References
Immediate dentures part 1: assessment and treatment planning
From Volume 45, Issue 7, July 2018 | Pages 617-624
Article
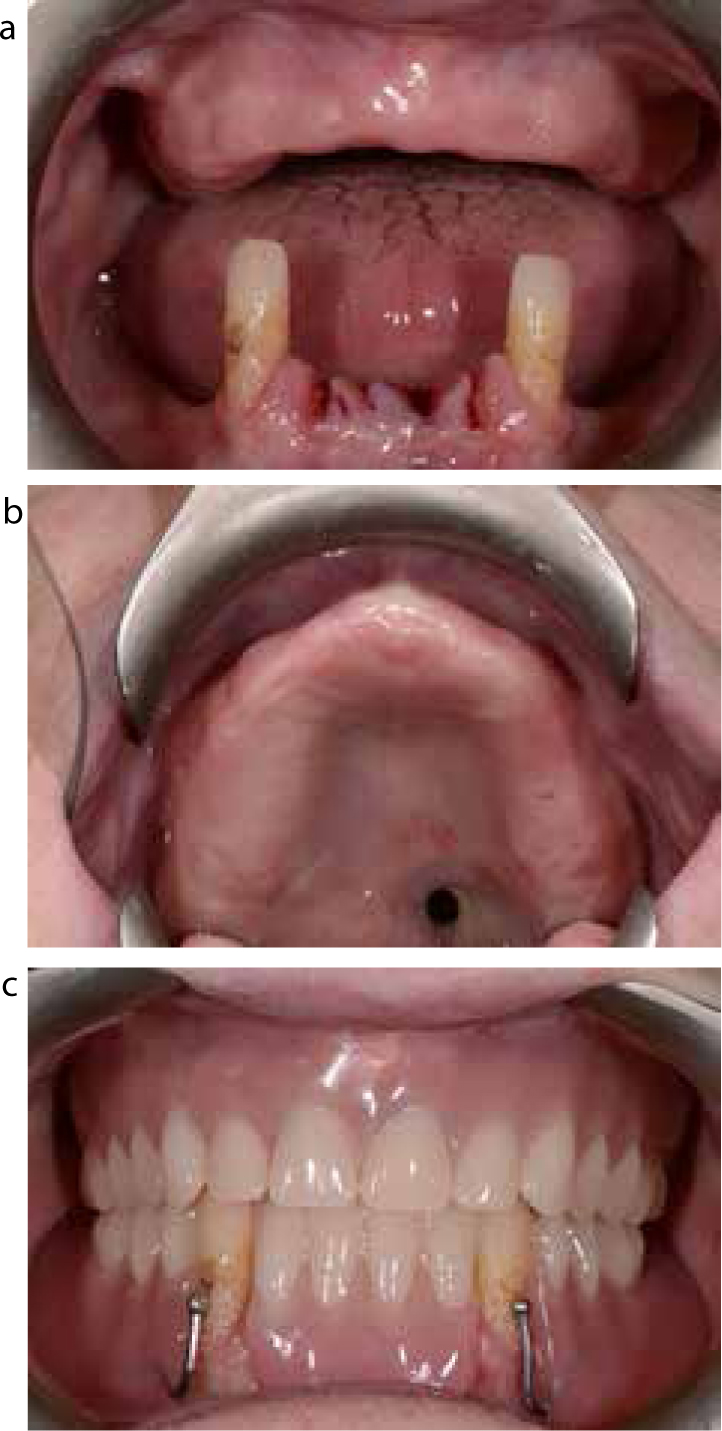
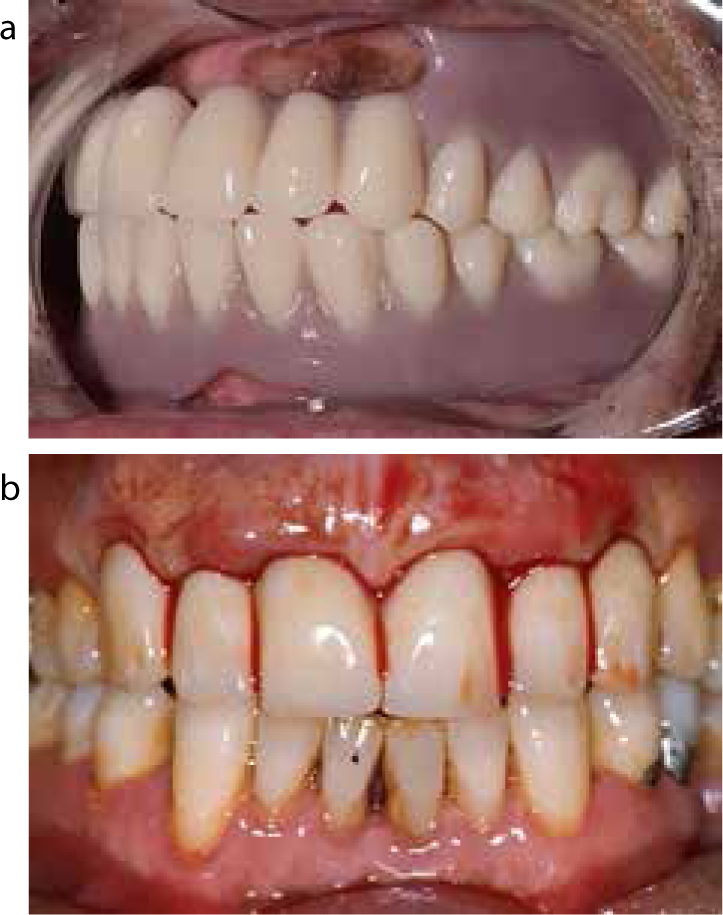
An immediate denture is a complete or partial removable prosthesis that is fitted immediately after extraction or modification of teeth. The prosthesis replaces the missing/modified teeth and, where required, the adjacent hard and soft tissues. It is constructed prior to the extraction of teeth and is used immediately to provide function and aesthetics which are lost as a result of tooth removal and avoid the embarrassment patients may have with living without teeth, while waiting for the tissues to heal prior to definitive tooth replacement1 (Figure 1). Some clinicians take impressions on the day of the extractions and fit the dentures a few days later. These dentures are fraught with challenges as the alveolar ridge begins to resorb soon after extractions, therefore an immediate denture is only truly an immediate denture when fitted on the day of the extractions.

The use of a removable prosthesis within the UK is currently around 19% of adults in the general population2 and, in spite of a decreasing trend, as patients retain their natural dentition into older age,2 there is still a need for prosthodontic replacement as teeth are lost as a result of caries, periodontal disease, tooth wear or trauma.3,4,5 The provision of an immediate denture can be challenging. Close co-operation between patient, technician and clinician is therefore required.
Assessment and treatment planning
All patients should have a thorough history, clinical examination and any relevant investigations carried out in order to attain a correct diagnosis and treatment plan. The formulated diagnoses and treatment plan, as well as the costs and timeframes involved, need to be thoroughly discussed with the patient in order to obtain informed consent before proceeding with treatment. It is also vital that the clinician has a clear understanding of the patient's expectations of treatment and whether these can be achieved in the proposed treatment, particularly in those patients who have never worn dentures before. Patients need to be clearly made aware of the limitations of a removable prosthesis in general and also the issues associated with an immediate denture. Denture wearing is a complex phenomenon and, while the technical ability of the clinician has a huge role to play in its success, it is largely dependent on the patient's psychological acceptance and neuromuscular ability to cope with the dentures.6
History
A thorough history of the patient is required. This will entail asking questions regarding any presenting complaint or issue which the patient is having, the patient's medical history and briefly exploring the patient's dental and social history. Taking a full and thorough history succinctly is a key skill since correct diagnosis relies on it. This in turn enables the clinician to propose an appropriate treatment plan.
A detailed medical history should include information regarding all relevant conditions. This would include, but not necessarily be limited to, information regarding bleeding disorders such as haemophilia, immuno-compromised patients, those with a history of head and neck radiotherapy, as well as those on anti-coagulants or bisphosphonates. In some situations, a patient's medical background can complicate or impact the process of dental extractions that the clinician needs to be aware of and be able to manage appropriately. There are also medical conditions that may make provision of a removable prosthesis challenging. This includes certain neuromuscular conditions (Table 1). The exact management of these conditions goes beyond the scope of this article.7,8,9
|
1-
|
Parkinson's disease |
Information regarding the patient's dental history, such as frequency of attendance, previous dental treatments and attitude towards dental treatment, gives an indication of how well a patient is likely to tolerate treatment. A brief understanding of the patient's social history with regards to his/her occupation, any hobbies or activities and the availability for appointments will help with planning treatment. Patients in certain professions may struggle with removable prosthesis, such as wind instrument players and public speakers, and the effect of the proposed treatment needs to be discussed.
Examination
A comprehensive examination in a methodical sequence is required, this includes an assessment of the following:
Denture-bearing tissues/edentate spaces
Examination of the denture-bearing areas should be carried out in detail since this will have an impact on the design of the final prosthesis. In cases of an immediate denture, it may be difficult to ascertain the ridge shape in the areas where extractions will be carried out. However, if there are any other edentulous spaces in the mouth, assessing them in detail will give an idea of the kind of retention, stability and support that can be gained from the denture base (Figure 2). The edentate ridges should be assessed on their height, width and shape, the firmness of overlying tissue and any undercuts that may be present. Muscle and frenal attachments should be checked, along with the sulcus depth, plus noting the shape of the palatal vault for the maxillary prosthesis (Table 2). In addition to the visual examination, palpating the denture-bearing areas carefully is a useful method to determine if there are areas of discomfort in the patient's mouth as these may require relief in the final prosthesis.10
|
1-
|
Alveolar ridge height, width and shape |
Dentition
The dentition and its supporting structures should be evaluated, which includes assessment of the periodontal condition along with BPE (Basic Periodontal Examination) scores, presence of caries, tooth surface loss, as well as any restorations and their condition. Teeth of hopeless prognosis should be planned for extraction and those with poor or dubious prognosis should be noted down and form part of the treatment plan, taking future tooth loss or need for extractions into account.7
Ideally, the primary disease within the mouth, such as periodontal disease, caries and tooth wear, should be stable and aetiological factors controlled prior to embarking on tooth replacement, although this may not always be possible. Any sub-optimal or defective restorations should be repaired or replaced, where appropriate, as part of a comprehensive treatment plan. Where possible, these restorations may be utilized to help retain or support the prosthesis.
Current prosthesis
Any prosthesis that the patient is currently wearing should be assessed and consideration given as to whether the current prosthesis can be added to or not. It is sensible to assess the existing prosthesis in detail, inside and outside of the patient's mouth. In situ, the prosthesis should be evaluated for retention, stability and support, with assessment of the occlusion and peripheral extensions, paying close attention to areas that are over or under extended around denture-bearing tissues. The occlusion should be checked and the occlusal vertical dimension (OVD) and freeway space noted. Aesthetics should be evaluated visually but it is also helpful to hear the patient's opinions on his/her existing denture. If the patient is happy with the aesthetics then this can be used to guide the final prosthesis. Any teeth that may be aiding the retention of the current prosthesis should be noted and their condition assessed as some of these may require extractions due to a poor prognosis. Similarly, other aspects of the current prosthesis can be assessed based on the discussion with the patient regarding the positive or negative experiences from denture wear, such as a loose mandibular prosthesis. This may be due to excessive resorption of the alveolar ridge and making the patient aware of its impact in the final prosthesis is helpful. Alternatively, a patient wearing a poorly retentive maxillary prosthesis, due to lack of palatal coverage, may prefer the design to be copied again and therefore needs to be aware of the limitations of the final result and the reasons associated with it. Allowing the patient to guide the clinician towards the final design of the prosthesis often provides for a satisfactory result for the patient.
Occlusion
A detailed occlusal assessment for the patient is indicated. Things to evaluate include assessing the patient's inter-cuspal position (ICP) and whether this is stable or not. In some cases, identifying the patient's retruded contact position (RCP) can be useful, as well as an assessment of the occlusal vertical dimension (OVD) and freeway space (FWS), and this should be assessed with and without the prosthesis in situ. A decision needs to be made on whether to maintain the existing jaw relationship or to re-organize the occlusal relationship when providing the prosthesis. In instances where the patient has a stable ICP and an appropriate OVD, it is sensible to maintain existing jaw relations. This will often be the case where a patient has retained most of his/her natural teeth. In situations where teeth have been lost to disease, this can lead to loss of OVD, causing mandibular over closure. Consideration needs to be given as to whether this is accepted or an increase in OVD would be a more sensible option. In complex situations, or to assist the treatment planning process, it may be useful to attain articulated study models, particularly when a reorganized approach is planned.
Investigations
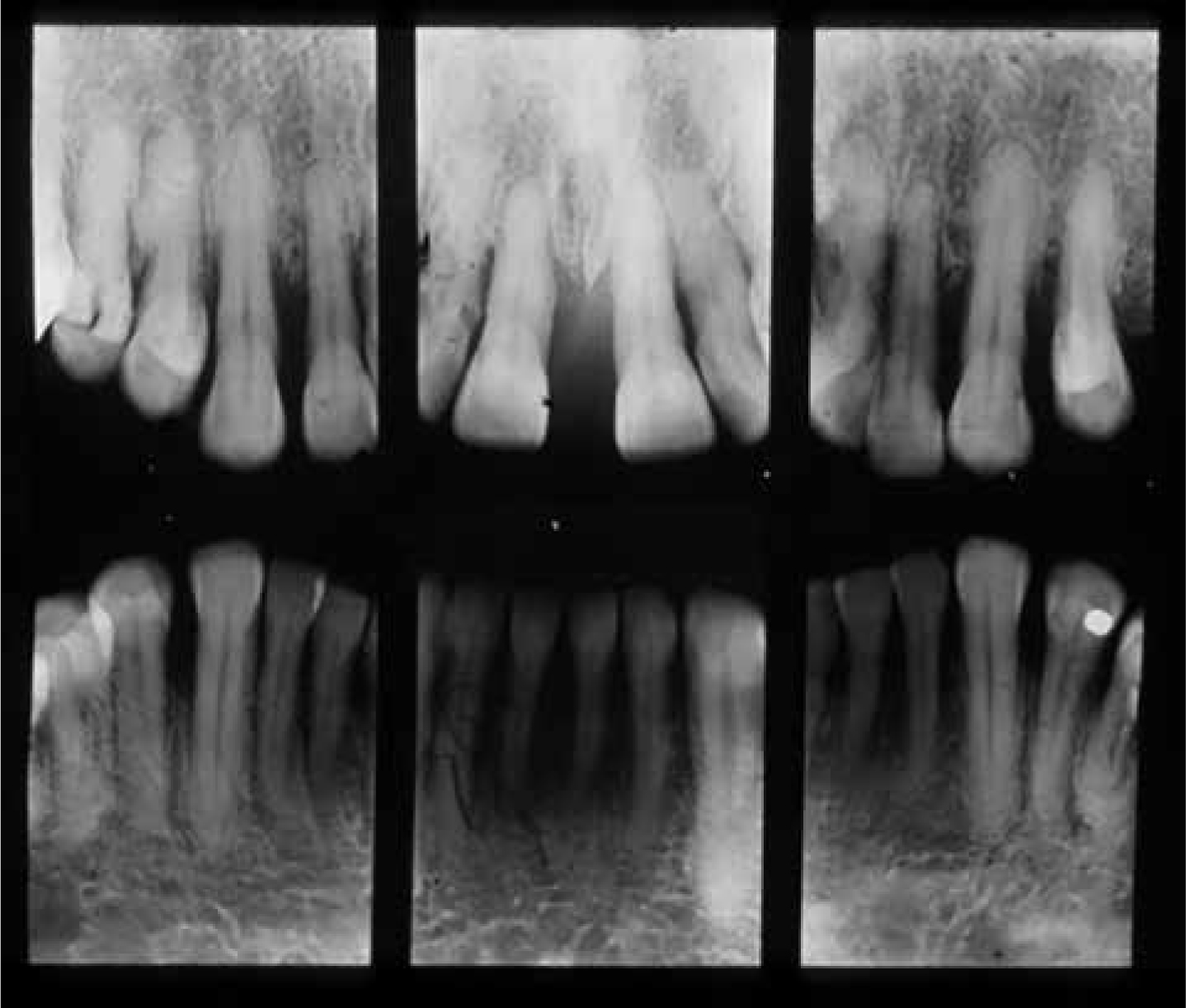
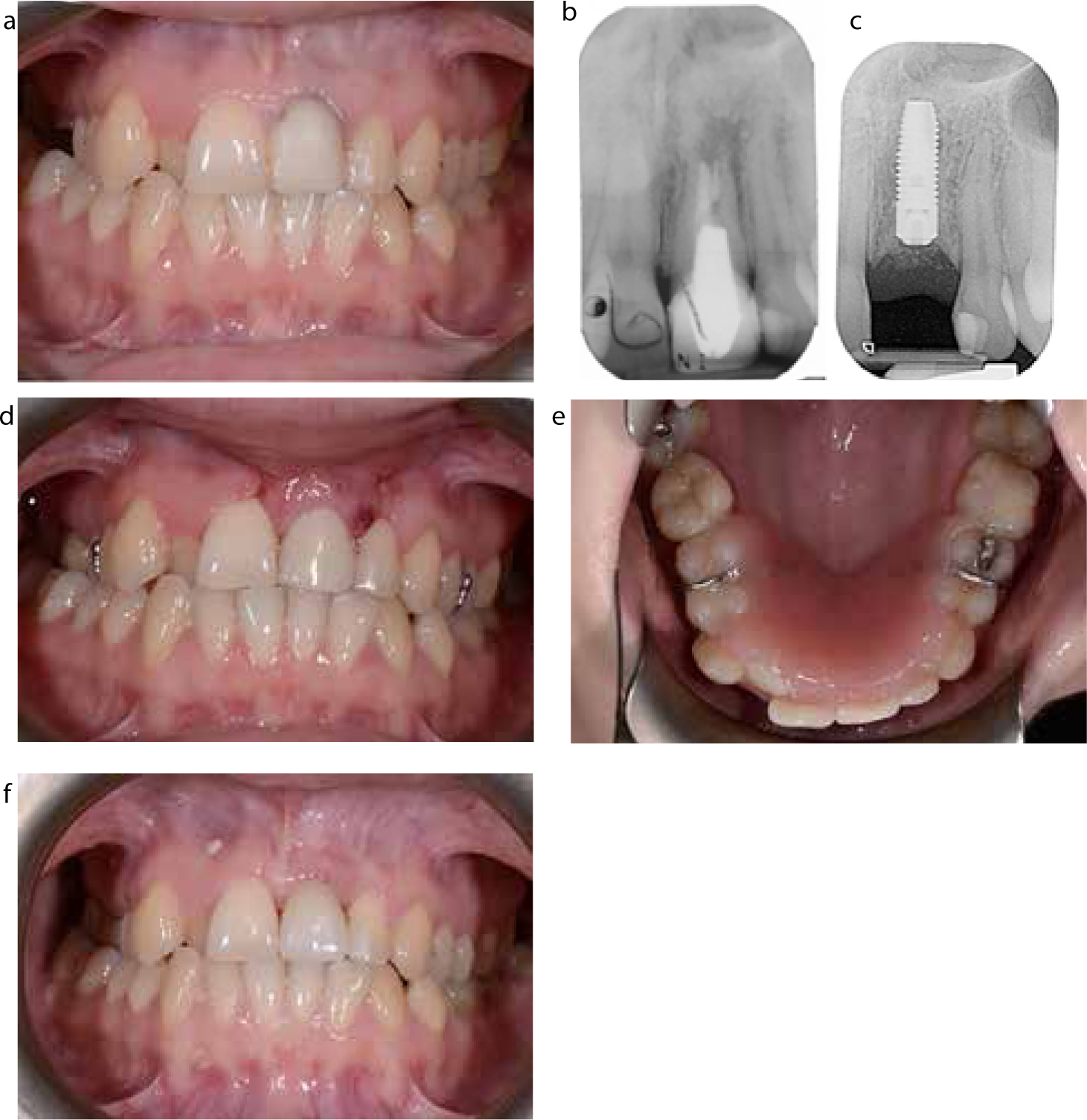
Appropriate investigations should be undertaken to help diagnose and plan treatment. Any teeth considered for extractions should have pre-operative radiographs to assist in the planning of the extractions (Figure 3). It is important to have articulated study casts to analyse and assist in the planning of the prosthesis prior to embarking on treatment and they can also be waxed-up to allow the proposed end result to be visualized.
Diagnosis and treatment planning
Once a thorough assessment has been undertaken, a diagnosis can be reached. This can enable the clinician to develop a clear picture of the patient's needs and develop an appropriate treatment plan, keeping in mind the patient's wishes, suitability for treatments, number of visits and the costs involved. The treatment plan should outline the nature of the procedures involved and, where possible, a proposed denture design.
The teeth that have been proposed for extraction need to be planned. Where a large number of teeth have been planned for extraction then a staged process of exodontia may be considered. Historically, this entailed extracting the posterior followed by the anterior teeth. This allowed the soft tissues of the extracted posterior teeth to heal prior to extracting the remaining anterior teeth and fitting the immediate complete denture at the same time.11,12
Staged extractions may be considered due to the patient's medical history, or if there is concern about the patient's tolerance to a removable prosthesis. In such situations, a transitional/acclimatization approach is utilized whereby certain teeth are extracted and these are added to the prosthesis over a period of time. Planning of immediate removable dentures may be dictated by events such as painful teeth, associated pathology, teeth with poor prognosis or those with limited prosthodontic use. These teeth are often the ones extracted first. Where possible, it is useful to retain teeth in opposing arches that provide some form of tooth to tooth contact at an appropriate jaw relationship for as long as possible, in order to assist in the denture construction and aid in the acclimatization for the patient.7
Denture type
In general, there are two types of immediate dentures that are described in the literature. These are:
Immediate dentures, like conventional prostheses, are most commonly fabricated from acrylic. In general, acrylic dentures are cheaper and quicker to construct and more amenable to modification.
Denture design
An important aspect of the design process is consideration for the type of flange to be used, particularly in the anterior region, with the options of either a full, partial or an open faced/socketed (flangeless design).
A full flange will extend to the full width and depth of the sulcus: the advantage of this is that it will maximize surface area for support and retention and, for this reason, where possible should be utilized as the first choice for immediate dentures. In patients with a degree of bony undercut or a low smile line, a partial or an open faced/socketed or a partial design is preferable. A partial flange design extends the labial flange border about 1 mm beyond maximum bulbosity of the ridge.8,14,15 These are useful in cases where an undercut of the alveolar ridge is present, but aesthetics dictate a flange, hence a short or partial flange is a reasonable compromise (Figure 5).

Alternatively, the open faced/socketed design helps to maintain an acceptable appearance in the immediate post extraction period in the anterior region by placing the necks of the denture teeth into the sockets so that these appear like natural teeth emerging through the gingivae,8 thus avoiding any displacement of the overlying soft tissue which may happen with a flanged design (Figures 6 and 7). This will help to maintain aesthetics. These types of prostheses are easier to fit. However, retention will be reduced, particularly where a complete immediate denture is fitted, as a peripheral seal cannot be made. Other drawbacks with this design include gaps appearing over time between the border of the prosthesis and the ridge during bony remodelling post-extraction. Such gaps can be unsightly as well as making the denture more challenging to reline.7,16 Adding a flange to this design is difficult and usually a remake is indicated early on.

Conclusion
Immediate dentures play a significant role in providing patients with tooth replacement immediately after loss of teeth, ensuring restoration of aesthetics and function. A list of advantages and disadvantages of immediate dentures is given in Table 3. Since the success of immediate dentures is greatly influenced by patient factors, it is therefore helpful to have a clear discussion regarding patient expectations as well as to gain informed consent. This should be followed by a thorough history and examination of the oral tissues, as well as any existing prostheses. In the next part, the various stages of denture construction, post-operative patient management, and any future additions to the immediate dentures, will be discussed.
| Advantages | Disadvantages |
|---|---|
| To the patient | To the patient |
|
|
|
| To the clinician | To the clinician |
|
|
|

