Article

This edition of the COVID-19 Commentary reviews and summarizes two landmark advisory documents on practising clinical dentistry during the coronavirus disease 2019 (COVID-19) pandemic, and beyond. Both these, freely available, documents are essential reading for the whole dental team currently engaged in the delivery of dental care either in UK or elsewhere.
The insidious persistence of COVID-19 in many communities, including the UK, is a stark reminder that dentistry must ‘adapt and adopt’ new infection control measures to return to practice. Hence, numerous organizations and professional bodies have issued multiple recommendations on how best to mitigate severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection risk in routine dentistry.1 It is, therefore, comforting to note the publication of two excellent pathfinder documents pointing the way forward for the dental team on safe clinical practice during the COVID-19 pandemic and beyond. The first is a guidance document from the Scottish Dental Clinical Effectiveness Programme (SDCEP) entitled Mitigation of Aerosol Generating Procedures in Dentistry: A Rapid Review,2 sponsored by NHS Education, Scotland. As the name implies, this document (46 pages) specifically addresses and appraises the extant evidence on a number of key questions related to aerosol generating procedures (AGPs) in dentistry, and recommends mitigation measures. The second is an extensive document (76 pages) issued by the College of General Dentistry (CGD) and the Faculty of General Dental Practice (FGDP), UK that covers a broader spectrum of practice issues, entitled Implications of COVID-19 for the Safe Management of General Dental Practice: A Practical Guide.3
Both documents, compiled by two different teams of experts, are timely arrivals when the profession is returning to work after the prolonged ‘shut downs’ and service curtailments. They complement each other well, despite the minor variations in terminology and recommendations. One major difference in the terminology is in the SDCEP document, which adopts the term AGP throughout, while the CGD team opts for a broader risk-based approach and uses the term ‘aerosol generated exposure’ (AGE), instead of ‘aerosol generating procedure’ (AGP). This, they contend, was selected ‘…to promote a risk-based approach and encourages dental professionals to consider AGEs from a quantitative perspective, and to consider the risk from droplet and aerosol spread from natural exposures, such as gagging, coughing or spluttering’. In other words, AGE is a broader, all-encompassing term that incorporates the risks from both naturally produced and procedurally generated aerosols.
In the absence of a significant evidence base on mitigating SARS-CoV-2 spread in clinical dentistry, both these documents provide sensible and pragmatic guidance on how best to practise dentistry in the current environment, until new data on therapeutic and preventive strategies, such as vaccines, and point-of-care diagnostics, emerge, As stated by the authors in the preambles, they are essentially dynamic and ‘live’ documents that will be updated as new data emerge. Although difficult to summarize in a short paper of this nature, the commentary below provides some of the salient features of interest to the readership. Both documents are essential reading for all practitioners embarking on post-COVID-19 clinical dentistry. The SDCEP paper is discussed first, followed by the CGD document.
Mitigation of Aerosol Generating Procedures in Dentistry: A Rapid Review by the Scottish Dental Clinical Effectiveness Programme (SDCEP)
As the name implies, the major focus of this document is on three major AGPs that, for the sake of convenience, have been categorized into three areas:
Group A: Procedures that will produce aerosol particles <5 μm due to the use of high velocity powered instruments.
Group B: Procedures that may produce aerosol particles <5 μm due to the use of low velocity powered instruments.
Group C: Procedures that may produce splatter, but are unlikely to produce aerosol particles <5 μm and do not use powered instruments. Examples of these are provided in Table 1.
| Group A | Group B | Group C |
|---|---|---|
|
|
|
|
The section on AGPs is then followed up by a discussion of the procedural and environmental mitigation. These are then subdivided as: categorization of AGPs; high volume suction; rubber dam isolation; pre-procedural mouthrinses, antimicrobial coolants; ventilation; and air-cleaners. Then, each subsection is further discussed in terms of: (i) evidence summary and appraisal; (ii) considered judgement and agreed position; and (iii) the position statement. Thus, in total, there are six well-argued and articulated position statements for the foregoing subcategories from the SDCEP document, which are summarized in Table 2.
| Position statement | Mitigation measure | SDCEP Recommendation |
|---|---|---|
| I | High-volume suction | Recommended |
| II | Use of rubber dam | Recommended |
| III | Pre-procedural mouthrinses | Not recommended |
| IV | Antimicrobial coolants | Not recommended |
| V | Fallow time | Recommended (for group A dental procedures: see Figure 1) |
| VI | Use of air cleaners | Not recommended |
Position statements and fallow-time determination
A well-argued case for all position statements can be found in the SDCEP document and they are not further discussed here, apart from the issue of fallow-time determination between two patient treatment sessions. In essence, SDCEP recommends that a minimum fallow time of 10 minutes must be applied after Group A procedures to include the time required for larger droplets to settle before environmental cleaning. It was surmised that, for Group B and C procedures (Table 1), the time for larger droplets to settle is accommodated within the standard infection control precautions as routinely used in dentistry. Additionally, they state dental procedures should not be conducted in a room that has no natural (ie a window) or mechanical ventilation.
Of the foregoing six position statements, perhaps the most contentious is the allocation of fallow time for Group A dental procedures with high-powered instrumentation. Consensus on this has been difficult to reach due to the lack of a robust body of convincing data on aerosol spread of SARS-CoV-2 in clinical dental settings when AGPs are used.4 However, the SDCEP Working Group has grasped the nettle and proposed a pragmatic, fallow-time algorithm for Group A dental procedures, drawing from data on fundamental principles of viral spread, and other accessory mitigation procedures (Figure 1).
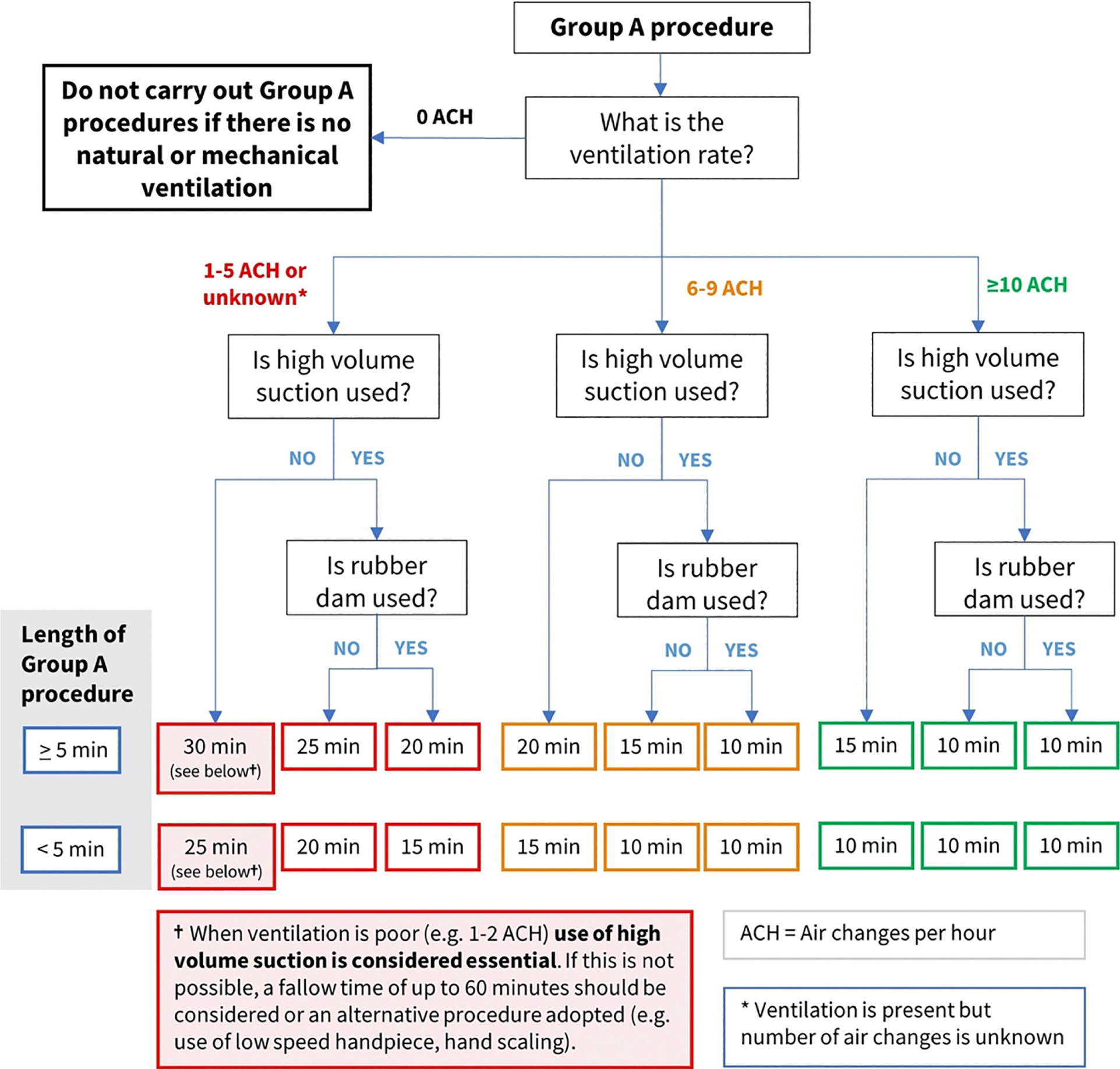
The algorithm provides various fallow times based on a bi-pronged classification of the duration of Group A procedures as either (a) shorter, or (b) longer than 5 minutes. These are then re-classified into fallow periods ranging from 10 to 30 minutes, depending on various mitigation procedures, and the number of ambient hourly air changes of the clinic. Clearly, due to the multiple confounding factors that dictate the fallow time, the algorithm is necessarily complex. For this purpose, a fallow-time calculator (FTC)5 has been launched to facilitate the process, which enables dental professionals to determine, justify and also record the fallow period necessary following dental procedures carrying a higher risk of exposure to potentially infectious aerosols. It is free to use once registered at https://myftc.co.uk/register
Implications of COVID-19 for the safe management of general dental practice – a practical guide by the College of General Dentistry Task Force3
This is the second, recently released document that points the way for safe dental practice during the COVID-19 era. It is a compilation by the task force of the CGD under the auspices of the FGDP, UK.
As mentioned, one of the key differences between the SDCEP and CGD document is the risk-based approach that the latter task force has adopted. Hence they opt to use the terminology ‘aerosol generated exposure’ (AGE), to substitute ‘aerosol generating procedure’ (AGP), owing to its broader remit that incorporates the risks from both naturally produced (eg coughing, sneezing), as well as procedurally generated aerosols.
Further, the CGD document is more comprehensive and is far broader, encompassing the following key areas related to the ‘patient journey’:
Each of the above sections comprise a summary narrative and a comprehensively tabulated matrix that could be used by practitioners as a quick reference to determine the risk level, and to identify measures that may be required in their practice in light of the alert level at that time.
Each matrix has three columns as follows:
The risk mitigation measures in the last column are subclassified as A, B and C, wherein ‘A’ measures are aspirational and represent the best possible practice. ‘B’ (basic) measures represent a minimum standard that must be in place for the procedures/topic and reflect a balance of the safety relative to the risk and alert level, and practical operating and resourcing constraints. ‘C’ measures are conditional, that is they denote basic measures (minimum requirements) in specific circumstances.
The document ends with two further sections on protecting vulnerable dental health care workers and frequently asked questions. The major points related to the five key areas discussed in detail in the document, are outlined below.
Pre-appointment
Patience attendance (pre-treatment)
During treatment
After treatment
Management tasks
Conclusion
In summary, the CGD Task Force document addresses a much broader range of subjects, while the SDCEP document focuses on a single aspect of practice protocol related to AGPs. The recommendations are a work in progress, and there is little doubt of their review and revision in the not too distant future due to the arrival of efficacious vaccines against SARS-CoV-2, point of care rapid diagnostic tests and, above all, new information on the infectivity and aerial and contact spread of this vicious virus. Finally, the summary commentary above does not do justice to either of these practical, timely and inclusive documents that should be considered essential reading for the whole dental team.

