Article
An interesting case of nicotine-induced leukoplakia
A 44-year-old male patient was referred to the oral and maxillofacial surgery (OMFS) unit by his general dental practitioner on an urgent basis in relation to a non-resolving, persistent white lesion in the lingual sulcus, adjacent to the lower left second premolar/lower left first molar, which was noticed at a routine dental check-up.
The patient was medically fit and well, with no known drug allergies. He was moderately active and worked a job that required a moderate level of baseline fitness. He reported an alcohol intake of around 8–12 units weekly. He had stopped smoking around 14 years previously, having been smoking around 10–12 cigarettes daily for 15 years.
Although not actively smoking, the patient reported craving a cigarette upon consuming alcohol. To overcome this, he would use nicotine lozenges in either a 2- or 4-mg strength. An extra-oral examination was carried out, which was unremarkable, and intra-orally the soft tissues and dentition appeared sound. The lesion had disappeared.
Further discussion revealed that prior to his dental check-up, the patient had been on a family holiday. In order to abstain from social smoking, 8–10 nicotine lozenges were used throughout the day. The patient reported holding these in his lingual sulcus, approximately where the lesion presented intra-orally. This was done throughout the entire duration of his holiday (14 days). Between the referral by his general dental practitioner and presentation within the OMFS unit, the termination of this habit had resulted in the self-resolution of the lesion (Figures 1 and 2). The patient reported the area remained asymptomatic and was noticed as a chance finding. To his knowledge, this was the first occurrence. On reviewing the referral sent by the patients general dental practitioner which included digital photographs, and comparing this with what presented within our unit, it was hypothesized that this was most likely localized hyperkeratosis in response to chronic chemical irritation.

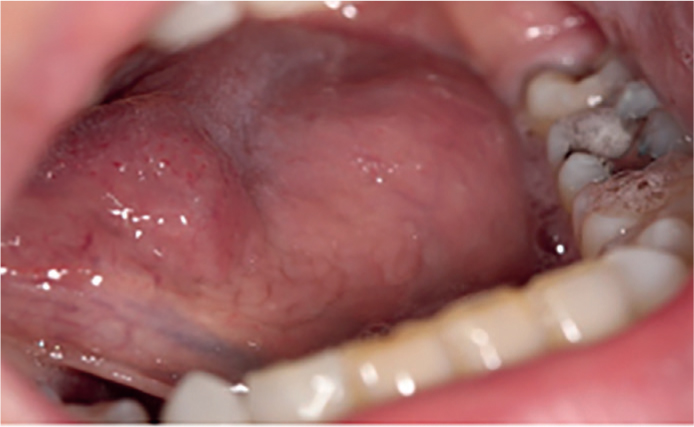
A new set of intra-oral photographs was taken that show the differences when compared to the initial presentation within primary care.
Owing to the complete resolution of the lesion, there was no indication for an incisional biopsy. Instead, the decision was made to discharge the patient back to his general dental practitioner for regular review. Additionally, advice was given, including limiting the use of nicotine lozenges, not holding them in one intra-oral location and seeking professional cessation services within the community. Furthermore, the patient was recommended to carry out regular self-examination of his oral tissues and advised to inform his general dental practitioner for immediate referral should any future lesions present.
In conclusion, intra-oral mucosal changes associated with NRTs is a rarely published side effect. The British National Formulary lists common side effects with oral and sublingual nicotine use that clinicians should be aware of (oral disorders, dry mouth, cough, altered taste)1 and chronic exposure of the mucosa to nicotine may result in the formation of hyperkeratotic white patches2,3 Primary care clinicians should consider whether an immediate referral is necessary. In some cases, a review may be appropriate and provide a better patient journey – saving both the clinician and patient any undue stress.
It is also recommended that regular reviews of this cohort of patients are undertaken by both general medical and dental practitioners to monitor for any potential suspicious lesions. This is vital following discharge from secondary care. If required, a non-urgent or urgent referral should be completed and the patient should be made aware of the potential outcomes.

