References
Prognostication in periodontics – science or art?
From Volume 45, Issue 6, June 2018 | Pages 496-505
Article

Patients expect dentists to be able to predict the course of a disease like periodontitis, to be able give them some idea of when they can expect to lose teeth and to advise them about the solutions that are available to manage that tooth loss. Indeed, the determination of prognosis carries much weight in the periodontal literature and has been described as ‘an integral part of periodontal practice’.1 But how accurate is a clinician's determination of prognosis? Are there any systems that can be used to help determine periodontal prognosis more objectively? Is there a danger that, with the availability and increasing popularity of treatments like implants, that the temptation is to remove teeth sooner than is advisable? Are implants better than periodontally-involved teeth? These questions represent some difficult decisions and, maybe, ethical dilemmas that will be explored in this paper.
How successful is periodontal therapy?
Periodontitis is a common condition affecting about half the adult population to some degree, with about 10% of the population suffering from a more severe form of the condition that threatens them with tooth loss over their lifetime.2 Such patients may well require restorative treatment to manage their tooth loss but restorative solutions are at high risk of failure without full control of the underlying periodontal pathology (Figure 1). However, even this type of periodontitis can be successfully treated and maintained over patients' lifetimes with appropriate self-care, professional treatment and long-term supportive therapy (SPT). Periodontitis cannot be cured, but it can be controlled; maintenance of periodontal health and the prevention of disease recurrence over a lifetime is dependent on a high standard of self-care, involving both a high standard of biofilm control and patients making the right lifestyle choices (smoking, diet, weight, exercise and so on) that reduces their risk of disease. With these elements in place, all forms of periodontal therapy, both non-surgical and surgical management, can be effective. A 2005 systematic review3 showed that non-surgical therapy was more effective than surgical therapy in increasing attachment levels for initial pocket depths of up to 6 mm, but that surgical therapy may be more effective for pockets over this depth. However, the authors recognized that these findings were based on 12 month results and that longer term studies4, 5, 6 had shown that the long-term results of non-surgical therapy were equivalent to those of surgical procedures, even for deeper sites, with respect to maintenance of mean attachment levels and prevention of tooth loss. This was confirmed in a more recent systematic review7 comparing the long-term effects of four surgical therapies and one non-surgical therapy with follow-up periods of 2–13 years: it was found that most studies favoured non-surgical therapy in terms of attachment level gain, even for deeper initial pocket depths. Such treatment can control periodontal breakdown but it has long been recognized that improvements can only be maintained by ongoing self-care and regular professional SPT, with personal and professional biofilm control being the cornerstone of long-term stability. One study on 75 patients with severe periodontitis who were maintained for 14 years found very little recurrence of disease.8 Axelsson et al presented the results of a 30-year, prospective, controlled cohort study on tooth mortality, caries and periodontal disease progression; the patients who continued to the end of the study (375) were seen for SPT every 3–12 months (depending on individual needs) and tooth loss rates over the 30-year period were low (0.4–1.8), with many of the losses being due to reasons other than periodontitis.9 The evidence therefore indicates that periodontal treatment with proper SPT can maintain periodontal health in the majority over the long term, but it is also recognized that a small proportion of patients will, unpredictably, experience disease recurrence. This is when clinicians start ‘prognosticating’ – trying to predict what will happen to severely periodontally-affected teeth.

Prognosis versus actual outcome
There is no globally accepted classification for determining tooth prognosis in the literature, so much of what is described in this context is subjective, vague and not evidence-based, with terms such as ‘hopeless’, ‘poor’, ‘fair’, ‘uncertain’, ‘dubious’, ‘good’ being used. Attempts have been made to define the ‘hopeless’ tooth; Becker et al10 defined such a tooth as having 75% bone loss, pockets over 8 mm, hypermobility, furcation involvement, poor crown-root ratio and close root proximity or a combination of a number of these features. A major problem here is one of terminology - just using the word ‘hopeless’ implies a lack of hope and what the patient hears is that there is no point holding on to a tooth which has been labelled as having no hope. The loss of a ‘hopeless’ tooth thus becomes self-fulfilling prophecy. It is interesting however to look at those studies in which so-called ‘hopeless’ teeth are retained due to the wishes of the patient to retain them. These studies consistently show high survival rates for periodontally-involved teeth even when teeth are given an unfavourable prognosis (Table 1). Hirschfield and Wasserman12 showed a 92% tooth survival over 22 years, Becker et al,10 a 95.3% survival over 6.58 years and McGuire and Nunn,25, 26, 27 a 95% tooth survival rate over 15 years. Chambrone et al28 conducted a systematic review into predictors of tooth loss during SPT, including 15 studies in the review. It was found that, over a minimum 5-year follow-up period, 73.9% of all teeth assigned as ‘hopeless’ or ‘questionable’ were not lost. Studies show particularly high rates of tooth survival when patients are well maintained; Chace and Low29 studied 455 dubious teeth that were treated and maintained over 40 years in 166 patients in a practice setting, demonstrating that only 12% of teeth were lost, with an average survival of 8.8 years prior to extraction. This is in agreement with a study30 that followed 1535 patients with 2.72 dubious teeth per patient treated over an average of 12.9 years in private practice in which 89% of patients lost no teeth. More recently, Fardal et al31 followed 100 consecutively treated patients with 2,436 teeth for 9–11 years (98.5% of teeth survived) and a retrospective study of 198 patients in SPT32 found a 94.5% survival rate over an average of 11.8 years. Eickholz et al33 conducted a cohort study comparing well maintained and irregularly maintained patients. Overall, patients with regular SPT retained 86% of ‘hopeless’ teeth for 10 years while patients in the irregular SPT group retained 61% of ‘hopeless’ teeth, which led the authors to conclude: ‘…even that rate of tooth loss (39%) over a period of 10 years does not fit into the real meaning of the word ‘hopeless'’. Even patients who have been diagnosed with aggressive periodontitis (AgP) seem to experience surprisingly low tooth loss rates. Graetz et al34 followed 34 patients with AgP and 34 with chronic periodontitis (ChP) during 15 years of SPT. Teeth with 50–70% bone loss were assigned a ‘questionable’ prognosis and those with 70% bone loss or more were regarded as ‘hopeless’. The annual tooth loss rate (TLR) was 0.14 for AgP patients and 0.16 for ChP patients. The authors concluded that ‘…the treatment of periodontally compromised teeth with advanced bone loss is a meaningful therapeutic approach to prevent tooth loss’. A follow-up study of this cohort of AgP patients, published in 2017,35 showed that tooth loss rates remained low overall, but with the risk of tooth loss being increased by smoking, being in the upper dental arch, furcation involvement and mobility.
| Study | Subjects | Years SPT | % Extracted | Annual TLR |
|---|---|---|---|---|
| Oliver11 | 422 | 10.1 | - | 0.05 |
| Hirschfeld & Wasserman12 | 600 | 22 | 8.37 | 0.08 |
| Becker et al13 | 30 | 3.72 | - | 0.5 |
| McFall14 | 100 | 19 | - | 0.14 |
| Becker et al10 | 95 | 6.58 | - | 0.2 |
| Lindhe & Nyman8 | 61 | 14 | - | 0.03 |
| Goldman et al15 | 211 | 22.2 | - | 0.16 |
| Wood et al16 | 63 | 45 | 7.1 | 0.1 |
| McLeod et al17 | 114 | 12.5 | - | 0.15 |
| Tonetti et al18 | 273 | 5.6 | 4.2 | 0.4 |
| Matthews et al19 | 335 | 16.1 | - | 0.06 |
| König et al20 | 142 | 10.5 | 2.95 | 0.07 |
| Fardal et al31 | 100 | 9.8 | - | 0.04 |
| Papantonopoulos21 | 29 | 6.5 | - | 0.01 |
| Chambrone & Chambrone22 | 120 | 17.4 | - | 0.05 |
| Faggion et al32 | 198 | 11.8 | 5.5 | 0.11 |
| Eickholz et al33 | 100 | 10.5 | - | 0.14 |
| Jansson & Lagervall23 | 60 | 16.2 | - | 0.14 |
| Tsami et al24 | 280 | 10.8 | - | 0.31 |
| Graetz et al35 | 68 | 15 | 15.3 | 0.15 |
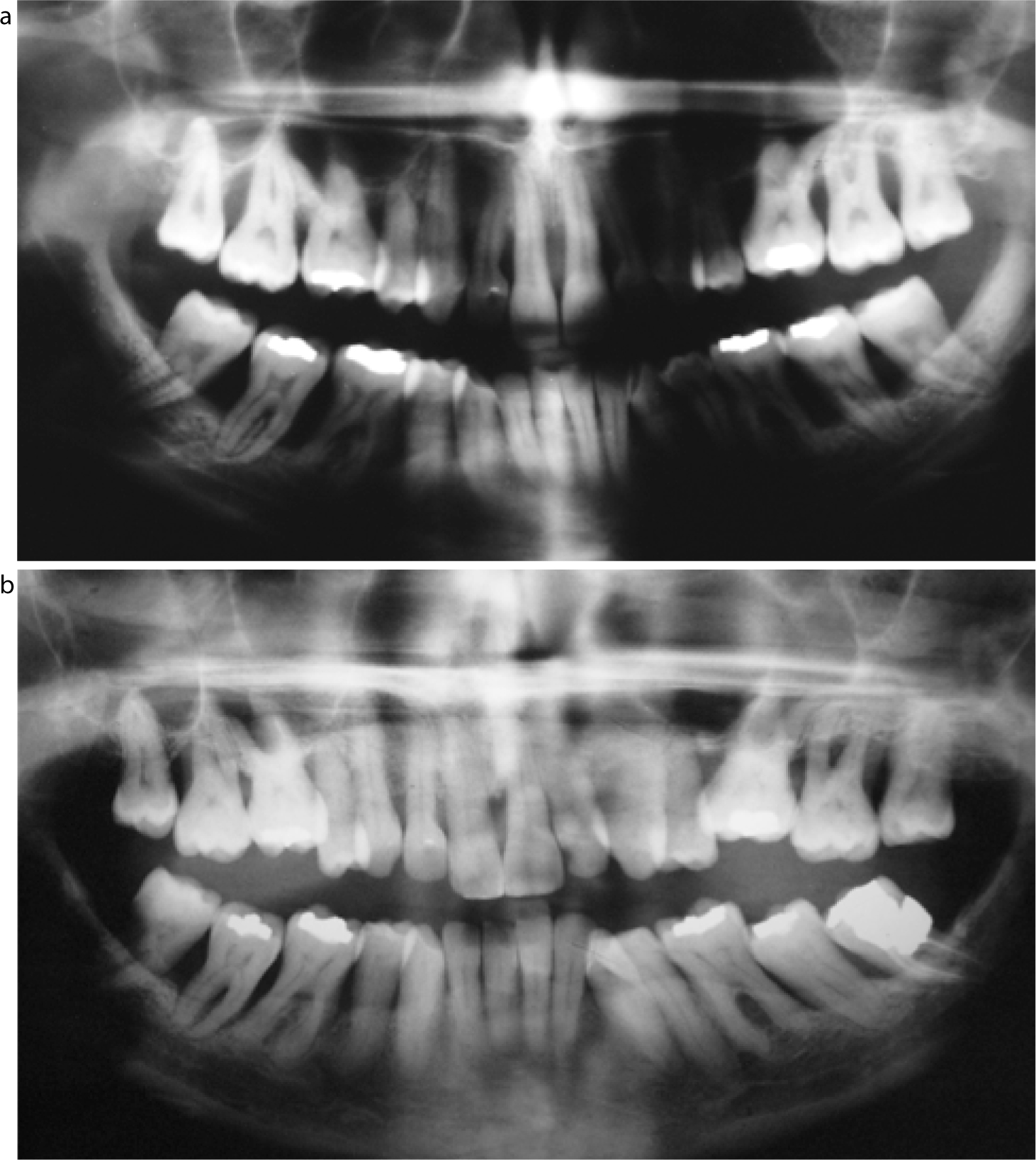
McGuire and Nunn25, 26, 27published a series of papers that followed 100 periodontally maintained patients at 5, 8 and 15 years. There were five prognosis categories of ‘good,’ ‘fair’, ‘poor’, ‘questionable’ and ‘hopeless’. The results showed the inability of conventional clinical parameters to predict any outcome other than ‘good’. In other words, they could find no reliable, clear or predictable relationship between the assigned baseline prognosis and the actual outcome in terms of tooth loss. A clinical example of the unpredictability of tooth survival is illustrated in Figure 2.
Systems for determining prognosis
A number of authors have attempted to devise systems, or algorithms, for helping clinicians to determine prognosis. None of these has been successful. For example, Faggion et al32 tried to develop a prognostic model to estimate quantitatively survival rates for teeth in patients receiving treatment for periodontitis, using 198 SPT patients over a mean period of 11.8 years. In their proposed model they took into account diabetes, bone levels, mobility, tooth vitality and single versus multi-rooted teeth. Overall, they were able to improve prediction of tooth loss by just 14%. They acknowledged that ‘…forecasting tooth survival is complicated by the fact that tooth loss rarely occurs by spontaneous exfoliation but is usually confounded by the provider's treatment decision’. Or to put this another way, as it was in another study: ‘…tooth loss is usually iatrogenic…most teeth can be retained until extraction by a dentist occurs.’1 Importantly, this study also emphasized that prognostication should be regarded as a dynamic process and that it should be re-evaluated as treatment and maintenance progresses. Many clinicians have been taught to determine prognosis at the start of treatment, but this approach fails to recognize that prognosis is influenced by the biological response to therapy and self-care and this response cannot be predicted at the outset.
So what can be deduced from these data? The unavoidable conclusion is that clinicians are not very good at determining periodontal prognosis and shouldn't give the impression that they know what they're doing in this respect when they clearly don't. When discussing these matters with patients words like ‘hopeless’, or even ‘good’, probably shouldn't be used, but doubt and uncertainty should be talked about instead. Or to quote Thomas Jefferson (1743–1826): ‘Ignorance is preferable to error: and he is less remote from truth who believes nothing, than he who believes what is wrong’.
Are implants the answer?
The decision on whether to retain or extract a periodontally-compromised tooth has always been a difficult one, but over the last two decades the goal posts have moved as a result of the advent of dental implants in that there is now the temptation to extract teeth earlier and place dental implants. For some time, when the practice and science of implantology was in its infancy, there was a widely held view that teeth should be extracted while there was still some bone present in order to facilitate implant placement. This was discussed by Kao who suggested the term ‘strategic extraction’, describing this as a paradigm shift that was changing the profession.36 It was argued in this opinion paper that, because of the high success rates of dental implants, there was a shift towards extraction to preserve the bone volume necessary for implant placement. More recently, the goal posts have moved yet again because of data that are starting to show that implants in periodontally-susceptible patients have a significantly higher risk of failure and that, over the long term, implant survival rates do not exceed those of teeth.
How do implants fare in periodontally-susceptible patients?
It is widely accepted that implants should not be placed when there is active periodontitis present largely, it is thought, because of the transmission of periodontal pathogens from residual pockets to the implants.37It has been shown that periodontal patients with pockets over 5 mm, who have been provided with implants, have a greater risk of developing peri-implantitis.38 In addition, the failure to address modifiable risk factors that have contributed to a patients' periodontal diseases in the past will result in patients experiencing significantly more implant complications. The host response in these patients is as important in their peri-implant disease as it is in their periodontal disease. Unsurprisingly then, smoking is associated with an increased risk of peri-implantitis, bone loss around implants and implant loss.39, 40, 41 Ferreira et al41 showed an association between poor diabetic control and peri-implantitis. Oral hygiene and compliance with maintenance visits are also crucially associated with peri-implant diseases – long-term studies have shown a correlation between poor oral hygiene and peri-implantitis41, 42, 43 and Rinke et al44 showed a correlation between peri-implantitis and poor compliance with SPT.
But what about the periodontal patient who is stable, with no residual pockets and control of all modifiable risk factors?
In a systematic review in 2008,45 Ong et al showed that patients who have been treated for periodontitis may experience more implant loss and complications around implants, including bone loss and peri-implantitis, than non-periodontitis patients. This was confirmed by a further systematic review in 201346 which, in addition, showed that the risks are higher if there is a history of aggressive periodontitis. A prospective cohort study in 201247 presented the results of a 3–16 year follow-up of patients with generalized aggressive periodontitis who had implants showing that, in comparison with periodontally healthy patients, there was a 5 times risk of implant failure, 3 times risk of mucositis and a 14 times risk of peri-implantitis. The most recent systematic review examining this issue was published in 2016.48 This review included 27 studies and confirmed the findings of all previous reviews, indicating that the risk of developing peri-implantitis was about 5 times higher in periodontally susceptible patients compared to the periodontally healthy.
What clinicians should be aware of therefore is that a history of periodontitis, even if stabilized, should be regarded as an independent risk factor for peri-implant diseases. Furthermore, the more severe the periodontal disease, the greater the risk of peri-implant disease. The role of the host response in peri-implantitis development should not be underestimated; the Ong, Sgolastra and Sousa et al systematic reviews45, 46, 48 imply that the host response in periodontally susceptible patients may play a crucial role in peri-implant disease development, irrespective of any residual pocket depths. In other words, just as in periodontitis, it's not just about the bacteria.
Many patients still do not realize that they can get diseases around their implants; patients who have been treated in the past for periodontal diseases and who are considering having implants should be advised of what is known and should make an informed decision about whether they wish to accept these risks and proceed with implant therapy or explore other forms of tooth replacement. A failure to explain this to patients, prior to implant provision, could be construed as a breach of duty and renders the clinician medico-legally vulnerable.
One of the key determinants in the survival of implants in the periodontally-susceptible is the long-term maintenance of peri-implant health, both by the patient and the clinician. It is therefore crucial that ‘…implant placement and prosthetic reconstructions need to allow proper personal cleaning, diagnosis by probing and professional plaque removal’.49 This is of particular relevance in the periodontally-susceptible patient, especially when full-arch reconstructions, such as the ‘All-on-4’ concept are being considered, whereby a whole dental arch is replaced by a single implant bridge, since poorly designed appliances which may meet patients' aesthetic needs but which do not allow for probing, personal cleaning and professional maintenance are at high risk of peri-implant disease or failure (Figure 3). Such constructions can, and should, be made in such a way that they can be properly cleaned by the patient and maintained by the clinician (Figure 4).


Tooth survival versus implant survival
Finally, a number of reviews have compared the longevity of teeth and implants, with some surprising results; Tomasi et al50 described the incidence of tooth and implant loss in a systematic review that included studies of 10 years or more, excluding any studies where the drop-out rate was over 30% or if less than 70% of subjects were not followed up for the full 10-year period. Twenty papers were included, 11 assessing tooth longevity and 9 implant longevity. Tooth loss rates varied between 1.3% and 5%, while implant loss rates were between 1% and 18%, leading the authors to conclude that, in clinically well-maintained patients, the loss rate of teeth was lower than that for implants. Levin and Halperin-Sternfield51 conducted a similar systematic review, only including studies of 15 years or longer. Their findings were similar: tooth loss rates were 3.6%–13.4%, while implant loss rates were 0%–33%. Their concluding remarks are worth noting: ‘The results of this systematic review show that implant survival rates do not exceed those of compromised but adequately treated and maintained teeth, supporting the notion that the decision to extract a tooth and place a dental implant should be made cautiously. The decision to retain properly treated and maintained teeth for as long as possible seems to provide an overall solution that can reduce the treatment risks over the long term.’
As teeth seem to survive better than implants, the decision to remove teeth and place implants needs to be justified on functional and aesthetic grounds; in addition, the maintenance of peri-implant health may be more onerous than the maintenance of periodontal health.
At Europerio 8 in London in 2015, the final session was a live 98 minute debate between four giants of periodontology – Jan Lindhe, Maurizio Tonetti, Klaus Lang and Mariano Sanz. The whole debate can be viewed online.52 During this session, Tonetti asked Lindhe whether he would rather have a tooth or an implant. He replied a tooth. Then Tonetti asked, would he rather have a compromised tooth or an implant? ‘A compromised tooth and treat it!’ he responded. That is where clinicians are in 2018 – implants should be a treatment for missing teeth, not a treatment for periodontitis, and, with patients' consent, clinicians should help them to keep their teeth if that is what they want to do. Dentists should also be honest with patients and not tell them what is going to happen to their teeth when the evidence shows that this is not known.

