Article

In the last Comment,1 I contended that, not only were Prototype dentists being left ‘high and dry’ on 31st March 2022, but also, potentially, their patients. I then went on to add that perhaps NHS dentists in general might be treated in a similar way at some other time. Just after writing that Comment, in which I expressed worries about the numbers of dentists who are considering getting off the treadmill, about the stress levels reported by NHS dentists and about the excessive time taken to NOT get a new Contract organized, there was a well-timed media offensive by the BDA bringing to the public's attention the lack of progress on a new contract, the poor morale of many NHS dentists, and the fact that many were retiring (early, in some cases) or simply leaving the profession. The Government's response to comments made in the House of Commons was that there were adequate urgent dental centres. The subject was, by coincidence, covered at around the same time, by Stephen Hancocks, in a superb BDJ Editorial entitled ‘I worry’, in which he eruditely mentioned young dentists and the prospect of life shackled with UDAs and the pressures of the need for onerous personal protection.2 Both of us painted a picture of a profession at the crossroads, and neither of us had practical answers.
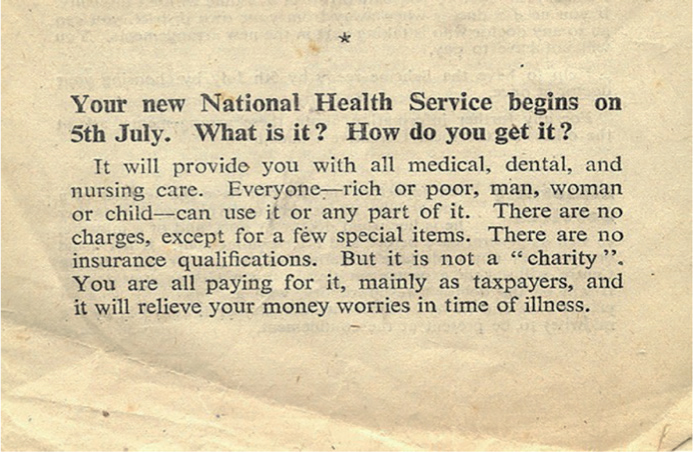
Perhaps it is worth looking at how it all began. At the inception of the NHS in 1948, there was a vast reservoir of untreated dental need. So, with the arrival of a free dental service (Figure 1), the demand for dental care on the new NHS was overwhelming, with dentists reportedly going from seeing around 15–20 patients per day to over 100.3 In the first 9 months of its existence, NHS dentists provided over 33 million artificial teeth.3 In the same period, there were 4.5 million extractions, with approximately the same number of fillings. Needless to say, as demand increased, so did dentists' incomes, and with the NHS becoming a more attractive proposition by the end of 1948, 83% of practising dentists had signed up. The objective of the service was that more patients would be treated, and this happened, but, as fees followed treatment, the cost ballooned and within 2 years of launching NHS dentistry, the government cut the rates of payment three times, without any consultation with the dental profession. Moreover, by 1951, the NHS was running short of money, hence patient charges were introduced, the first for any type of NHS treatment: it remains thus to the present day. Older readers (perhaps all readers) will not need much prompting to see the similarities in the beginnings of NHS dentistry to what has happened for the ensuing 74 years: today seems little different.
After writing the last editorial, I then had a dream, or was it a nightmare? As dentists leave the NHS, as they are indeed entitled to as independent contractors, patients may be left without a dentist to provide their treatment, particularly as the ready-made supply of labour from Europe has disappeared after Brexit. For the dentists who have decided that NHS dentistry is not for them, and have decided to go down the private route, be it private capitation or private fee-per-item (and they will not have taken that action to see more patients), they will effectively disenfranchise a proportion of their patients who will not be able to, or be prepared to, pay the increased (but more realistic from the profession's viewpoint) fees. Who will get the blame for this in government? The greedy dentists. As I write, the number of dentists on the Register has been the same, give or take, over the past 3 years, so the tipping point at which dentists are leaving the profession does not yet appear to have been reached. On the other hand, given the rigours of working in a pandemic and the reduction in patient throughput, the same number of NHS dentists will not achieve the same treatment output as they did prior to 2020.
Add to that, as a proportion of dentists have elected to go private, or retire, or leave to do something different, a point will be reached at which the critical mass to provide a meaningful NHS dental service will be breached, with little chance of the gaps being filled, given the dearth of new graduates and the difficulties in readily recruiting from overseas. My bad dream continued: there are several things that can happen:
- As the number of dentists prepared to work in the NHS decreases to make the system unviable, NHS dentistry will become a core/urgent treatment service so that ministers can tell themselves that no patient will be left in pain or with an acute swelling and will try to fool the public into thinking that their dental needs will be catered for, given that it has been stated, by the Chief Dental Officer England, Sara Hurley, that there are over 600 urgent dental health hubs in existence (even if a substantial proportion of those were existing practices who were prepared to treat emergencies during the first lockdown and that still remain a designated urgent hub). Saving in £s will be substantial, given that the cost of dentistry 3 years ago was quoted as being, £7.1 billion per year – of which NHS market share was circa £3.5 billion.4 At a time when Government will soon have to start thinking about saving money by cutting spending, this might seem an attractive proposition, even if it does not compare with the £billions wasted in unusable PPE, unusable beds in Nightingale hospitals and fraudulent claims for benefits. In addition, some in Whitehall may be tempted to discuss whether the loss of NHS dentistry, as we know it, would cause the Government to lose an election.
- A second scenario is that fees will increase to realistic levels and the dreaded UDA system is abandoned, but the signs that that will happen are not yet on the horizon, given the abandonment of the Prototypes project. Is the recent announcement of an additional £50 million NHS funding (albeit, by my calculation, a small proportion of the total budget) the start of some support for NHS dentistry? The scheme in which these monies will be used will involve weekend/out of core hours working, with dentists being paid one-third more than their normal fee. Is this a dream, I ask? Where might the dentists come from to staff this service? Do readers detect any similarities to the early days of NHS dentistry?
- There is always a chance that I am wrong and that nothing, or, alternatively, something novel, will happen. There has been a degree of inertia concerning UDAs and pay cuts for years, hence the tardiness by which any changes have been considered, possibly because only a few patients and dentists were complaining until recently, and the Government was content that, in 2006, it had achieved what it wished for, namely, a cash-limited scheme. However, I cannot see this scenario playing out because of the increasingly widespread discontent in the profession and the excellent performances of the BDA in drawing the public's attention to NHS dentistry's problems.
I almost quoted the famous football manager Sir Alex Ferguson's actual phrase, which referred to the sound made by moving around in a plastic seat while squirming under pressure in the moments of a close game or season! I feel that it is the same for NHS dentistry. Something has to be done as we run out of time, and potentially, NHS dentists. For the good of our NHS patients and NHS dentists, I hope that a satisfactory, properly funded new contract will arrive, sooner rather than later. But, I fear that my dream may have become the nightmare of the demise of NHS dentistry, and what happened in 1948 will go into reverse. In that regard, readers who wish to learn more about the history of NHS dentistry should read the excellent reference 3 and its associated material in full, published by the BDA.
PS I apologize to readers outwith England for two Comments, which may not relate totally to them, but, perhaps there are lessons to be learned everywhere.
PPS As we go to press, I have just read David Westgarth's excellent and well reasoned article5 ‘Is NHS dentistry being privatised by stealth?’, expressing anxieties on a similar topic to this Comment.
Welcome to Dr Pynadath George BDS, MFDS, MSc RestDent, MScImpDent, DClinDent OralSurg

I am delighted to welcome Dr Pynadath George (or ‘George’ as he is commonly known) to the Editorial Board of Dental Update. This is especially relevant as the volume of articles on the subject of dental implants increases, given that George is a dental surgeon who has a practice limited to implant dentistry and all aspects of prosthodontics and associated surgery.
George graduated from Liverpool University Dental School in 2004, completing his membership exams from the Royal College of Physicians and Surgeons, Glasgow shortly afterwards. Subsequently he completed a Masters Degree in Restorative Dentistry from the Eastman Dental Institute, UCL, and a further Master's degree in Dental Implants from Warwick University Medical School. His academic training culminated in a 3-year full time doctorate degree in oral surgery at the University of Edinburgh.
George previously worked as an associate specialist in Preston Royal Hospital treating cancer patients for removable and fixed prosthodontics, but more recently he has gone back to his roots and is currently teaching surgical endodontics and implant dentistry in Liverpool University Dental School to postgraduate trainees. George currently also works as a clinician providing implants and mentoring dentists in a number of practices in Scotland, England, Wales and Ireland. In addition, George has been the treasurer for the Association of Dental Implantology (ADI) for the past 4 years, and has been on the executive board for the past 6 years.
I am delighted that George has agreed to join us as I am certain that his knowledge in the field of dental implants will complement the knowledge, wisdom and expertise already present in the Editorial Board of Dental Update.

