References
Gagging – bringing up an old problem part 2: management of the condition
From Volume 45, Issue 8, September 2018 | Pages 712-718
Article

Following on from the initial consultation (discussed in part one of the series), the clinician will have now established a good understanding of the patient's dental history and his/her overall expectations. Furthermore, the underlying aetiological factor(s) and an estimation of the severity of the gag reflex should have been properly evaluated. The clinician must now decide the most appropriate intervention(s) that will be implemented, in the first instance, with the aim of managing the gag reflex and achieving a successful outcome. The methods chosen will vary between different patients and, in most instances, a combination of different management approaches is normally recommended.
Management options
There are numerous treatment approaches which have been suggested in the literature and are categorized into the following methods: behavioural, pharmacological and non-pharmacological. Importantly, it should be mentioned at this stage that the evidence base for the management of the gag reflex is relatively poor and reliable conclusions cannot therefore be confidently drawn. The Cochrane Library1 has reported that future studies are required in order to highlight the effects associated with each intervention and to provide evidence to inform clinical decisions better. Therefore, at the present time, it is recommended that clinicians have an overall awareness and understanding of all the available management options for gagging patients; from the author's experience, the clinical situation varies widely between different patients and there is no one approach that will be suitable (or appropriate) for all scenarios.
Behavioural
It was discussed in the previous article that a prolonged and exaggerated gagging response to a normal (non-noxious) stimulus, or where no mechanical stimulus occurs at all, was the consequence of a conditioned response. Leading on from this thought, it should become apparent that these learned behaviours are also amenable to change. In theory, the emotional responses triggered by the higher centres can be completely reversed with complete elimination of the hyperactive gag reflex.
Relaxation
There are various techniques which can be used to reduce the patient's anxiety state and remove unhelpful thoughts.2 Hoad-Reddick suggested a method of ‘controlled rhythmic breathing’ which involves deep inhalations and exhalations to focus the patient into a state of self-hypnotic relaxation.3 This is also beneficial as patients who gag are more prone to hold their breath during their appointment.4
Distraction
This serves as a temporary distraction for patients whilst a potentially unpleasant procedure is being undertaken. This may include conversation, instructing patients to raise their legs during the course of a procedure or asking them to visualize a safe and comfortable place. Relaxation and distraction interventions can be used in combination. However, these methods are usually only successful in mild gagging patients.2
Hypnosis and suggestion
This provides the clinician with a set of skills which helps to facilitate or augment a course of treatment by temporarily removing the gag reflex. There are relatively few contra-indications for this type of treatment. The principles of hypnosis include anxiety control, relaxation, desensitization and boosting confidence.5 A trained and experienced hypnotherapist may even be capable of abolishing the gag reflex altogether.
Systematic desensitization
Positive experiences can alter maladaptive thought processes of the patient. Consequently, previously learned behaviours, which occurred via classical conditioning, are changed and a form of re-education can take place. Gradual exposure to the noxious stimuli occurs in combination with praise and positive encouragement from the clinician; the aforementioned behavioural techniques may also be used at this stage to aid progression.
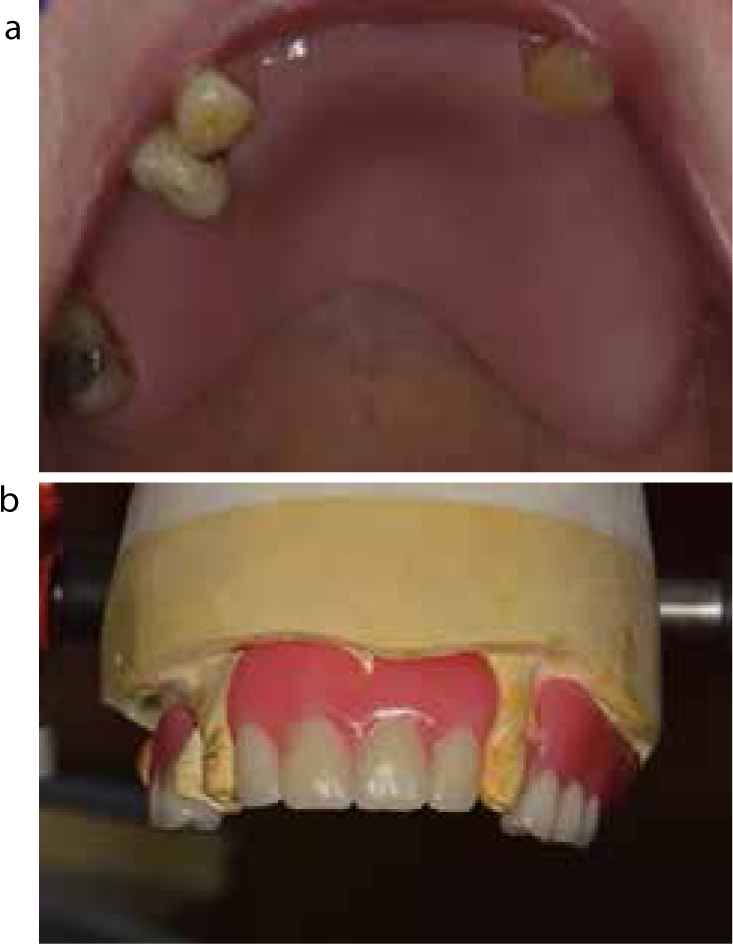
Patients with a severe gag reflex can be re-educated by using acrylic discs, a toothbrush, impression trays, x-ray holders, dental mirrors, marbles and/or an acrylic training plate (Figures 1 and 2). Whichever method is selected, the patient is presented with this task as a form of ‘homework’, where the intensity, duration and frequency is increased slowly over time, in order to allow the patient to habituate to the gagging sensations and develop coping strategies.4

Errorless learning
This has similar principles to systematic desensitization. It allows for gradual, increased durations of the exposure to the noxious stimuli. It is an effective method which is used for patients who cannot tolerate their dentures as they provoke gagging. Importantly, the gag reflex must not be stimulated in order for the technique to be successful with removal of the conditioned behavioural response.
The disadvantage of this technique is that the treatment takes place over a prolonged period of time, which will vary greatly between patients. Compliance is another crucial factor. It is vital that patients follow the instructions given to them by the clinician and that they carry out the necessary ‘homework’ in order for progress to occur. Regular encouragement will be necessary by the dentist.
Cognitive behavioural therapy
This is commonly used to treat anxiety disorders and depression. This method of intervention can manage irrational thought processes by challenging a patient's strongly held beliefs, such as their perceived consequences of gagging. The eventual aim is to apply these acquired skills to situations faced in daily life. This is a highly effective technique and, under these circumstances, the therapist can prove to be of invaluable assistance to the clinician.
Pharmacological
The drugs used for management of gagging are classified as either centrally or peripherally acting drugs. However, pharmacological intervention will only offer a short-term solution, especially for patients with severe gagging problems.6 These agents act to desensitize the mucosal surfaces and, consequently, the patients are less likely to gag.7
Peripherally acting drugs include topical and local anaesthetics. The rationale for the use of these drugs is that, if the afferent impulses from sensitive oral tissues are eliminated, the reflex of gagging will not take place.8 Centrally acting drugs are categorized as antihistaminics, sedatives, tranquillizers, parasympatholytics and central nervous system depressants.
Local anaesthetic
In addition to the normal anaesthetic techniques, there is the glossopharyngeal nerve block (GNB) which is reported to obtund the gag reflex.6 Watt and MacGregor advocate infiltration of the greater palatine nerves when taking maxillary impressions where the cause is solely somatogenic.9 Theoretically, the GNB works in gagging patients because the ninth cranial nerve supplies sensory innervation to the posterior third of the tongue, vallecula, the wall of the pharynx, the tonsils and the anterior surface of the epiglottis.
A randomized control trial performed by Mogensen et al10 demonstrated the benefits of using a lidocaine lozenge over oral solutions to diminish the patient's gag reflex during endoscopic procedures. Other forms of topical anaesthetics include gels and sprays which have shown benefit when applied to the palate prior to maxillary impressions.11,12
Conscious sedation
This usually includes nitrous oxide, benzodiazepine or propofol; the addition of a sub-anaesthetic dose of ketamine can also be considered. Sedation will temporarily eliminate gagging and anxiety during a dental procedure. Inhalation and oral sedation methods are normally more appropriate for mild gagging patients. Inhalation sedation (Figure 3) will give a more profound level of gag suppression at the beginning of treatment; however, the gagging response will return as soon as the sedation reduces.13 Sedation is a useful approach for urgent treatment, but it is clearly not a long-term solution if appliances are to be worn on a regular basis. Therefore, this intervention does not obviate the need for other treatment modalities.

General anaesthetic
This is generally considered as a last resort for patients who do not respond successfully to any other form of treatment. This should be used only on rare occasions for patients with a gag reflex, considering the inherent risks.
For the sake of completeness, other pharmacological approaches include antiemetic and herbal medications. A randomized control trial was performed by Barenboim et al,14 which investigated the use of Granisetron, a medication used to treat nausea and vomiting, and its effectiveness in the management of gagging patients. However, the study was flawed and there were no definitive conclusions.
Non-pharmacological
Interventions that are neither behavioural nor pharmacological are classed as non-pharmacological methods.
Salt on the tip of the tongue
Theoretically, the salt stimulates the chorda tympani branches of the taste buds in the anterior two-thirds of the tongue (Figure 4), thereby depressing the gag reflex. This method produces a lot of saliva. However, Chidiac et al demonstrated this approach as having little effect on the gag reflex compared to conscious sedation.15

Acupressure
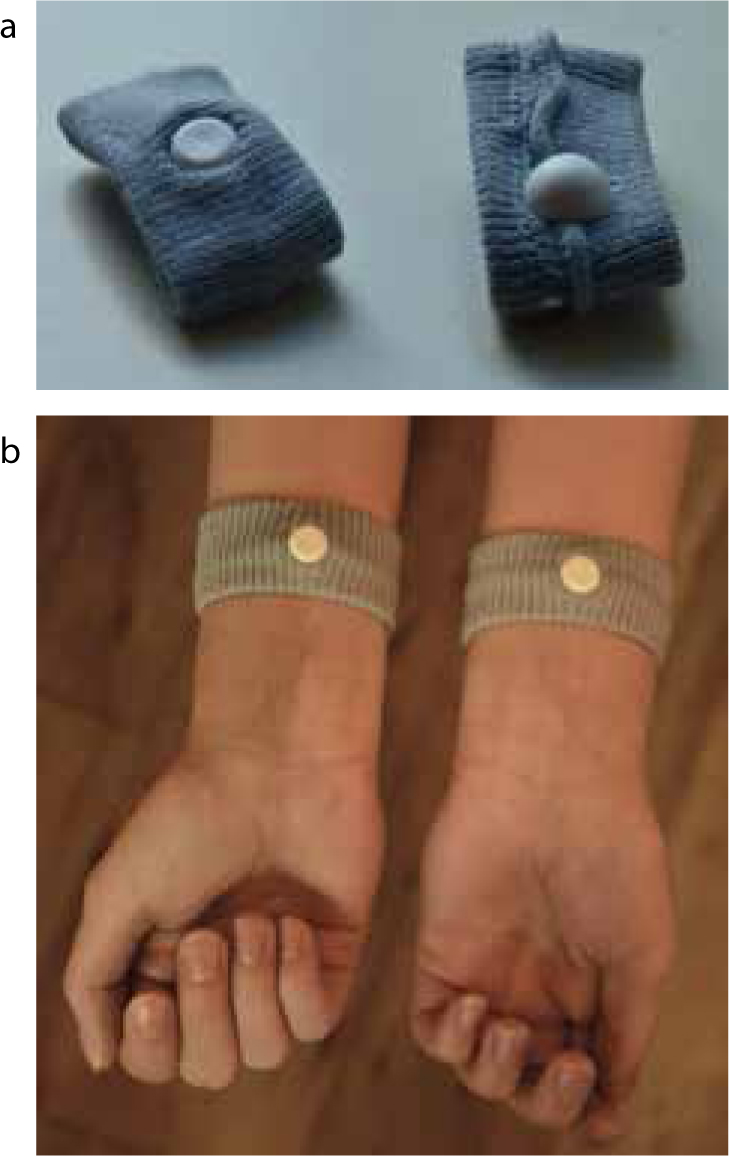
Stimulation using acupressure of point Pericardium 6 (P-6) has been reported to be effective in preventing nausea and vomiting.16,17 Point P-6 is situated on the palmar aspect of the forearm, 2 cm above the transverse crease of the wrist, between the tendons of m.palmaris longus and m.flexor carpi radialis.18 P-6 acupressure is commercially available as travel sickness bands (Figure 5). Acupressure of the Conception Vessel 24 (CV-24), located on the labio-mental groove, has also been shown to decrease gag reflex during maxillary impression procedures.19
Acupuncture
This is a safe, quick, inexpensive and relatively non-invasive technique for controlling exaggerated gagging. A controlled study by Lu et al16 established that acupuncture of point P-6 significantly reduced the gag reflex. Acupuncture of the ear and CV-24 have also demonstrated an ability to control the gag reflex.20 However, in order to perform this skill, the clinician will require additional training and experience.
Prosthetic management
A correct assessment must first take place. This is followed by either technical modifications to the current prosthesis, in order to make the appliance more acceptable to the patient or, alternatively, a new approach may be taken if the gagging patient is still unable to adapt to the appliances. Prosthetic treatment and assessment criteria have been outlined in Table 1.
| Prosthetic Assessment Criteria |
| High attention to detail is crucial when providing appliances to any patient with an exaggerated reflex. Therefore, where current dentures are already present, the following criteria should be assessed by the clinician: |
| Prosthetic Treatment |
| Prosthetic management approaches for patients with a pronounced gagging response: |
Miscellaneous
Non-perforated impression trays will prevent extrusion of material into the oral cavity which could trigger the gag reflex (Figure 6). Rubber dam isolation is also a useful consideration as it will help prevent air spray and water from coming into contact with the high risk anatomical sites.

Other interesting approaches which, if proven effective in the literature, would certainly prove to be a fast and easy way of managing gagging patients include:

Conclusion
Once the correct underlying aetiological factor(s) and the gagging severity have been diagnosed, it will become apparent which intervention(s) should be attempted in the first instance. Initially, it is always good practice to adopt a combination of behavioural techniques, within a safe and nurturing clinical environment.
Pharmacological and non-pharmacological interventions are invaluable tools in the dentist's armamentarium. However, if appliances are necessary as a long-term prosthetic solution, or if a complex restorative treatment plan has been developed, then it is strongly recommended that the source of the patient's conditioned behavioural responses are targeted, with re-education of maladaptive thought processes.
At the present time, the evidence base with regards to gagging patients is very low. Hopefully, in the near future, further studies will be published which will contribute to our constantly evolving understanding of the gag reflex and clinicians will be provided with clearer guidelines to inform their clinician decisions better.

