adverse biological consequences and have acceptable durability, particularly as they can be repaired as required, without causing the longer-term problems to teeth that crowning them can do.18,19 Composite is universally available and predictable to apply to dentine and enamel, preferably using a well proven adhesive approach.1 The crazy effects of the way things are measured and rewarded by the fiat currency of UDAs means that this proven, protective, durable treatment often does not get done while there is still enough enamel present for it to be undertaken predictably by most dentists. Unfortunately McNamara's fallacy strikes again here – because the government's chosen UDA measurement system, coupled with some companies' commercial advertising to improve their profits, has resulted in the sometimes fallacious ‘watch and wait’ approach being adopted by many as being the correct one.11 Is that unquestioning acquiescence due to the various ‘influencers’ actively promoting ‘BEWE’ – or could it be due the malign and corrupting effects of measurement by UDAs?20
The alarm bells should have started ringing in the UK about the emerging epidemic of tooth surface loss when Robb published the results of his PhD in 199121 (30 years ago) and some years later in the Journal of Oral Rehabilitation along with Smith in 1996.22 That independent, unsponsored, research, carried out in Southeast England,21,22 showed that greatly increased tooth surface loss was occurring mainly in people under 26 years. Robb drew attention to the worrying finding that those under 26 had three times more tooth surface loss than the next cohort of those aged between 26 and 35, and twice that of those people between 36 and 45, and 45 and 55.21,22
However, that was not an isolated finding. Around that time, many other interested clinicians in Birmingham, Liverpool and London in the UK, and elsewhere in the world, had noticed and reported the same pattern of greatly increased tooth surface loss occurring in younger people. Some had lectured extensively and written about what factors might be involved in causing those increasing problems.3 The ‘read through’, even 30 years ago, was that whatever the combination of factors that was responsible for what was happening in the much younger age groups to cause this widespread tooth surface loss, it would probably have catastrophic financial and other consequences when that cohort got much older unless something sensible was done.3 However, in spite of all that alarming clinical evidence, the ‘wait and see’ policy prevailed for many. Other pragmatists, however, found that it was relatively easy and cost effective to treat the different wear problems pragmatically with direct resin composite additions to the damaged teeth at an increased anterior vertical dimension.1,14,15,16,17
It is yet another fallacy that patients with decent amounts of periodontal ligament have difficulty in adapting to an increase in anterior vertical dimension if their ‘enamel overcoats’ have been left on them. In other words, the restorations increasing the anterior vertical dimension should not have caused pulpitis by extensive drilling or microleakage to provide them. Other stipulations for predictable adaptation include that the increase should be at least a millimetre in the anterior region and that the patient should like the appearance change that was created by that treatment (Figures 11 and 21). In addition, they do need know in advance that it will take a variable amount of time for that adaptation to happen, but that this is required by them to protect what is left of their worn teeth. That ability to adapt to occlusal changes was demonstrated as long ago as 1962 by Declan Anderson, who was a polymath and physiologist working in the UK. He used onlays at an increased vertical dimension to show that people adapted to planned changes in their occlusion without any significant problems.23 His findings were followed 13 years later by Bjorn Dahl in l975.24 Dahl used his device as a preliminary to using gold pinledges to restore the worn teeth.










It is another fallacy that the localized anterior ‘orthodontic type’ of device that was popularized by Bjorn Dahl was his idea alone. Some suggested that it should be called the ‘Dahl concept’, while others used his name as a verb, such as in ‘to Dahl’ in composite restorations, which he had never described anywhere, or at any time. The truth is that the anterior bite platform idea that Dahl described was remarkably like that described much earlier by Sved, which was used extensively during traditional teenage orthodontics for reducing anterior overbites. To be fair, Dahl did draw attention to less destructive ways of managing localized problems of tooth surface loss. However, that localized approach was resisted by some traditional ‘occlusionistas’ for whom the ‘full mouth rehabilitation to achieve the optimal occlusion’ was still the gold standard for managing tooth wear.
Perhaps one of the daftest beliefs in the occlusionista tribe is that excessive occlusal forces cause bending of the enamel prisms of teeth in the cervical region, thereby causing them to fly off and leave supposed ‘abfraction lesions’.
‘Abfraction’, like Santa Claus, is just a figment of some dogmatic occlusionista's imagination. Such theoretical and anecdotal cases as have been described in various case reports were probably due to dietary acid erosion episodes, which were followed very soon afterwards by aggressive tooth brushing using abrasive toothpaste on the buccal aspects of teeth with a thin periodontal phenotype (Case 4, Figures 22–25). The clinching point is that no one has ever seen enamel prisms apparently fly off from the palatal aspects of those very same teeth where there is lots of attached thick periodontal tissue still present (Figures 24 and 25).




If teeth were really being bent by excessive occlusal forces, then serious clenchers and bruxists, complete with their masseteric and temporalis hypertrophy, would provide the biggest test for enamel prisms in the cervical region However, one never sees ‘abfraction lesions’ in cases of serious attrition in patients with a thick periodontal phenotype because the periodontal ligaments act as resilient shock absorbers. (Please see Figures 26 and 27 where no cervical prisms have been ‘broken off’. Figures 28 and 29 show the facial signs of parafunction that cause this tooth wear.)




It is yet another fallacy that the theoretical mechanical and mathematical models used to support the far-fetched fantasises about abfraction ever simulated realistically the variable visco-elastic dampening characteristics of healthy and sound periodontal ligaments. In fact, the proponents of the abfraction theory do not even mention the roles of the exquisitely innervated periodontal ligament mechanoreceptors (‘the lovely ladies in the ligaments’) in controlling occlusal forces and jaw positions.25
For many traditional dentists, the role of occlusion in causing or managing tooth wear has been deemed to be vitally important. For instance, one old fallacy is that anterior slides from RCP to ICP cause tooth wear. Another fallacy is that non-working interferences trigger bruxism and thereby cause tooth wear. Whenever those allegations are made as justification for very aggressive full mouth rehabilitation treatments, one might point out very gently that ‘coincidence does not prove causality’. In other words, one could certainly demonstrate various occlusal problems in patients with bruxism and tooth wear, but they were not necessarily causal, and could well have been coincidental.
Another McNamara fallacy about full mouth rehabilitations for managing moderate tooth wear is that if various measurements of great precision are used to set highly sophisticated articulators, that somehow this would compensate the patient for the much more important measurement of the biological damage being done to their sound tissues necessarily involved in full mouth rehabilitations.26 The truth is that the requirement for very precise measurements was, and is, caused mainly by the destruction of sound tooth structure of the worn and unworn teeth alike to achieve the desired tooth preparations for that particular, and changeable occlusal philosophy to be implemented.27 The impressions of, and the relationships between, those now professionally mutilated teeth really do need to be done with great precision. However, that sophisticated measurement is only required because of the serious reduction in the stiffness of the teeth following the loss of their marginal ridges where most of the strength of teeth is situated (Case 6, Figures 30–32).2 The much more important thing that ought to be measured is the long-term outcome for the teeth following that dentist-delivered abrasive tooth tissue loss.19 Different shapes of abrasive burs were, and still are, used to destroy very precisely up to two-thirds of the tooth structure of a lot of the sounder teeth to achieve those scientifically dubious ‘occlusal goals’. The reality was that, in many cases of tooth wear, the aggressive treatment for multiple crowns for all the teeth, whether they were worn or not, in order to achieve that supposed ‘ideal occlusion’, was often worse for the teeth than the disease than it purported to treat (Figures 30–31).26,27



It is another fallacy that exactly even anterior guidance is required if one is adding direct composite to eroded teeth that have intact marginal ridges.2
Maxillary central incisors are roughly twice the size and have a much greater palatal surface area than maxillary lateral incisors. Why then should the much smaller lateral incisors be asked to carry as much load in protrusion as the much bigger central incisors to produce even anterior guidance (Figures 11, 12, 20, 31, 32). That just about might make a tiny amount of sense in relation to extensively prepared teeth for full coverage crowns (Figures 31 and 32). However, even then, it is highly debatable. If one removes somewhere between 63% and 72% from both the central and the lateral incisors for anterior full coverage all-ceramic crowns, then there should be much less left of the structure of the lateral incisors than of the central incisors.28 However, according to the ‘even anterior guidance’ idea, all of the now much-weakened lateral incisor cores are expected to take the entire load evenly during the protrusive movements of the mandible, but at this stage, to do that without the strength that was present previously in their marginal ridges before the burs destroyed them.2 In fact, the truth is that the supposed requirement for ‘even anterior guidance’ is often created by the elective destruction of about two-thirds of the sound tooth tissue for full coverage bonded crowns or all-ceramic crowns as was described by Edelhoff and Sorenson in 2002.28,29
That amount of tooth ‘preparation’ causes a serious reduction in their stiffness2 as well as often causing problems for pulpal health. If any clinician has been unwise enough to destroy lots of sound marginal ridge structure electively, then it is true that they really do need to be very careful with what little is now left. That is why one should, indeed, use the appropriate sophisticated articulator, and be incredibly careful with inter-occlusal records, to set it properly.
However, it should be kept in mind that most of those problems were actually caused by the elective destruction of the load bearing marginal ridges in the pursuit of some antiquated, fundamentalist, occlusal ideals.26 ‘Waiting and watching’ until a lot of sound tooth tissue has gone in order to then crown multiple worn teeth in the pursuit of any supposed ‘occlusal nirvana’ is both unscientific and unreliable. The sad truth is that aggressive preparations for full coverage crowns destroy the marginal ridges and, in so doing, affect badly the residual strength of the prepared teeth as well as hazarding their pulpal health in various ways, which ultimately can result in the teeth being lost.2,18,19












If the marginal ridges of anterior teeth are still intact, which they are in most cases of erosion, one can bond resin composite to the teeth at any appropriate pragmatic height without fear of the teeth breaking with those increased loads (Cases 1, 2 and 7).26 Usually, all one needs to do is to make the eroded short upper incisor teeth appear to be longer than their widths and make their incisal tips parallel to the interpupillary line. The upper incisors tips should also follow the outline of the lower lip and any irregular dark spaces should be bonded to get rid of them. If bleaching is desired, it ought to be done first because the composite will not bleach (Cases 1, 2 and 7).
If it is desired to protect extensively worn anterior teeth that have lots of exposed dentine, then the palatal aspects of the maxillary canines and occlusal aspects of the upper premolars can be bonded pragmatically to help do that. The ‘closest speaking space’ is a pragmatic guide to what height that is. One can assess that quite easily by asking the patient to count from 60 to 80 and watching how close the anterior teeth are to one another throughout that counting. If one stays short of intruding into that space, there is never a problem with patient adaptation (Cases 1–3 and 7).
One clinical trick is to keep the hybrid composite within the occlusal table of the sound ring structure of the upper premolars (and sometimes the first molar) teeth. That means that the patient can only load the composite in compression (Figures 36, 37 and 40). It is important that the opposing teeth have an intact ring structure themselves and are sound. Putting the composite into compression on the side teeth protects the composite on the more vulnerable dentine on the oblique surfaces of the worn anterior teeth from potentially damaging shear or tensile forces (Cases 2, 3 and 7).
In summary, the main benefit of composite additions to worn teeth is that a pragmatic approach maintains and protects the inherent strength of the eroded teeth's marginal ridges, while still improving the appearance.30







In many ways, the preventive bonding of eroded and disappearing flat surfaces of the teeth in young people is analogous to the arguments for using fissure sealing to prevent dental deterioration continuing due to decay. If that additive protective resin composite bonding is not done more widely soon, then by the time the young cohort of UK patients with excessive tooth surface loss get through to their forties or fifties (with many of them having 40-odd years still to go) there will be no sound tooth tissue left. The consequential social, financial and legal costs will be huge, as many have been warning for over 35 years.31
The numerous problems of excessive tooth surface loss, particularly in young people, have been known for many, many years.1,3,21,22,31
Ongoing deterioration could, and should, have been prevented and managed more effectively. Many effective treatments were developed by pragmatic clinicians to help deal with the appearance problems without destroying the remaining tooth.1,14,15,16,30,31 Sadly, there appears to have been a lack of compassion by some in the profession towards people with tooth surface loss problems. Unfortunately, some fell under the spell of various ‘influencers’, some of whom might well have had dubious motives. Others were institutionalized by the government's imposition of the iniquitous UDA system on them, which discouraged them from intervening appropriately. Unfortunately, McNamara's fallacies struck, with the ‘measurement mirage’ being pursued by most, while the invaluable matrix of many of the worn teeth quietly slipped away, never to return. Others, in the vain pursuit of a fallacy about an occlusal nirvana, ground away lots of sound tooth tissue, and in the process did years and years of physiological tooth wear in minutes.26,27