References
Oral rehabilitation of a patient suffering mal-union of a fractured mandible
From Volume 45, Issue 7, July 2018 | Pages 647-654
Article

Mandibular fractures normally heal by the formation of an osseous bridge between the fractured components, followed by remodelling and maturation. Inflammatory-, osteoblast-, osteoclast- and periosteal-cells all play a role in the healing process that can be simplified into four phases:
The fractured mandible experiences opposing tensile and compressive forces from the supra hyoid and masticatory muscles, respectively. Such forces may cause movement of the fractured bony portions, if inadequate fixation has been undertaken, and also influence healing at a cellular level. Whilst tensile forces encourage bone deposition via osteoblasts, compression forces initiate osteoclasts and subsequent removal of bony matrix.
The anatomic location of mandibular fractures varies (Table 1), with several studies demonstrating that the site of fracture correlates with mechanism of injury.1,2 Whilst anterior forces, such as in a head-on motor vehicle collision, will usually result in fracture of the symphysis and condyle, applied lateral forces (eg from a punch) will likely result in fracture of the angle and body of the mandible.1,2 Other contributing factors to mandibular fracture include:
| Coronoid | 2% |
| Alveolus | 3% |
| Ramus | 3% |
| Symphysis | 14% |
| Angle | 20% |
| Body | 21% |
| Condyle | 36% |
Mandibular fracture can be managed both non-surgically and surgically, with the approach often influenced by both patient (systemic illness/age) and local (severity and displacement of the fracture) factors. Treatment aims to encourage primary bone healing without excessive callous formation and is normally achieved via reduction of the fracture followed by rigid fixation to approximate and immobilize the portions of the bone.
Mal-, or non-union, of the mandible occurs when the fracture heals via fibrous tissue and will often present with infection at the fracture site or mal-occlusion. Such problems are normally associated with factors that include: severe fractures with extensive displacement, failure to align the bony fragments adequately during reduction, failure to achieve stability through fixation and post-operative infection1,2 (Table 2). Despite advances in the treatment of mandibular fracture, the incidence of mal-union has remained relatively unchanged, with a reported range of 0.8%4 to 2.8%.5
| General Factors | Local Factors |
|---|---|
| Alcohol Abuse | Severity of injury including the presence of multiple fractures |
| Diabetes Mellitus | Delay in treatment greater than 5 days |
| Osteoporosis | Tooth in presence of fracture line |
| Morbid Obesity | Surgeon experience |
| HIV | Osteomyelitis/infection |
| Atrophic mandible (edentate) |
Various techniques to correct mal-union surgically have been described, with high success rates reported.6,7 However, should surgical correction fail to achieve bony union, permanent instability or movement may occur between the two parts of the fractured mandible. The stresses instigated by such movements may lead to prosthetic dental complications, such as de-bonding, or fracture, of restorations and may be particularly pertinent when a fixed prosthesis bridges the fracture line. Presently, there is little information available for the clinician seeking to provide a fixed restorative solution for patients suffering mandibular mal-union. This case report details the rehabilitation of a patient using a combination of upright- and distal-angulated dental implants to negotiate the mal-union within a fractured mandible and the construction of a fixed-supported prosthesis.
Case details
A 62-year-old female patient presented with failing maxillary- and mandibular-fixed bridgework that prevented her from eating solid foods or smiling in public. The bridges had been placed over 20 years previously, following severe dental and oro-facial injuries suffered during a road traffic accident (RTA). This injury had resulted in fracture and mal-union of the left mandible (Figure 1) and paraesthesia of the left lower lip. An attempt at corrective surgery to join the mandible, 10 years previously, had been unsuccessful. The patient had subsequently been restored using conventional fixed bridges but these structures now had a history of repeated de-bond and, on examination, were found to be supported by carious, periodontally-compromised abutments (Figure 2).


A course of cause-related therapy was employed to stabilize the patient's periodontal disease and the bridges were systematically removed to confirm poor restorative prognosis of the abutments. The patient was only willing to accept a fixed restorative solution and it was decided to proceed with a plan that involved extraction of most of her dentition with rehabilitation using dental implant-supported bridges. The plan involved three phases.
Phase 1
The patient's existing fixed conventional bridgework had a sub-optimal occlusal scheme and was set at a vertical dimension that provided insufficient space for a natural-looking dentition. A diagnostic wax-up of the patient's articulated study models was used to plan new prostheses at an increased vertical dimension, seeking to change both the appearance and inter-arch occlusal relationships. The wax-up was also used as a guide to assist with the construction of immediate removable partial dentures (RPDs) at an increased vertical dimension.
Following removal of the fixed bridges, the unrestorable teeth were extracted, leaving second molars and the UR6. Provisionalization of the patient was achieved using immediate RPDs, fitted at the time of extractions. These appliances were used to gauge the patient's tolerance of the increased vertical dimension (Figure 3).

Phase 2
Following a period of adaptation, a Cone Beam Computerized Tomographic (CBCT) image was utilized to examine the feasibility of implant placement in the maxillary and mandibular arches. Radiographic stents, manufactured using a copy denture technique, were used to clarify the position of the intended prosthetic structure in relation to the mal-union and the residue debris that can be seen in Figure 2.
Within the upper arch, six dental implants (3i BioMet Parallel Osseotite®, Palm Peach, Fl, USA) were planned to support a cross-arch bridge. There was insufficient vertical bone height within the posterior right alveolar process for implant placement, and right maxillary sinus augmentation with localized alveolar ridge augmentation, using bovine bone (BioOss®, Wolhusen, Switzerland) and a screw-retained porcine-derived collagen membrane (BioGide®, Wolhusen, Switzerland) was undertaken at the time of implant placement (Figure 4). A conventional two-stage surgical approach with delayed-loading was adopted. The implants were restored using multi-unit abutments and the RPD was converted chairside into a provisional acrylic bridge.

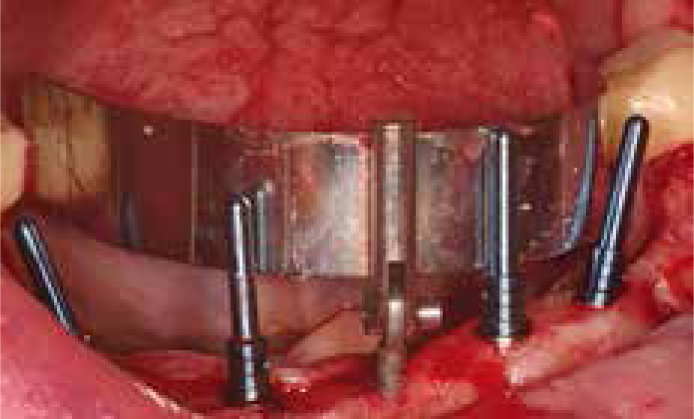
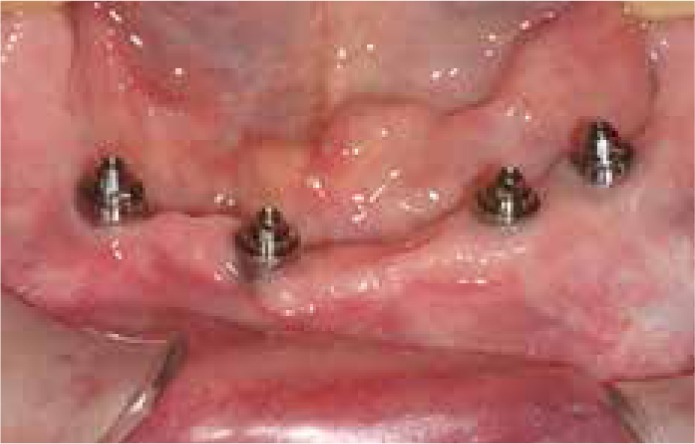
Four dental implants were planned for the lower arch (3i BioMet Tapered Certain Osseotite®, Palm Peach, Fl, USA). The posterior implants were distally angled to compensate for both the position of the mental nerves and the fibrous union of the left mandible. The implants were placed using a Nobel All-on-4® template (Nobel Biocare®, Zürich-Flughafen, Switzerland) (Figure 5). Multi-unit abutments were placed to correct the angulation and the implants (Figure 6) were immediately loaded with an acrylic bridge, which was constructed via conversion of the RPD (Figures 7 and 8).



Phase 3
Definitive restoration of the maxilla and mandibular implants was planned using Computer Aided Design/Computer Aided Manufacture (CADCAM) milled titanium bars and an acrylic overlay (Figure 9). The second molars and UR6 were restored with single unit crowns. Review at two years post dental implant placement found the bone levels to be stable (Figures 10 and 11).


Discussion
Although the instance of mal-union of the mandible is low and high success rates3 are reported for surgical correction, treatment for this patient's mandibular fracture had not been successful. To the best of our knowledge, there is little in the dental literature that discusses the management of mandibular mal-union using either conventional restorative therapies or dental implants.
Although not practical in this case, theoretically, dental implants could have been placed on either side of the mal-union. However, the functional movements of the adjacent parts of the mandible may have caused stress within the implants and supra-structure. In addition, rigid splinting of the mandible with a cross-arch implant-supported prosthesis may negatively affect both implant bone levels and cause chipping or fracture of the prosthetic supra-structure8,9 as the mandible expands during opening.10,11
Alternatively, placing upright paralleled implants mesial to the mandibular abnormal-union would have led to distal cantilevers with considerable extension and longer than the recommended 15 mm maximum length.12,13 Distal cantilevers have the potential to act as Class I levers during function, resulting in complications such as bone loss around the dental implant and either implant or suprastructure fracture.13,14
The use of two dental implants placed upright anteriorly and two angularly tilted implants posteriorly, commonly referred to as an All-on-4® approach, aims to restore the edentulous arch immediately with a fixed implanted-supported acrylic bridge.15 The retention of the second molars means that was not a true All-on-4® case but provided the benefits of continued tooth proprioception that should assist with reducing the occlusal load on the implant-borne supra-structures.16
An All-on-4® guide (Nobel Biocare®, Zürich-Flughafen, Switzerland) was used to assist with the correct angulation of the implants. Alternatively, stereolithographic surgical stents may be useful with the undertaking of these cases as they facilitate implant placement that accurately corresponds to the restorative plan and may reduce the risk of damage to anatomic structures, such as the inferior dental nerve.17,18 In addition, these guides usually employ a tissue punch to access the underlying bone, as opposed to the conventional raising of full thickness mucosal flap, and this may reduce both post-operative morbidity19 and the duration of the procedure.20
Other advantages advocated with the All-on-4® approach include: reduced requirement for invasive bone augmentation procedures such as sinus floor elevation procedures; the cost-effectiveness of using fewer implants to retain a full-arch prosthesis; and immediate loading and time efficiencies with full-arch restoration. Within the mandible, angulation of the distal implants mesially allows longer length implants to be used, which in theory facilitates better bony anchorage without increased risk of damage to the inferior dental nerve.15
It has been hypothesized that the All-on-4® approach improves stress distribution and reduces flexure of the supra-structure, allowing acrylic to be employed as a cross-arch fixed restorative material.21 Whilst acrylic was employed as the sole prosthetic material in the immediate provisional prosthesis, the definitive bridge was reinforced with a CADCAM milled titanium substructure that provided increased strength and support to the acrylic finish. A plethora of CADCAM bar designs are available for the clinician/technician to adopt within cross-arch dental prostheses. In principle, the substructure should be designed to follow the contours of the underlying arch ridge, whilst providing clearance space (normally 0.5–1.5 mm) and convex contour to aid cleansibility, and sufficient support for the desired overlying material. Although titanium is commonly employed as a substructure, due to its strength, biocompatibility, high polish and lightweight properties, other materials have been employed and include; gold, cobalt chromium and zirconium. Advantages of using acrylic or composite as the overlying material include their relatively low cost, stress absorbance and good aesthetics. Although prone to chipping and wear,9 these materials can be stripped and replaced relatively simply, reducing the expense of future refurbishment of the substructure. Alternatively, porcelain may be used to provide optimal aesthetics, although this incurs greater expense and, in theory, increases applied stresses to the implants and substructure via transfer of occlusal loading forces.22
The All-on-4® approach has been widely studied with survival rates of over 95%,15,23,24 and compares favourably to conventional approaches.25 Within this case, an upright/tilted implant approach facilitated placement of sufficient implants to support a fixed prosthesis without bridging implants across the abnormal-union.
Conclusions
This case report details an effective means of rehabilitating a patient with mandibular mal-union using a modified All-on-4® dental implant approach to support a prosthesis.

