References
An alternative approach to replacement of an avulsed central incisor
From Volume 45, Issue 3, March 2018 | Pages 215-225
Article
When an avulsion injury occurs in a permanent maxillary incisor, ankylosis often occurs. In order to restore aesthetics and function, dental treatment is required.
Avulsion is classed as complete displacement of a tooth from its socket.1 Ankylosis is frequently a sequela following avulsion injury. The determining factor in whether a tooth becomes ankylosed after avulsion is the health and status of the periodontal ligament (PDL) after injury. Minimal damage and disruption to the PDL reduce the chances of ankylosis. There are three main factors that have the strongest impact on PDL:
Optimal conditions are considered to occur when the tooth is re-implanted immediately following injury and has an open root apex. The risk of ankyloses injury in this case is approximately 12% after 5 years.3 Suboptimal conditions are considered to occur when the tooth has been out of the socket for over 5 minutes, not stored in a physiologic medium, such as saliva, and has complete root development.
Following avulsion, the approximate risk of ankylosis is 74% after 10 years.3 If ankylosis does occur, the clinician will then need to manage the rehabilitation of the tooth through prosthetic or restorative means. The clinical signs of ankylosis, particularly in a growing patient, are infraocclusion and a high pitched sound upon percussion of the tooth. Radiographically, replacement resorption is often seen. If this situation is not detected early, complications from ankylosis include loss of vertical alveolar bone height, tipping of teeth and acute periapical periodontitis.4,5
When faced with the loss of a central incisor, due to avulsion/anklylosis, the principles of management are immediate replantation, application of a flexible splint for up to two weeks and initiation of root canal treatment 7–10 days after replantation and before splint removal.
The factors to consider when treatment planning a patient with an ankylosed tooth are:
This clinical case report examines these factors and considers an alternative approach to replacing an avulsed central incisor.
Case report
Patient HG first attended in October 2012. Her presenting complaints were that she was missing her UR1, use of an upper partial denture, and that she felt that her upper canine tooth ‘stuck out’. Patient HG was wearing a partial acrylic denture (spoon denture) at the time, with which she was unhappy due to lack of retention, poor aesthetics and social embarrassment. The UR1 had suffered an avulsion injury 3 years previously and the tooth was re-implanted by her dentist after an extended extra-oral time of one hour. Unfortunately, this tooth became ankylosed and had to be extracted in August 2012 to prevent further loss of alveolar bone height and recurrent infection.
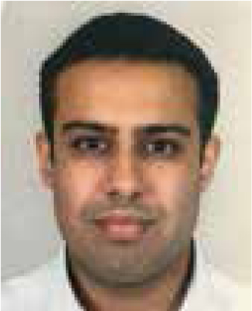
Orthodontic examination showed that the patient had a mild Class II skeletal base with a Class II division 1 incisal relationship. The overjet was measured at 5 mm with an average overbite. The upper arch showed moderate crowding with the UL3 having contact point displacement of 6 mm. There was average inclination of the upper incisors. The lower teeth presented mild crowding of 3 mm, retroclination of the lower incisors, a moderate curve of spee and a lower centreline shift to the right by 3 mm. The lips were competent at rest, with full incisor show on smiling. Buccal segments were ½ Class II on the left-hand side and ¾ Class II molar on the right-hand side. The IOTN was 4d, due to the displaced canine (Figures 1 and 2).

As this was a complex case with many treatment options, following the orthodontic examination, the patient was subsequently seen at a joint orthodontic and restorative clinic. This allowed for a full discussion of all treatment options to allow the patient and parents to make an informed choice with the help of a multidisciplinary team.
It was concluded that the UR1 had experienced replacement resorption, hence its subsequent extraction. Irregular gingival contours and a significant palatal concavity with a rather unusual midline palatal fissure indicated that implant placement would be difficult without careful planning and bone grafting.6 The defect in the alveolar ridge would have also made replacement using a resin-bonded bridge aesthetically challenging. The various treatment options were discussed and a final treatment plan was decided upon.
Options
1. Extraction of UL3 and no further treatment
Although this was an option it was not appropriate as this plan would not address the patient's concerns, and would leave her with an unsatisfactory partial denture.
2. Extraction of UL3, fixed appliances upper and lower arches to maintain space for prosthesis
Prosthetic replacement could involve the use of a resin-bonded bridge or partial denture before implant placement. When the patient is 18, a dental implant placement could be considered. Alternatively, a resin-bonded bridge as a definitive restoration of the UR1 space could be used. In regard to the resin-bonded bridge, there are several factors that need to be considered for the bridge to be successful, including careful case selection, bridge design and clinical technique.7 Due to the patient's vertical ridge defects, replacing the soft tissue using a bridge becomes difficult. Pink porcelain or composite can be used to replace soft tissue. However, the restoration often becomes bulky and can compromise oral hygiene.7 The provision of either a bridge or implant in the space would be technically difficult with limited survival and success rates in a suboptimal site, as highlighted in the joint clinic discussion.
3. Autotransplantation of the UL3 or UL5 into the UR1 space, fixed appliances upper and lower arches
Autotransplantation is defined as the movement of one tooth from one position to another, within the same person.8 When implant placement is not a viable option, for example in a patient under the age of 18, autotransplantation of an immature tooth can be considered an option. It has been previously reported in the literature that autotransplantation with space closure may represent a viable aesthetic result.9
Ideally, transplanting the UL5 into the UR1 space would preserve upper arch symmetry, and allow alignment of the UL3, utilizing space created by extraction distally to the canine. If the UL5 was lost in the future, bone would have been preserved for implant placement once growth had ceased. Transplanting the UL3 would reduce orthodontic treatment time. However, this would also leave a small compromise in aesthetics due to asymmetry.
There are several criteria that have to be met for autotransplantation to be a viable option. These include donor tooth criteria, recipient site criteria and careful patient selection. Ideally, the donor tooth chosen for transplantation should have two thirds of its root developed with an open apex. This provides the tooth with the potential for pulp regeneration in the transplant site (apex opening >1 mm radiographically).8 Unfortunately, in this case, all the patient's premolars were fully formed with practically closed apices (Figure 2), and so this treatment modality was deemed to have a low chance of success. The lack of bone, labially in the UR1 region, was a further reason that the success of autotransplation was doubted.
The success of autotransplantation is largely down to the technical skill and experience of the surgical team. Whilst our surgical team have experience in this treatment modality, they felt that to attempt autotransplantation in this case was too complex to guarantee success.
4. Extraction of UL3, fixed appliances in the upper and lower arches to close space and camouflage the UR2 as an UR1
This plan also incorporated camouflage of the UR3 in the UR2 site and both first premolars as canines with composite build-ups, if required. The aim would be to put the first premolars in a Class I canine position and to finish with the molars in a full unit, Class II relationship. This option removed the need for placing the prosthesis in a suboptimal site and would reduce the short- and long-term costs for the patient and the National Health Service. It also allowed re-establishment of the alveolar ridge by means of migration of the UR2 through orthodontic tooth movement. Extraction of the UL3 would also shorten treatment time.
Option 4: Treatment
Option 4 was chosen and the finalized treatment plan was carried out as follows:
Treatment progression
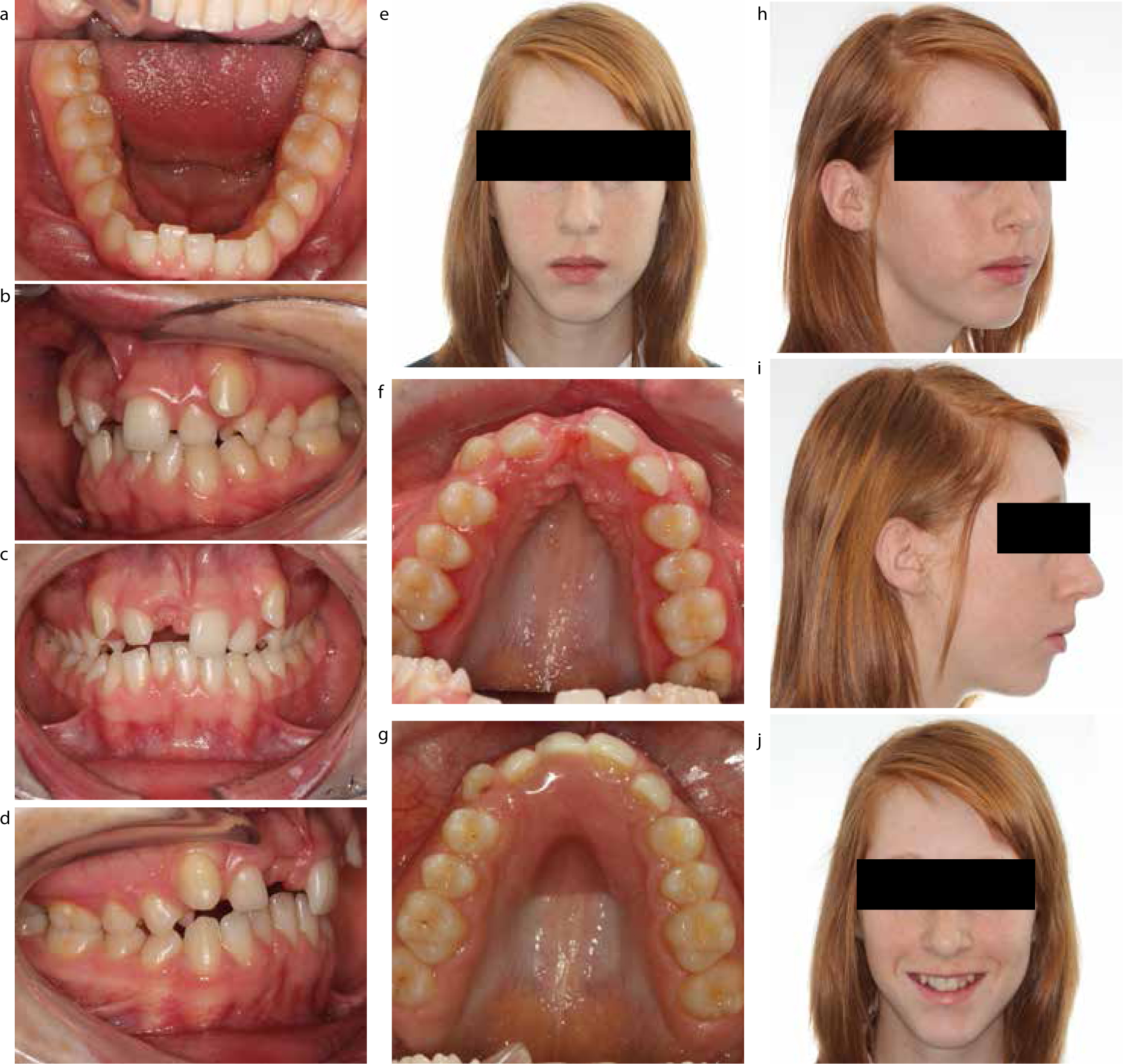
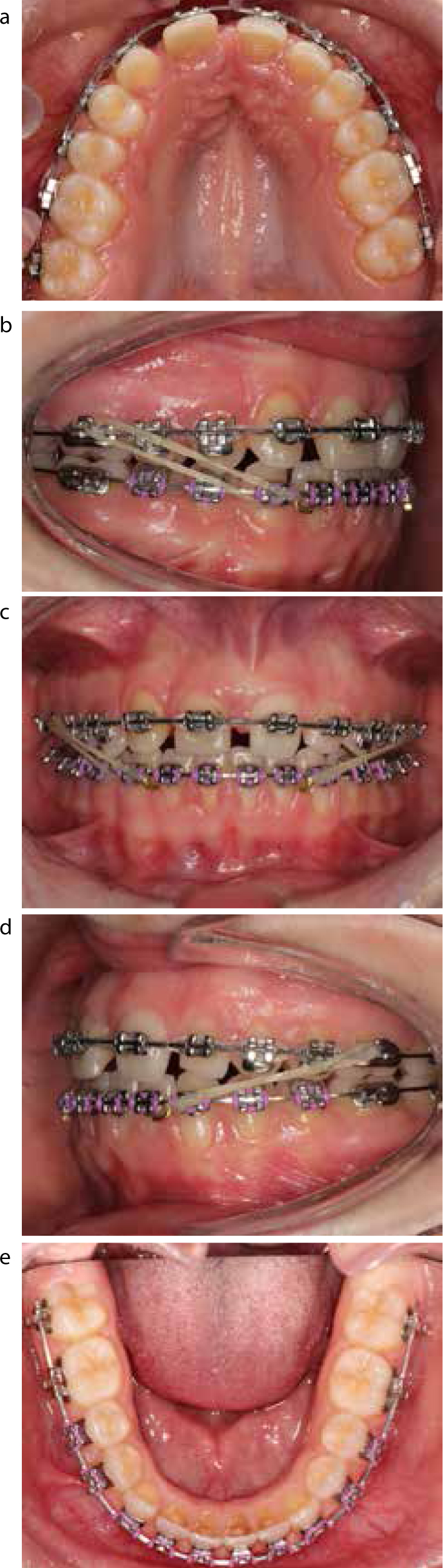
Treatment started in June 2013 and began with initial alignment with 0.016” nickel titanium archwires. The UR3 was inverted to change the torque from -7 to +7, to reduce the prominence of the canine root labially (Figure 3).
Rectangular 18/25 nickel titanium archwires were used to continue to level and align the teeth until working stainless steel 19/25 archwires could be placed (Figure 4).
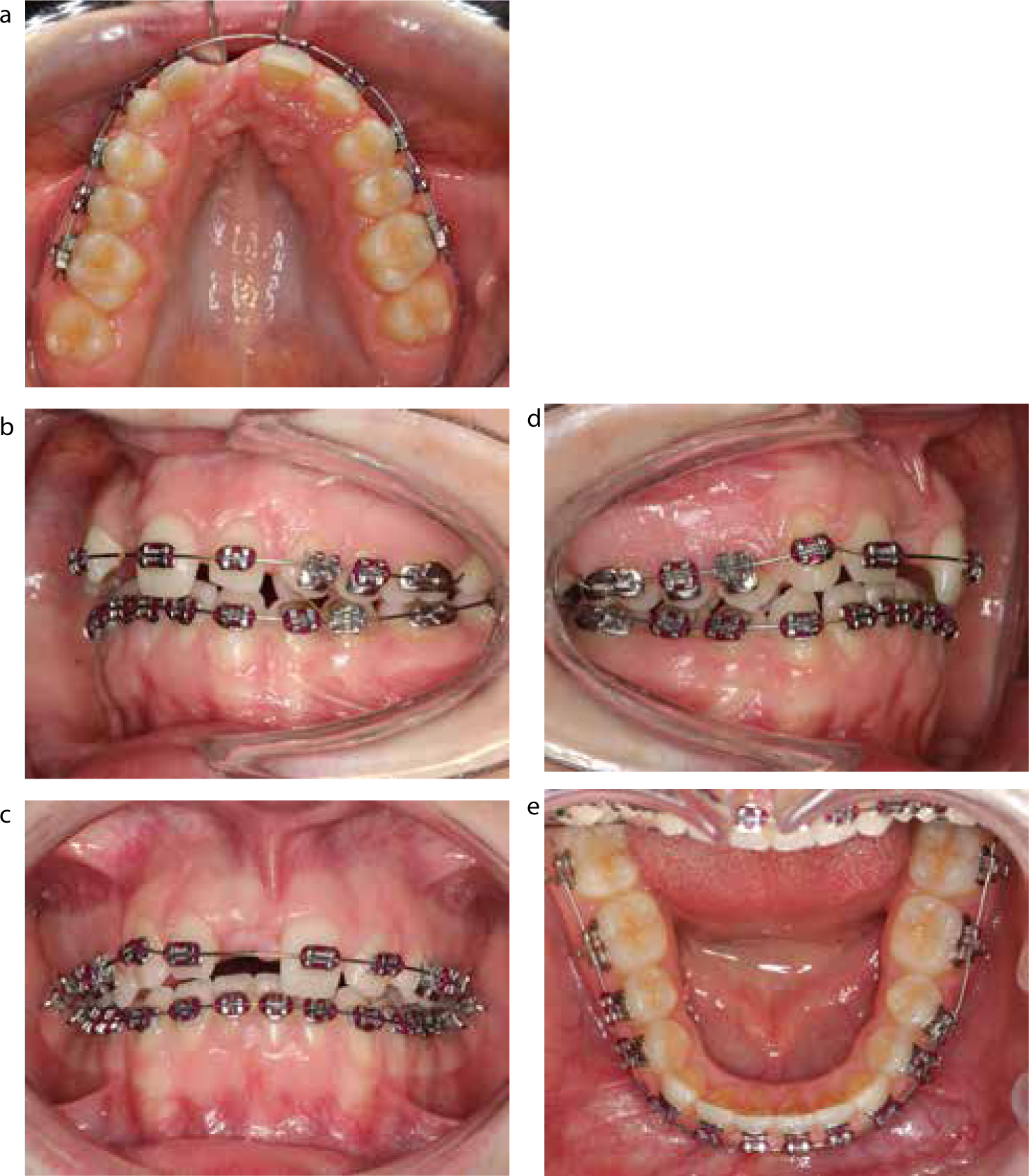
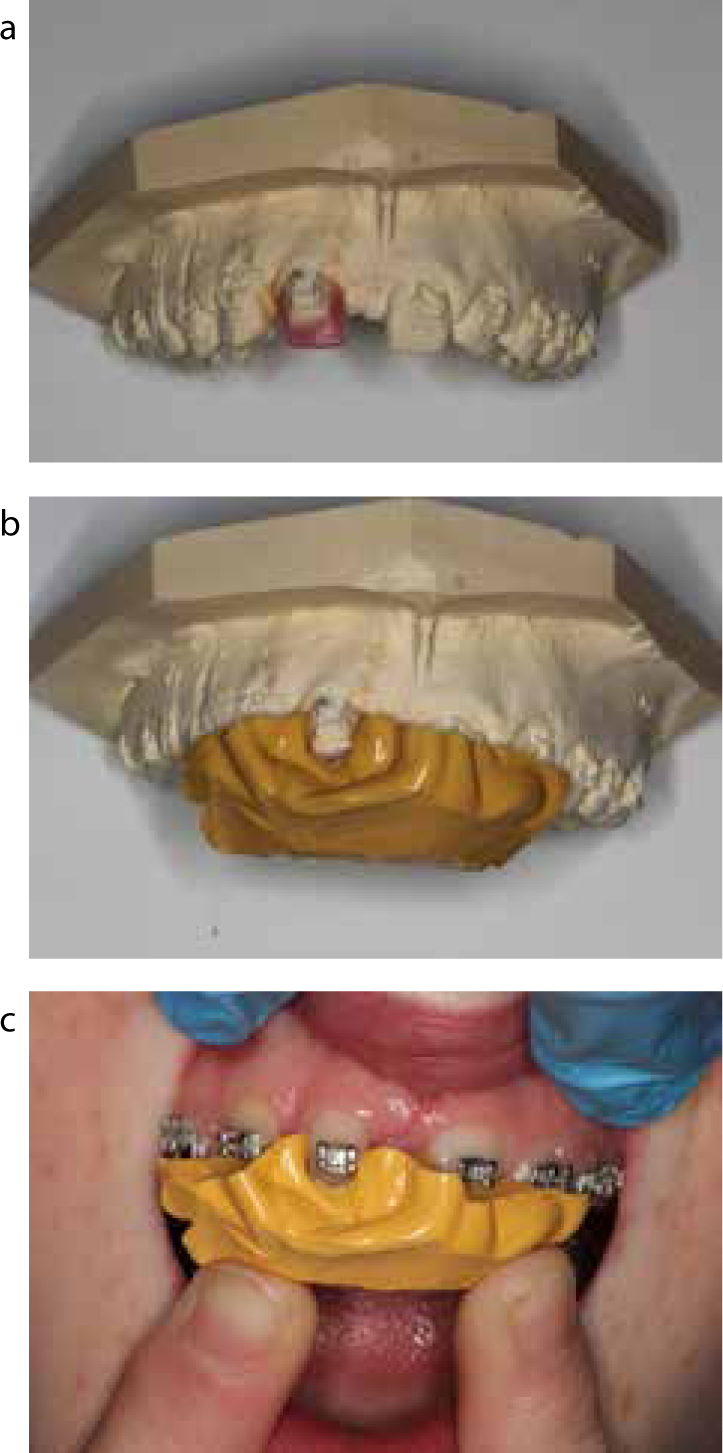
The next stage of treatment was to place nickel titanium push coil between the UR3 and UR2 to migrate the UR2 towards the midline. When space had been created mesially and distally around the tooth, an alginate impression was taken of the upper arch with the archwires removed. The wire was replaced and the position of the UR2 was held exactly by placing stainless steel tubing, either side of the tooth, on the archwire. This impression was used to provide a kesling set-up and build the UR2 to a relative size to the UL1. Once the clinician was happy with the mock up, a medium-bodied silicone impression material (vinyl polysiloxane) was used to create a stent, which could be used intra-orally to build the tooth up in composite (Figure 5).
Space has been created mesially and distally between the UR2 due to the push coil. The UR2 was built-up palatally, incisally, mesially and distally but not labially due to the attachment of the bracket to enamel. The tooth was prepared in the usual way and Herculite XRV™ (Kerr, Orange, CA, USA) enamel and dentine composite was used to build the tooth up. The build-up was finished with green and white stones and Sof-flex discs (Figure 6).

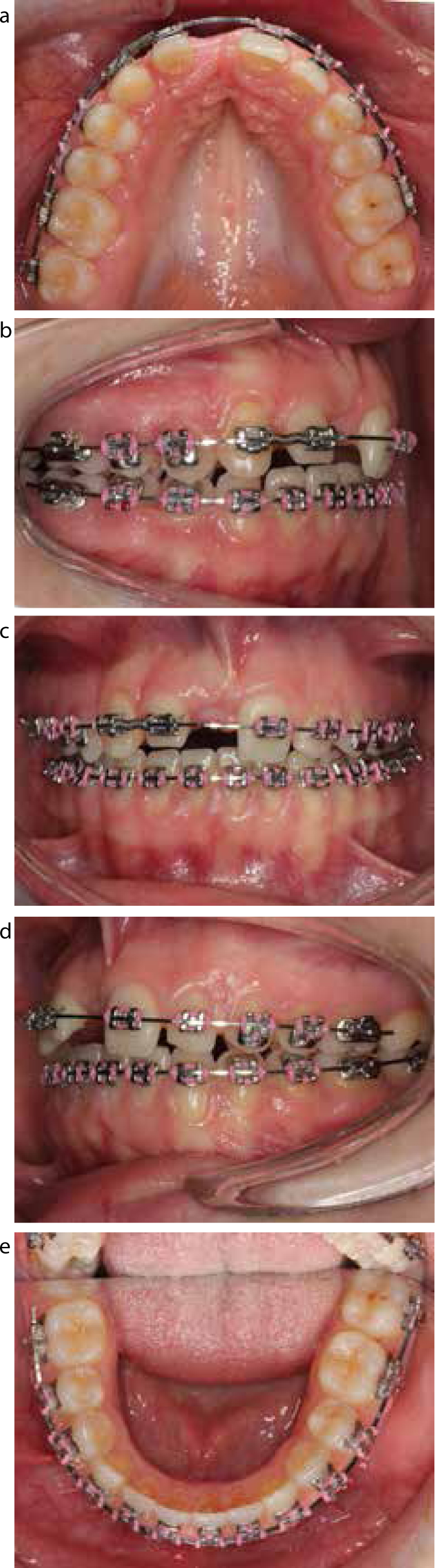
Now that the UR2 was a size relative to the UL1, the remaining orthodontic treatment involved upper centreline correction and complete space closure in the upper arch. This was achieved by the use of a power chain on an upper 19/25 stainless steel archwire. To allow mesial movement of the upper buccal segments and prevent reduction of the overjet and overbite, the patient was instructed to wear Class III elastics 24 hours a day. Final detailing and finishing was completed on round stainless steel archwires (Figure 7).
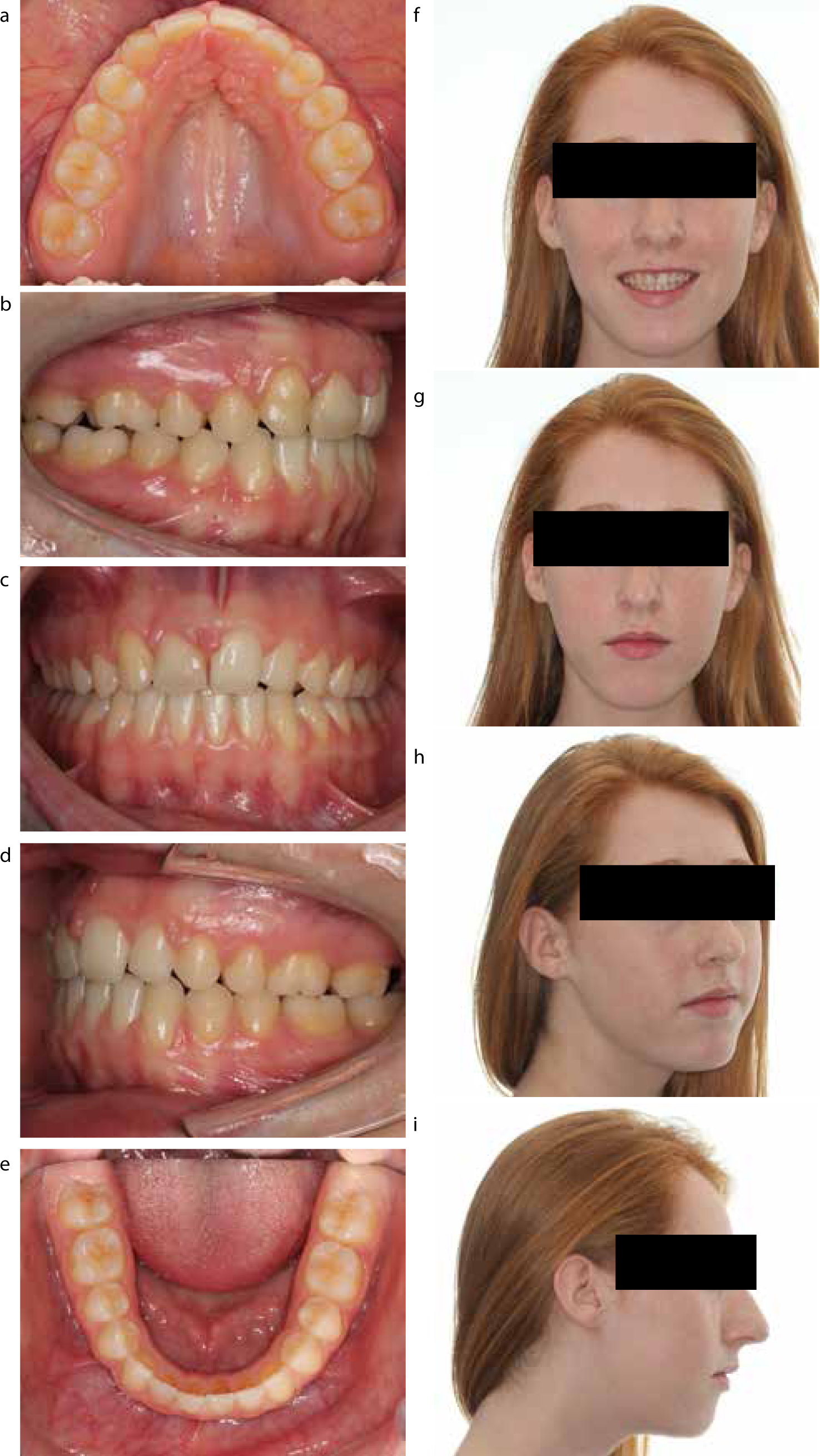
The patient was debonded after 2 years of orthodontic treatment with the occlusion and facial appearance as in Figure 8.
Discussion
This case is a good example of an effective method to treat a patient who has suffered ankylosis with bone loss following an avulsion injury in childhood. Avulsion injuries are more common in patients with a large maxillary overjet, according to the literature.10 There are many advantages of using orthodontics and direct composite bonding to restore a patient's dentition. A primary advantage is that it is a cost-effective option in the short- and long-term. There are no initial implant/bridge costs for placement and no costs associated with implant/bridge management and future replacement. The cost of a bridge on the NHS is currently priced at £244.30.11 Dental implants are often not provided on the NHS and the average cost of an implant in the UK is currently between £1500 and £4000.12
This treatment has been minimally invasive, utilizing the patient's remaining dentition to provide a good aesthetic result and restore alveolar bone in the UR1 position.
From a critical perspective, the upper centreline is to the right by approximately 1.5 mm. This may have occurred due to the asymmetric arrangement and size of teeth in the upper left and right labial segments. Considering the overall result, it was felt that this was acceptable and unlikely to be noticed by members of the public.13
The authors note that symmetry was not preserved in this case, however, they feel that this has been adequately camouflaged. In hindsight, a superior aesthetic result may have been achieved by extraction of the UL2 instead of the UL3. This would have left the patient with both maxillary canines in the lateral incisor positions, creating a more symmetrical finish. Relapse potential of aligning a high buccally positioned canine would have to have been considered during the consent process.
Ideally, the UR3 would benefit from bleaching and build-up in the future to achieve a more aesthetic result. The patient's low smile line masks the higher gingival margin of the UR3 compared to the UL2. Careful monitoring of the UL2 build-up by the GDP is essential to ensure that good gingival health is maintained.
Using composite build-ups to alter tooth morphology to resemble the UL1 counterpart has enabled a minimally invasive treatment plan where there was little need for tooth preparation. The patient has the option to have further restorative dentistry performed, if desired.
Conclusion
In this case, the orthodontic team have been able to work closely with their restorative colleagues to provide the optimal treatment for the patient, which has been both cost-effective and has provided an aesthetic end result.
Avulsion injuries can be very traumatic for children and it is important to re-implant the tooth as soon as possible. If ankylosis does occur, classically, there are several options to replace the tooth via prosthesis. This case has provided an alternative treatment plan to restore the space created due to a lost tooth.

