Article
Stafne's Idiopathic Bone Cavity (SIBC)
We would like to report on a case that was referred to our Oral and Maxillofacial Surgery department. A fit and well 40-year-old male was referred by his general dental practitioner regarding a radiolucency associated with the lower left premolar region. This was otherwise asymptomatic and the LL4 and LL5 were said to be vital. A panoramic radiograph confirmed the presence of a well-defined and corticated radiolucency in the lower left premolar region (Figure 1).
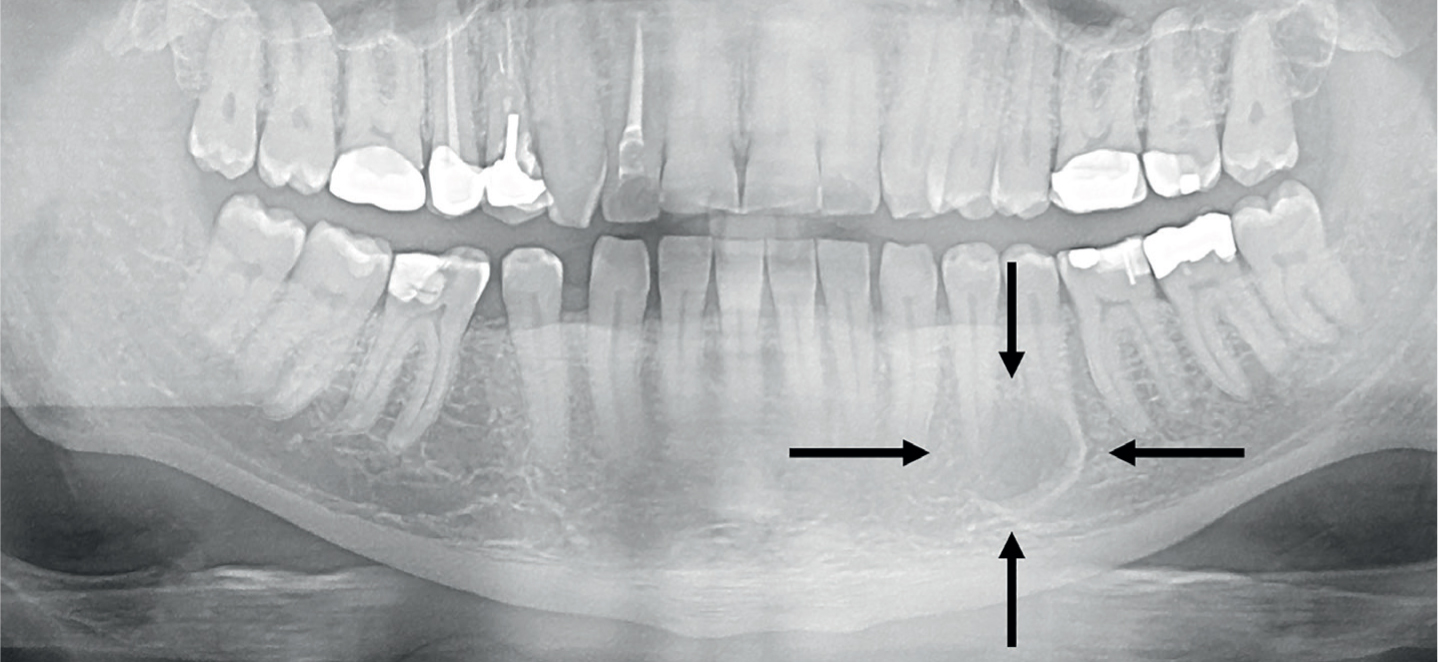
Clinically there was no intra-oral abnormality; the lower left premolars were non mobile and vital. A CT scan was requested to obtain more detail. This revealed a depression of the lingual left side of the mandible 5 x 10 mm in size with the roots of the lower left premolars just lateral to this lesion. The inferior dental neurovascular canal was sitting immediately inferiorly to the lesion. The lesion was described as potentially being a Stafne's Idiopathic Bone Cavity (SIBC). As per previous literature,1 an MRI scan was performed, so as to investigate for any involvement or pathology associated with the adjacent salivary gland tissue (likely sublingual) which could be associated with this bone defect.
The MRI scan revealed that the sublingual gland was in close proximity with the lesion, otherwise the remaining soft tissues were normal. Given this information, a SIBC was confirmed, therefore a surgical exploration was contra-indicated as this potentially could damage the premolar apices and the mental nerve for no clinical benefit.
A SIBC is a developmental defect. It has also been described as a pseudocyst without an epithelial lining.2 Their prevalence is <0.5% and they typically occur at the angle of the mandible below the inferior dental neurovascular canal3 with the appearance as described. It is postulated that they are caused by compression of the lingual cortical plate from adjacent salivary gland tissue.4 When these have been examined for histopathology, more often than not they have been found to contain salivary gland tissue.4,5 The management of a SIBC is conservative.
In summary, although unusual and unexpected, this finding should be highlighted to our colleagues, especially as SIBC in the mandibular premolar region has been described6 and therefore considered in a differential diagnosis whenever there is an apparent well corticated radiolucency involving the apices of otherwise vital and asymptomatic teeth. Although more detailed imaging will confirm the diagnosis, it may not always be necessary if the suspicion for SIBC is high.

