References
Endodontics or implants?
From Volume 45, Issue 6, June 2018 | Pages 506-521
Article

Endodontic treatment and implant placement are two different treatment modalities that can be utilized to restore function for a patient. When presented with a tooth that has pulpal or periapical infection and a potentially poor prognosis, a number of factors need to be taken into account; these include patient preferences, tooth and periapical factors and evidence-based outcome for both treatment options.
Endodontic treatment aims to treat and maintain the tooth through either non-surgical or surgical approaches, whereby placement of a dental implant improves function by replacing a missing or a tooth of hopeless prognosis. Outcome studies on both treatment modalities appear to yield similar results, however, it must be emphasized that success criteria for outcome in endodontic treatment is strict when compared to that of implants.
There are a number of factors that can influence the outcome of each of the treatment options and knowledge of these is paramount when making an informed decision. Table 1 summarizes some of the main factors to take into consideration for treatment planning when presented with a tooth with infection and a potentially poor prognosis.
| Tooth-related | Remaining amount and quality of coronal tissue | |
| Presence and size of a periapical lesion | ||
| Presence of pre-operative sinus tract | ||
| Patent root canals | ||
| Iatrogenic damage: perforation/ledging of the root canal | ||
| Quality of the existing obturation in retreatment cases | ||
| Root fractures | ||
| Root length if considering apical surgery | ||
| Periodontal | Periodontal disease | |
| Perio-endo lesion depending on the primary origin | ||
| Amount and quality of bone | ||
| Amount of keratinized tissue | ||
| Gingival biotype | ||
| Patient-related | Smile line | |
| Aesthetic demand | ||
| Oral hygiene | ||
| Bruxism | ||
| Smoking | ||
| Systemic | Medication-related: systemic bisphosphonate treatment for osteoporosis, cancer or Paget's disease |
|
| Medical history: | Radiation to the head and neck area |
|
| Pregnancy | ||
| Age-growth of jawbones completed | ||
It has been highlighted that dentists may have a preference for the treatment modality to use, depending on their training experience. When making decisions on patients' treatment, clinicians should consider their perceptions and preferences.
Patient-centred outcomes
When considering patients' perceptions, clinicians look at oral health impact profile scores (OHIP). The lower the score, the better the perceived outcome for the patient. When comparing the quality of life for patients restored with a single endodontically-treated tooth versus a single implant-supported prosthesis, Gatten et al found a high rate of satisfaction with both treatment modalities. However, there was a clear message from the patients that they wanted to save their natural teeth, if possible.1 When considering options for overdentures, there was found to be no quality of life difference when using retained roots as overdenture abutments when compared to implant-supported overdentures.2
Dentist-led decision-making
When treatment planning a case, the best available evidence must be taken into account with the clinician's own experience. This may account for the variations in treatment planning depending on training experience. Lang-Hua found, when assessing the treatment planning decisions of dental practitioners with and without postgraduate implant qualifications in Hong-Kong, that those with postgraduate qualifications were three times more likely to retain teeth as those without.3 In Canada, a survey of dental practitioners showed a higher rate of preference for implant-supported crowns in general as opposed to endodontic retreatment.4 In America, there was not a shift towards a preference for implant treatment when compared to endodontic treatment. However, a perceived superior outcome for implant treatment was said to exist in the dental community.5
Success versus survival of root canal treatment and dental implants
When referring to the evidence on outcome studies to identify the best treatment for a compromised tooth, direct comparison between implants and root canal treatment can be a challenge, as highlighted by Iqbal and Kim.6 Success criteria for root canal treatment, whether surgical or not, is strict and described as an absence of clinical symptoms and healing of the periapical tissues.7 Success criteria for implants has been proposed and includes absence of mobility, peri-implant radiolucencies, signs or symptoms of pathology and less than 0.2 mm of bone loss annually after the first year of placement.8 However, as highlighted by Iqbal and Kim in their systematic review, most implant studies measure survival as an outcome measure, compared to success in endodontic studies. When a direct comparison in their systematic review was undertaken, it showed that there were no significant differences between non-surgical root canal treatment and single tooth replacement implants when using survival as the outcome measure. Doyle et al carried out a cross-sectional retrospective study matching 196 implant-supported restorations with initial non-surgical root canal treated teeth measuring four different outcomes: success, survival, survival with subsequent intervention and failure. They found that the number of failures were the same in both groups, however, implant treatments had a higher fraction of cases that were classified as surviving with the requirement of subsequent treatment. Interestingly, the implant cohort were five times more likely to require an intervention over the observation period compared to endodontically-treated teeth.9
Factors affecting the outcome of non-surgical root canal treatment
Success rates for primary and secondary root canal treatment, based on periapical health, have been reported to be 83% and 80%, respectively.10 There are a number of prognostic factors that can significantly affect the success rate of the root canal-treated tooth which can be identified pre-operatively. Ng et al reported a number of factors that should be taken into account when assessing the chance of success using root canal treatment; these include the pre-operative absence of a periapical radiolucency, the smaller the radiolucency the better the prognosis; the odds of success were found to reduce 14% for every 1 mm increase in diameter of a preoperative lesion.10 In addition, the absence of a sinus and root perforation significantly affected the rates of success by 48% and 56%, respectively. Intra-operatively, the ability to treat to the apical terminus, absence of inter-appointment flare up and obturation to within 2 mm of the apex were positive prognostic factors. The presence of a satisfactory coronal restoration is a pivotal factor in survival of the root canal-treated tooth, in addition to having mesial and distal proximal contacts, which suggests that the amount and integrity of the remaining coronal tissue, in addition to occlusal forces, have an effect.11 Ray and Trope investigated the radiographic quality of coronal restoration and root canal treatment and found that periapical health depended more on the quality of restoration.12 Tickle et al reported on their study on NHS-treated molar teeth that those that had been crowned had better success rates than teeth with intracoronal restorations and this was more important than the radiographic quality of the root canal filling.13 Whether a cuspal coverage restoration should be placed has also been investigated; in an eight-year retrospective study looking into root canal-treated posterior teeth, there was 84% survival when a full coverage crown was placed; this lowered to 71% if no crown was placed. They found that root canal-treated teeth receiving a crown over 4 months after root canal treatment was completed were three times more likely to be extracted than teeth being crowned within 4 months.14 In a 3-year study on premolar teeth with Class II cavities restored with fibre posts and direct composite restorations, Mannocci et al reported that the success rates were similar when compared with porcelain fused to metal crowns.15 Therefore, in premolar teeth with small access cavities which are not involved in guidance, it may be possible to avoid placing a cuspal coverage restoration.
A good coronal restoration has been shown to lead to an 11-fold increase in the odds of success.10 In a large scale study of outcomes of initial endodontic treatment over 8 years, 1,126,288 patients were assessed and showed that only 3% of teeth required extraction; of these teeth, 85% did not have full cuspal coverage.16 The quality of the coronal restoration has been shown to be a predominant factor in the absence of peri-radicular infection.17In vitro studies have shown that it takes a few days for bacteria to reach the apex of a root-treated tooth and that endotoxins may penetrate the system sooner.18, 19
There is a lack of evidence relating smoking habits and the prognosis of root canal treatment, however, a review on the subject states that there is a possible influence on the prognosis of endodontically-treated teeth and a likely increase in surgical complications.20
Surgical root canal treatment
When faced with a failed root canal treatment, non-surgical re-treatment would be the favoured option to enable thorough cleaning of the root canal system. In certain circumstances, surgical endodontics is indicated:21
Surgical endodontics would not be advised if there is a poor coronal seal, poor initial root canal treatment, an unfavourable crown to root ratio or reduced periodontal support.22, 23 A recent Cochrane review stated that, at this current time, there is insufficient evidence to determine whether surgical or non-surgical methods have better success to treat periapical lesions.24 The use of micro-surgical techniques, however, in surgical endodontics has improved success rates, yielding results as high as 94% success compared to 59% for traditional surgical methods in a recent meta-analysis.25
Tooth restorability
To assess the restorability and prognosis of a tooth that is to undergo root canal treatment, ideally coronal disassembly of existing restorations will be carried out. Abbott showed that, when assessing 245 teeth before and after coronal restoration removal using periapical radiographs and clinical examination, there was only a 56% chance of detecting caries, cracks or marginal breakdown (Figure 1). He also identified that composite restorations were more often associated with early onset and rapid progression of pulpal disease, indicating rapid rates of marginal breakdown and loss of seal in these restorations.26
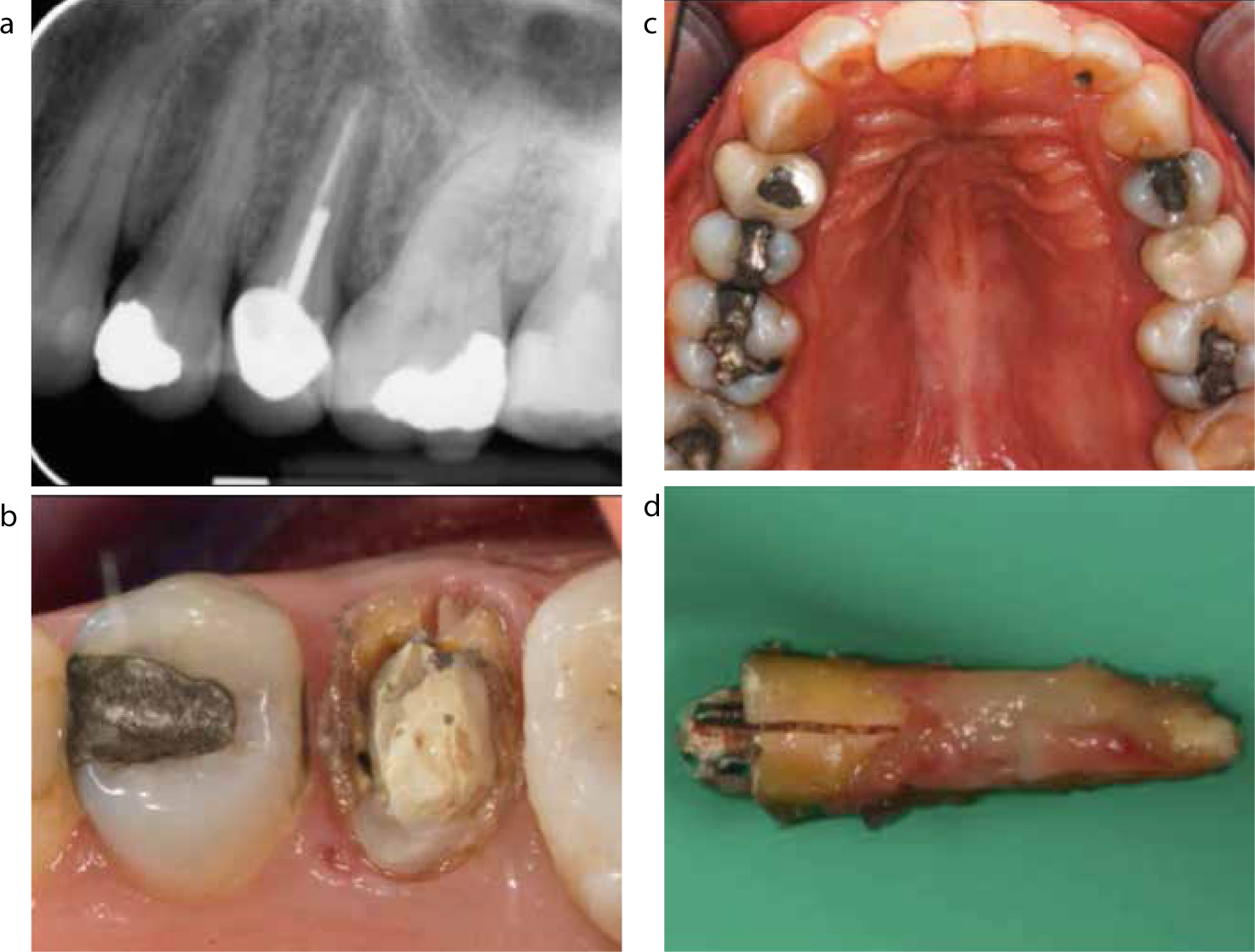
The presence of a post-retained restoration should not deter the practitioner in disassembly as part of the assessment process, as it has been shown by Abbott that the fracture of roots when removing a post was not high risk. Out of 1600 post removals, root fracture was detected in 0.06% of the cases27 (Figure 2). In addition, when assessing restorability of a posterior tooth, a bitewing radiograph may be beneficial in addition to a long cone periapical as it gives a perpendicular and therefore more accurate representation of the cervical alveolar interface28 (Figure 3).
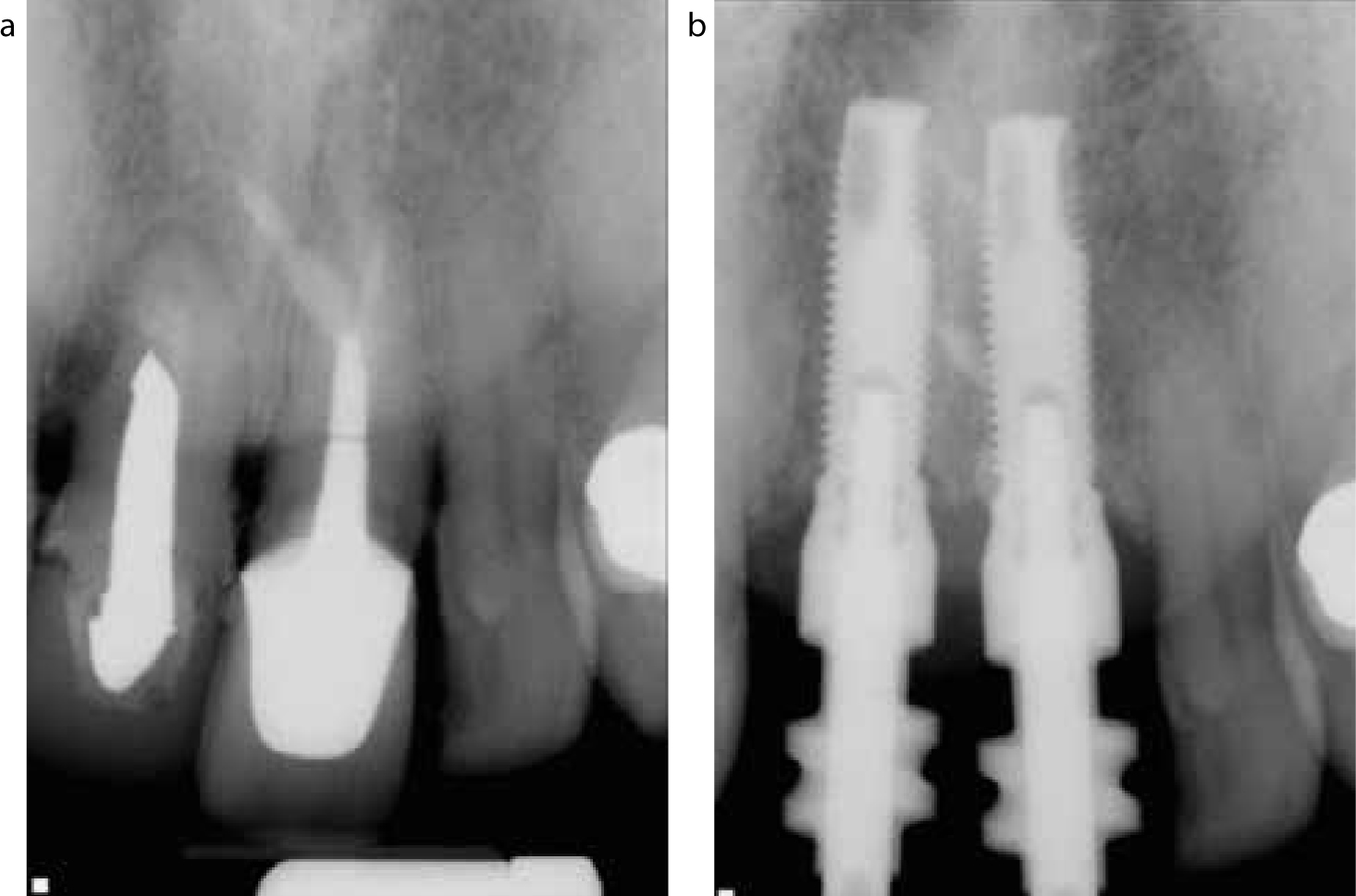

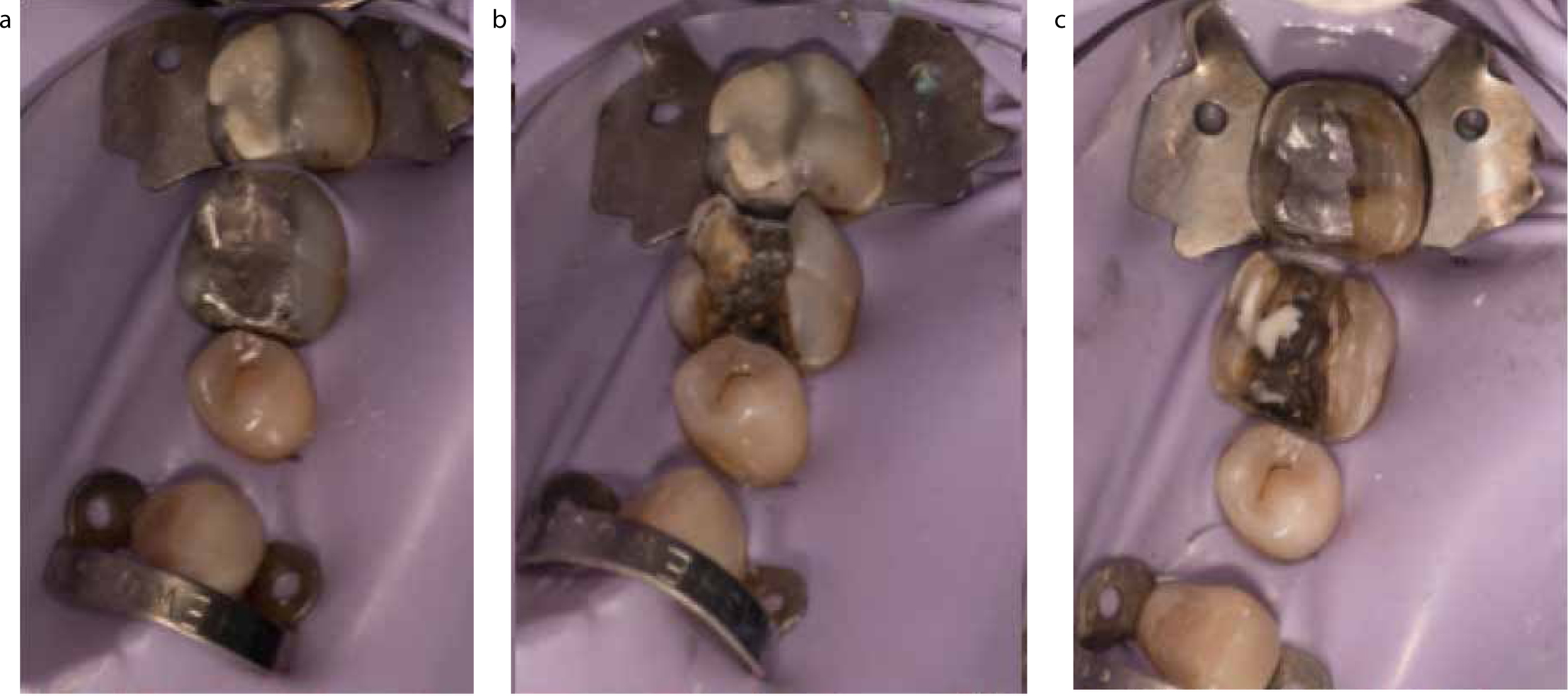
To assess restorability of a tooth, we need to know how much sound tooth tissue is present above the alveolar crest and the functional requirements of the tooth to be restored. Goodacre suggests a minimum of 4 mm of coronal height in posterior teeth and 3 mm anterior for extra-coronal restoration with conventional retention and resistance form.29 If adhesive technology is to be used, the amount of remaining supported enamel to bond to is an important consideration. Attempts have been made to objectivize the restorability of a tooth to help decision-making using the Tooth Restorability Index30 and indicate whether crown lengthening or a post may be required to optimize retention and resistance form of the future crown. This seminal paper by Mcdonald and Setchell is highly quoted but is purely based on conventional retention and resistance form in retaining an indirect restoration. In adhesive techniques, the enamel quality is a consideration, for example cervical enamel is thin (0.3 mm) and typically difficult to bond to, in addition to the location of enamel in relation to the gingival margin, and therefore the ability to isolate this with a rubber dam. A way to determine if a restoration can be adhesively bonded is to carry out the tooth preparation under rubber dam; if the most apical margin can be isolated and enamel is present there, then the definitive restoration can be bonded with resin cement (Figure 4). A new tooth restorability index called the ‘Dental Practicality index’ has recently been proposed by Dawood and Patel. This makes some developments on the ‘Tooth Restorability Index’ as it takes into account the patient's periodontal status, medical co-morbidities, and complexity of endodontic treatment required. It does not look at the tooth preparation in terms of whether you can predictably bond or not.31
Teeth restored using intra-radicular retention have shown high survival rates over 5 years, provided that high quality root canal treatment and restorative protocols were implemented.32 It has been found that the presence of a ferrule of tooth structure was the most important factor on outcome when using posts, more so than the type and length of post used.33
Dental implants
Dr P-I Brånemark is regarded as the father of modern implantology. His discovery came about in the late 1950s when he was unable to remove titanium optical chambers from rabbit femurs where he had been studying blood flow.34 Its applications were introduced into dentistry in the 1960s.35 Later, Brånemark described the phenomena that existed between the ‘fixture’ and the bone in which there was a direction structural and functional relationship as osseointegration.36 The most recent definition of osseointegration is ‘a process in which a clinically asymptomatic rigid fixation of alloplastic material is achieved and maintained in bone during functional loading’.37
The original Brånemark implant was cylindrical and machined, made of titanium which produced successful long-term results, with an 85–99% success rate over 15 years.38 Since the time of original Brånemark implants, the material has evolved predominately into a titanium alloy, with increased strength in order to reduce the implant diameter, to negate the potential for implant fracture and allow for higher loads to be cantilevered. Not only has main constituency of the implant changed, but also the surface topography. The traditional Brånemark has been classified as a minimally rough surface. Different surface topographies and treatments are now utilized to make them more osseoconductive, in order to increase the rate of osseointegration to allow earlier loading of the implant.39 Recently, with the advent of ‘ceramic materials’ like zirconia, there has been an increase in the number of companies producing implants containing zirconia. To date, there are very few longitudinal robust outcome studies on their success and survival.40 The main marketing reason for ceramic implants is to negate the risk of shine-through of metallic implant after placement or, in the future, if the patient develops bone loss and recession.
Implant success and survival
There has been extensive work around the world from different research groups highlighting the survival of implants. In particular, Jemt has published a follow-up of the largest cohort of patients in the world, with up to a 31-year period41 in which he found very high survival rates, ranging from 95–99%, but what does that mean to patients? When looking at success, the implant can be considered and the attached prosthesis as single entities or combined. The complications for each can be broadly divided up into mechanical and biological complications.
Mechanical complications
Mechanical complications tend to occur more frequently and earlier to the overlying prosthesis, with prevalence very much depending on whether it is single crown, bridge or denture.
Technical complications in single implants42
Technical complications in implant fixed dental prosthesis (FDPs)44

Overall, screw loosening is the most common mechanical complication and is considered to be minor, however, it is an intermediate complication when there is loosening of the abutment screw.45 It was reported by Pjetursson et al that abutment or prosthetic screw loosening was the second most common complication for implant-supported reconstructions.43 In Pjetursson et al's systematic review, they found the annual complication rates were 1.15% for implant-supported FDPs, 1.44% for combined tooth implant-supported FDPs, and 2.72% for implant-supported single crowns, translating into 5-year rates of abutment or occlusal screw loosening of 5.6% for implant-supported FDPs, 6.9% for combined tooth-implant-supported FDPs and 12.7% for implant-supported single crowns.43 Uneven distribution of occlusal loads and torque stresses on the various components of the prostheses have been suggested as the cause of loosening or fracturing of screws. With the potential for occlusal loading playing a part in the aetiology of both screw loosening and fracture of the overlying prosthesis, a patient factor that can be overlooked is the potential to brux. A recent study found that patients who brux and did not wear an occlusal splint were seven times more likely to fracture their overlying prosthesis.46
Biological complications
These complications occur in the peri-implant tissues and can manifest as signs of inflammation, bone loss, suppuration and soft tissue dehiscence (Figures 6–8).

Peri-implantitis is now accepted as the most significant biological complication of implant treatment. It has been defined by consensus at the 7th European workshop on periodontology that ‘peri-implantitis’ should indicate change in the level of crestal bone, bleeding on probing (BoP) and deepening of peri-implant pockets and or suppuration.47 Natural non-pathological bone loss is said to exist around implants of up to 0.2 mm a year on average and 0.1 mm around natural teeth.48, 49, 50, 51 For implants, the standard of success is based on the original criteria for dental implants which are Brånemark Mk I (10 mm in length and 3.75 mm in diameter, with a 1 mm polished collar) where the protocol was to counter sink 1 mm below the bone level, which therefore resulted in up to 2 mm of bone loss. Therefore, by definition, success was seen as up to 2 mm of bone loss within the first year, then no more than 0.2 mm each year after that.52 Another reason for this bone remodelling in the first year is due to surgical trauma and, for butt-joint contaminated interfaces, as an immunologic reaction to the bacteria and bacterial products which are typically limited to a few millimetres away from the interfaces.52
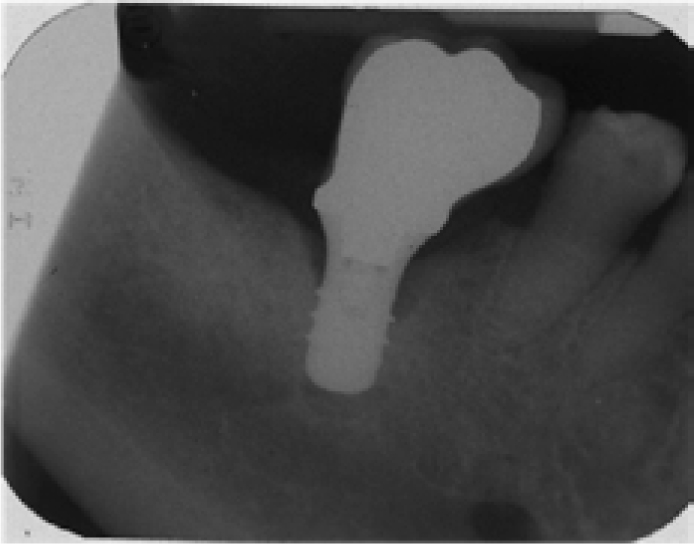
When looking critically at studies which present data on the prevalence of peri-implantitis within a given cohort, there is variation in what the authors define as their criteria of success, how or if baseline radiographs were taken, and the indices used to measure peri-implantitis (BoP, pocket depth, recession, marginal bone loss on radiographs, the reproducibility of the radiographs from year to year).53, 54, 55 Therefore, peri-implantitis prevalence varies from 2–45% of patients in a given population.56 Peri-implantitis can also exist in the form of bone loss around the apical aspect of the implant; this is known as retrograde peri-implantitis57 (Figure 9).
A recent systematic review found that the 5-year rate for soft tissue recession around ceramic abutments was twice that of metal abutments (8.9% vs 3.8%).58 Ultimately, these biological complications can lead to aesthetic problems and it has been stated that the 5-year complication rate was 7.1% (unacceptable aesthetic appearance due to soft tissue recession, an unfavourable colour and visible crown margins).42 More recently, over the last 10 years aesthetic complications have been increasingly taken into consideration. These complications can broadly be divided into pink and white. Pink aesthetic complications are more challenging to correct, for example recession around an implant with exposure of metal can be difficult to manage and, as a result, occasionally these may be explanted and a new implant placed.
Patient factors and clinical outcome
Smoking is a significant factor that can contribute to the failure of dental implants; it has been shown to double the risk of failure when compared to non-smokers.57 This is thought to be due to compromised wound healing in smokers. Although the exact mechanism is unknown, a number of factors have been implicated, such as cytotoxicity of carbon monoxide to tissue cells, vasoconstriction leading to reduced tissue perfusion and compromised polymorphonuclear leukocyte function.59
Patients' susceptibility to periodontitis can increase their risk of marginal bone loss and post-operative infection. It has been found, from a systematic review, that susceptibility to periodontitis doubles the risk of implant loss.58
The factors to consider in patients are:
The age of the patient should be taken into consideration, particularly in placing single implants in the anterior maxilla. Zitzmann et al advised postponing such surgery until the age of 25 to prevent infra-position of the dental implant and possible aesthetic complications.63
Medical conditions that should be considered include diabetes, as patients with uncontrolled diabetes are associated with delayed wound healing and increased rates of periodontal disease. In a recent systematic review it was found that there were increased rates of marginal bone loss around dental implants in diabetic patients, however, overall no significant differences were found in implant failure rates between diabetic and non diabetic patients. The results of this review should be interpreted with caution due to low sample sizes in the included studies and uncontrolled confounders.64
Patients who have received bisphosphonate treatment for osteoporosis, cancer treatments or Paget's disease or, alternatively, treatment with RANK-L inhibitors or anti-angiogenics in oncology treatment are at risk of medication-related osteonecrosis of the jaw (MRONJ). In oncology patients who have received irradiation to the part of the jawbone where an implant is to be placed, it can lead to 25% higher risk of implant failure and, potentially, osteo-radionecrosis.65 In addition, uncontrolled bleeding disorders and treatment with anticoagulant therapies could contra-indicate surgery to place an implant.
Surgical-related factors and clinical outcome
The experience of the surgeon placing implants has been found to have an impact on the outcome of treatment. A recent systematic review found that implants are twice as likely to fail when placed by someone who has placed fewer than 50 implants. Interestingly, they found no significant difference related to the specialty of the surgeon.66
There is no evidence at present to show that implant angulation has an effect on the outcome of treatment. A recent systematic review found that tilted implants compared to axially placed implants did not affect implant survival rates.67 There is, in addition, no available evidence that the timing of loading of an implant has an effect on the implant survival.68
Cost-effectiveness of RCT vs implants
The cost-effectiveness between maintaining a tooth or replacing it with an implant is an important factor to consider when planning treatment.69 Implant treatment not only involves the cost of placement of the implant but other expenditures, such as tooth extraction, bone grafting and maintenance costs arising from any biological or mechanical complications. These ‘extra costs’ can be overlooked when offering implant therapy to patients but are often included in medico-legal claims when funding is to go towards implant placement.
The most cost-effective option has been found to be orthograde root canal treatment, then non-surgical retreatment and then, if that fails, replacement with a dental implant.70 The study by Pennington et al examined surgical endodontics but found it not to be a cost-effective option when compared to replacement of the tooth with a dental implant. This study attempted to estimate lifetime costs and longevity of tooth and implant-supported crowns at a maxillary incisor site. It used a UK-based costing system and a mathematical means of investigating stochastic or random events over time, called a ‘Markov model’. However, in the Pennington et al study they based their data for apical root surgery on a study which was for root resection of periodontally compromised multi-rooted teeth over a 10-year period, which is not akin to the typical situation of maxillary central incisors requiring a contemporary apicoectomy.71 More recent attempts to try and compare the cost-effectiveness of root end surgery to an implant have shown that there are actually higher quality outcome studies relating to surgical endodontics. The study by Torabinejad et al does make a valid point that a contemporary apicoectomy is a one hit treatment and does not require the tooth to be taken apart or multiple interventions to maintain survival.72
In the UK, implants are currently economically inaccessible to the vast majority of patients who want or need them, with only a small proportion of patients being eligible for implants on the NHS.73 For patients who require and are clinically suitable to undergo endodontic surgery, the acceptance criteria is not as limiting in secondary care when compared to those who can undergo implant therapy on the NHS, which is something to bear in mind for a patient who is treated under the NHS remit.
Conclusion
The rising cost of indemnity for implant providers has come about due to the number of litigation cases within the field increasing. The financial quantum of these cases tends to be large and, as a result, it would seem that there is more potential for surgical and prosthodontic problems compared to conventional dentistry. There is evidence of a similar outcome between primary and secondary root canal treatment compared to implant-retained restoration for single teeth. It is now agreed that peri-implantitis is a significant risk for implant treatment, which has made some consider that, on balance, preserving a tooth and saving time in terms of restorative failure cycling is a sensible first step when considering extraction of a restorable tooth/teeth. It is essential that patients are clearly informed of the potential benefits and risks of both treatment modalities. This should include an explanation to high-risk patients that there is no clear consensus on how best peri-implantitis can be managed. In patients deemed high risk of implant complications due to active periodontal disease, poor plaque control or smoking habits, the first line treatment that should be targeted is to try to preserve the natural tooth. Table 1 includes factors that must be taken into consideration when treatment planning these cases, in particular assessing the strategic importance of a tooth, the patient's preferences and the biological and technical impacts that may occur where implant success may be difficult to predict.

