Article
Cerebellar abscess with Fusobacterium nucleatum in a middle-aged man with periodontal disease
Fusobacterium nucleatum is an anaerobic micro-organism that is found only in the human oral cavity, where it co-exists with more than 500 other species.1 It causes diseases such as periodontal and soft tissue abscesses, which can spread to the brain and cause intracerebral infection.2 Infections of the brain involving F. nucleatum are uncommon but potentially severe, with many requiring surgery.3
Case presentation
Here we report a case of a 50-year-old man with a cerebellar abscess caused by Fusobacterium nucleatum that resulted in left-sided hemiplegia (Figures 1 and 2).
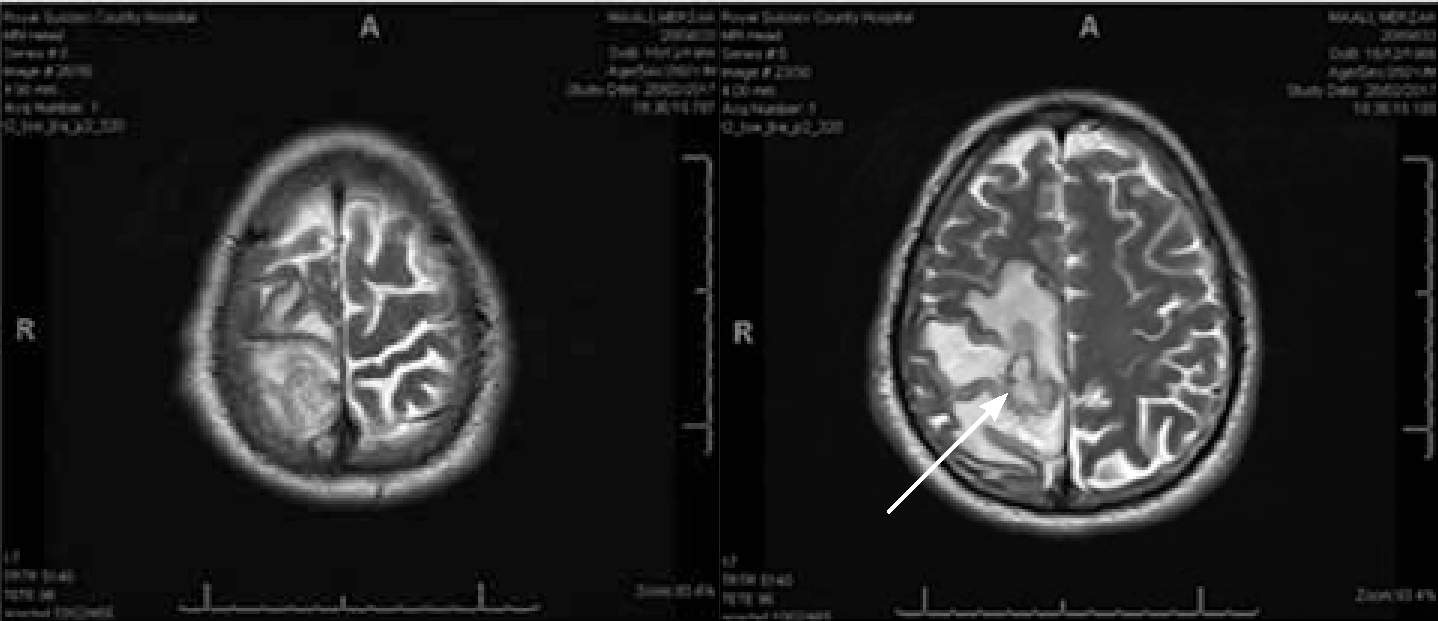

This patient presented in A&E following a fall, with left-sided weakness and pyrexia. CT and MRI imaging revealed a brain abscess in relation to the right parietal/posterior frontal lesions. This is shown in Figures 1 and 2. After 48 hours of progressively worsening left-sided weakness, the patient underwent drainage of the right brain abscess and was treated with antibiotics.
Further drainage of the abscess was needed 11 and 17 days later as the repeat MRI scan showed increasing size of the abscess. Microscopy, culture and sensitivity from the cerebral abscess cultured Fusobacterium nucleatum, which is an anaerobic bacteria that inhabits the oral cavity.
The patient was subsequently reviewed by the maxillofacial team. The intra-oral clinical examination, as well as the CT mandible 3D reconstruction shown in Figure 3, confirmed the presence of generalized periodontal disease and periapical pathology. Multiple teeth were grade III mobile with associated periapical abscesses.

The maxillofacial team performed extraction of 13 of the patient's teeth under general anaesthetic with periapical abscesses and severe periodontal disease. From there the patient improved and subsequent CT head scans revealed no evidence of recurrent abscesses.
Discussion
Brain abscess of dental origin is a rare situation but deserves attention in the dental and medical community due to its high mortality rate and potential to cause disability.4 The mechanism of spread is still not entirely known, however, a systematic review of 60 cases of intracranial abscesses of odontogenic origin found that the position of the brain abscess appeared unrelated to the side of dental involvement. This suggests that hematogenous spread is the most likely route of dissemination.5
One of the key treatments for cerebellar abscess is eradication of the primary focus of infection.6 In this case, the maxillofacial team performed extraction of 13 of the patient's teeth under general anaesthetic and the patient subsequently made an uneventful recovery.
This case highlights the importance of periodontal health as this was the direct cause of the cerebellar abscess. When the maxillofacial team discussed this with the patient he was unaware that he had periodontal disease, despite being a regular attender at the dentist. Thus the importance of both education and treatment of periodontal disease in both primary and secondary care cannot be emphasized enough.

