References
A review of additive manufacturing in conservative dentistry and endodontics part 1: basic principles
From Volume 46, Issue 2, February 2019 | Pages 125-132
Article

Search strategy
An extensive electronic search was performed of articles on PubMed from 1990 to 2017. Key words such as ‘Additive printing’, ‘3D-bioprinting’, ‘CAD CAM’, ‘Rapid prototyping’ and ‘Restorative dentistry’ were used alone or in combination to search the database. The option of ‘related articles’ was also utilized. Finally, a search was performed of the references of review articles and the most relevant clinical research papers.
Introduction
In recent times, the use of CAD/CAM in dentistry has been synonymous with the rapid production of dimensionally accurate prostheses thereby omitting tedious laboratory procedures. Most of the current methods using CAD/CAM fabrication techniques in dentistry have concentrated on milling from a solid block of material (ie subtractive manufacturing). However, this method of manufacturing comes with some inherent limitations such as:
Considering the limitations, in the near future one can expect a major transition from making prostheses by subtractive manufacturing to what is referred to as additive manufacturing. Additive manufacturing processes were traditionally used to make prototypes or models and thus it had its origin in rapid prototyping (RP).
Rapid prototyping (RP)
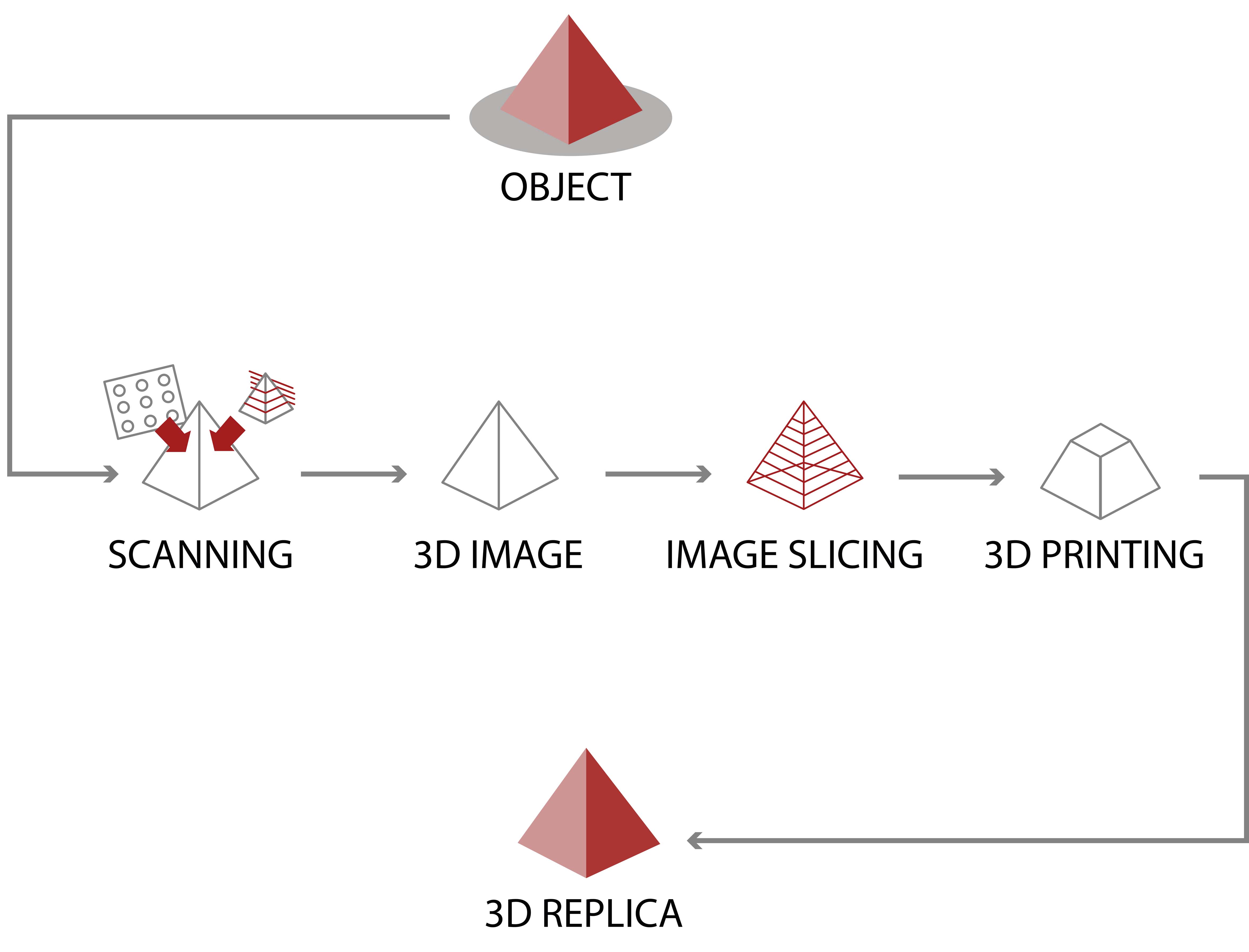
The first form of creating layer by layer three-dimensional objects using computer-aided design (CAD) was rapid prototyping, developed in the 1980s for creating models and prototype parts. Rapid prototyping is used to describe the customized production of solid models using 3-D computer data.2 This technology was created to help the realization of what engineers have in mind. Rapid prototyping is one of the earlier additive manufacturing (AM) processes. It allows for the creation of printed parts, not just models. Among the major advances that this process facilitates are time and cost reduction, human interaction and, consequently, a shorter product development cycle and also the possibility to create almost any shape that could be very difficult to make by machine.3 It operates on the principle of depositing material in layers or slices to build a model (additive technique). The primary advantage of this process is that the model created directly retains all the details of the internal geometry rather than just the outer surface contours.4
Data used by RP machines can be obtained by medical imaging techniques such as computed tomography (CT), magnetic resonance imaging (MRI), or laser imaging scans. These digitized technologies allow parts of the subject to be serially recorded, which can then be 3-dimensionally rendered and manipulated to generate accurate models.5 Several studies have analysed the dimensional accuracy of anatomic models produced by rapid prototyping systems (Figure 1).6, 7, 8
Literature on dimensional accuracy of RP
Barker et al compared measurements between anatomic landmarks on a dry skull with an anatomic replica and noted an absolute mean deviation of 0.85 mm.5 Choi et al found the absolute mean deviation between 16 linear measurements made on a dry skull and an RP model to be 0.62 mm.6 Bill et al determined that an accuracy of 0.5 mm can be reached for anatomic models based on CT data.7
The basic methodology for all current rapid prototyping techniques
Summary of various RP techniques
Stereolithography (STL)
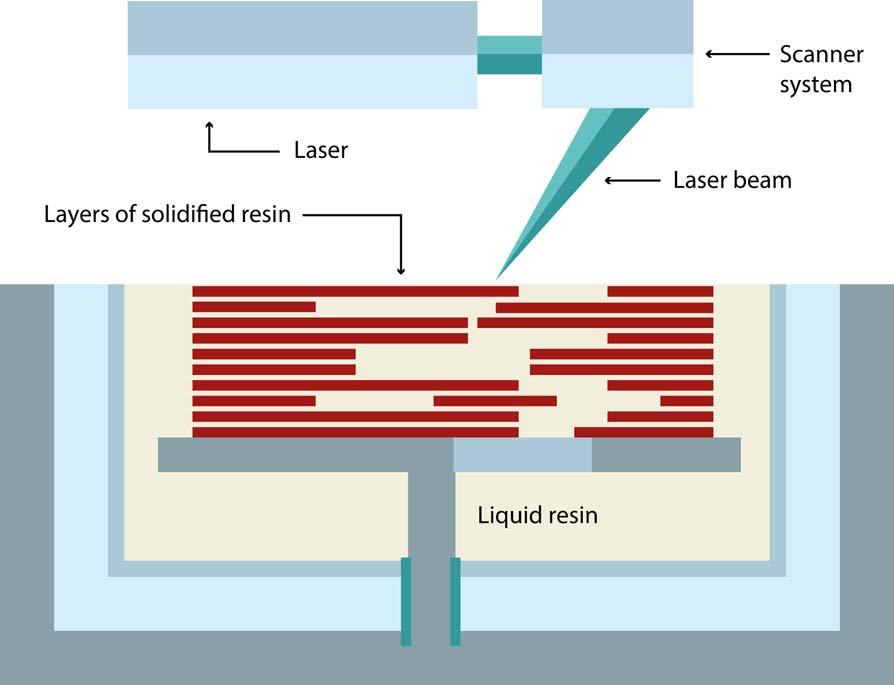
The STL file was created in 1987 by 3D Systems Inc when they first developed stereolithography, and the STL file stands for this term. It is also called Standard Tessellation Language. This is a liquid-based process that consists of curing or solidification of a photosensitive polymer when an ultraviolet laser makes contact with the resin. The process starts with a model in a CAD software and then it is translated to a STL file in which the pieces are ‘cut in slices’ containing the information for each layer. The thickness of each layer as well as the resolution depends on the equipment used. A platform is built to anchor the piece and support the overhanging structures. Then the UV laser is applied to the resin, solidifying specific locations of each layer. When the final layer is polymerized, the platform is lowered and the excess resin can be reused.9, 10, 11 A newer version of this process has been developed with a higher resolution and is called micro stereolithography, a process that means that a layer thickness of less than 10µm can be achieved.12 The basic principle of this process is photo polymerization, which is the process where a liquid monomer or a polymer converts into a solidified polymer by applying ultraviolet light, which acts as a catalyst for the reactions. This process is also called ultraviolet curing. It is possible to have powders suspended in the liquid-like ceramics (Figure 2).13
Disadvantages
Selective laser sintering (SLS)
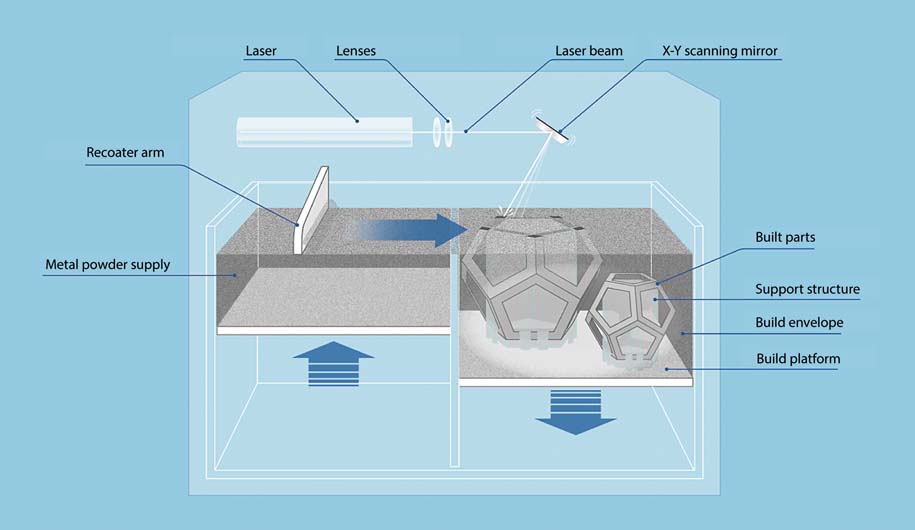
This is a three-dimensional printing process in which a powder is sintered or is fused by the application of a carbon dioxide laser beam. The chamber is heated to almost the melting point of the material. The laser fuses the powder at a specific location for each layer specified by the design. The particles lie loosely in a bed, which is controlled by a piston, which is lowered the same amount of the layer thickness each time a layer is finished. This process offers a great variety of materials: plastics, metals, combination of metals, combinations of metals and polymers, and combinations of metals and ceramics (Figure 3).12,17,18
Advantages
Disadvantages
Fused deposition modelling
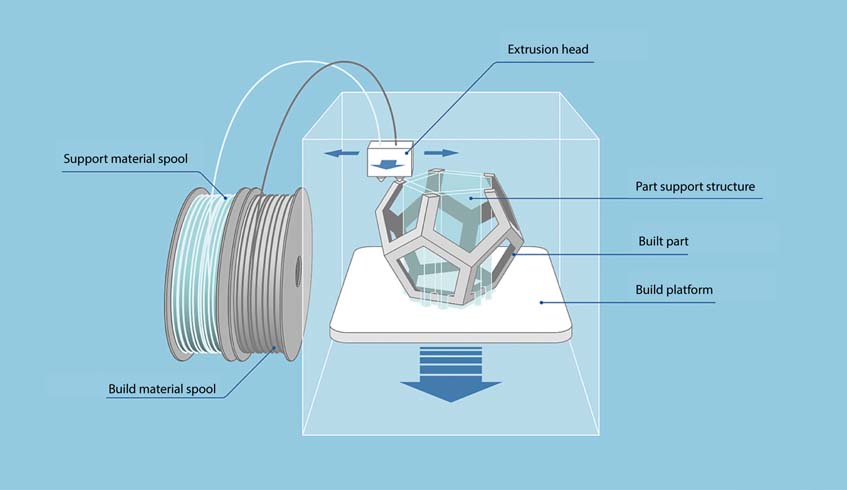
Fused deposition modelling (FDM) is an additive manufacturing process in which a thin filament of plastic feeds a machine where a print head melts it and extrudes it in a thickness typically of 0.25 mm. Materials used in this process are polycarbonate (PC), acrylonitrile butadiene styrene (ABS), etc (Figure 4).
Advantages
Disadvantages
3D printing (3DP)
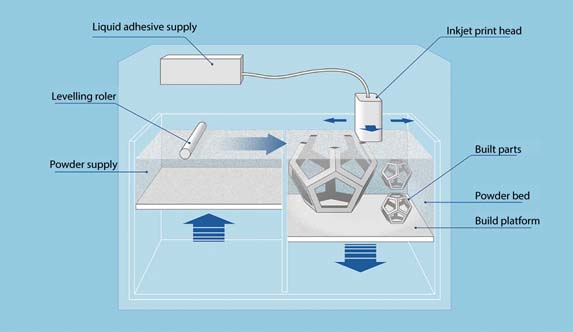
The 3DP process is a Massachusetts Institute of Technology licensed process in which a water-based liquid binder is supplied in a jet onto a starch-based powder to print the data from a CAD drawing. The powder particles lie in a powder bed and they are glued together when the binder is jetted. This process is called 3DP because of the similarity with the inkjet printing process that is used for two-dimensional printing on paper (Figure 5).
Advantages
In a study conducted by Ibrahim et al, the capacity of Selective Laser Sintering, 3D Printing and polyjet models to reproduce mandibular anatomy and their dimensional error was analysed.20 The authors concluded that the SLS prototype had a greater dimensional accuracy than the PolyJet and 3DP models (Figure 6).
3D bioprinting
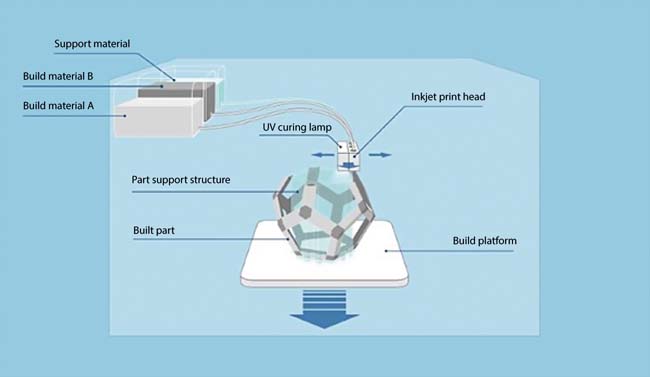
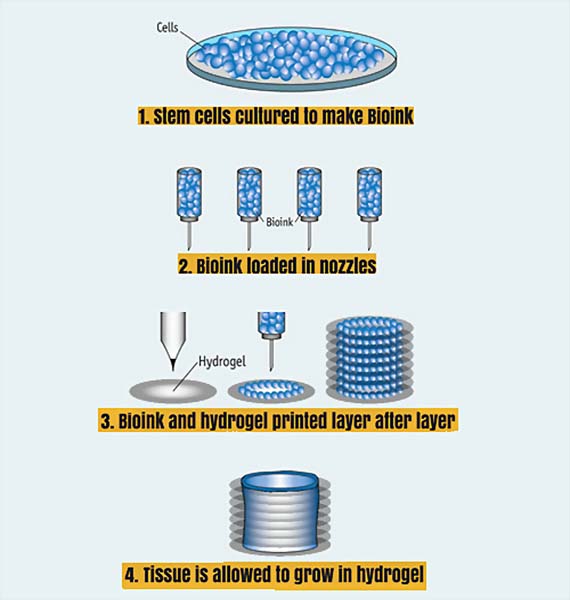
3D bioprinting systems can be laser-based, inkjet-based, or extrusion-based. The inkjet-based bioprinting is most common.21 This method deposits ‘bioink’ droplets of living cells or biomaterials onto a substrate according to digital instructions to reproduce human tissues or organs.21 Multiple print heads can be used to deposit different cell types (organ specific, blood vessel and muscle cells), a necessary feature for fabricating whole heterocellular tissues and organs.21
A process for bioprinting organs
Benefits of 3D printing
Customization and personalization
The greatest advantage that 3D printers provide in medical applications is the freedom to produce custom-made medical products, equipment and treatment planning such as:
Increased cost efficiency
3D printing offers the ability to design and manufacture items cheaply.25 Traditional manufacturing methods remain less expensive for large-scale production, however, the cost of 3D printing is becoming increasingly competitive for small production runs.25 This is especially true for small-sized standard implants or prosthetics, such as those used for spinal, dental or craniofacial disorders.22The cost to custom-print a 3D object is minimal, with the first item being as inexpensive as the last.25 This is especially advantageous for companies that have low production volumes or that produce parts or products that are highly complex or require frequent modifications.23 3D printing can also reduce manufacturing costs by decreasing the use of unnecessary resources.24 For example, a pharmaceutical tablet weighing 10 mg could potentially be custom-fabricated on demand as a 1-mg tablet.24
Enhanced productivity
‘Fast’ in 3D printing means that a product can be made within several hours.23 That makes 3D printing technology much faster than traditional methods of production, which require milling, forging and a long delivery time.22 In addition to speed, 3D printing is also holistically improving in resolution, accuracy, reliability and repeatability.22
Democratization and collaboration
Another beneficial feature offered by 3D printing is the democratization of the design and manufacturing of goods. An increasing array of materials are becoming available for use in 3D printing, at reduced price.23 This allows people from various sectors to employ 3D printing with imagination to design and produce novel products for personal or commercial use.23 The nature of 3D printing data files also offers an unprecedented opportunity for sharing among researchers.26 Researchers can standardize their methodology through access to downloadable ‘.stl’ files that are available in open-source databases.26 By doing so, they can use a 3D printer to create an exact replica of a medical model or device, allowing the precise sharing of designs.26 Hence, 3D printing is instrumental in international scientific collaboration and, towards this end, the National Institutes of Health established the 3D Print Exchange (3dprint.nih.gov) in 2014 to promote open-source sharing of 3D print files.
Bioprinting tissues and organs
Tissue or organ failure due to ageing, diseases, accidents and birth defects is a critical medical problem.27
Challenges in traditional organ transplant protocols
Although still in its infancy, 3D bioprinting offers additional important advantages beyond this traditional regenerative method (which essentially provides scaffold support alone) such as, highly precise cell placement and high digital control of speed, resolution, cell concentration, drop volume and diameter of printed cells.21, 28

