References
The role of dentists in management of snoring with oral appliances
From Volume 45, Issue 5, May 2018 | Pages 408-412
Article

A recent development in dentistry is the emergence of dental sleep medicine (DSM), which is a recognized branch of sleep medicine that deals with patients who have sleep-related breathing disorders. These can range from ‘simple’ snoring to obstructive sleep apnoea (OSA), which is characterized by repeated collapse of the pharyngeal airway during sleep. Whilst snoring is largely considered to be more of an anti-social problem, with resultant disturbed sleep for bed partners, there is evidence to suggest that this in turn could act as an independent risk factor for Type II diabetes and cardiovascular disease.1,2 OSA and the resultant impaired sleep is associated with a significant cardiovascular and metabolic comorbidity, impaired quality of life and increased risk of motor vehicle accidents.3,4
Dentists are beginning to take notice of their proactive role in this emerging area of special interest in managing patients who have sleep-disordered breathing. First line therapy for symptomatic OSA remains continuous positive airway pressure (CPAP), in view of its proven treatment effect.5 However, the limitations of this therapy relate to significant issues with tolerance, in particular adherence which remains highly variable and has been reported to range from 17−60% and, finally, in a small sample may not resolve the OSA.5,6 There is now an established evidence base for the management of OSA with custom-made, titratable, which permits incremental advancement (3rd generation7), mandibular advancement appliances (MAAs), provided by a dentist with special training.8It is worth remembering that dentists remain the only healthcare providers with both the knowledge and expertise to undertake MAA therapy.
In order to be involved in DSM, dentists need to undergo training in oral appliance (MAA) therapy, have knowledge of sleep-related breathing disorders and established management protocols, as well as having an understanding of how to work as part of a multidisciplinary medical team, in order to build a productive medical and dental collaboration.
It is widely recognized that a large percentage of OSA patients remain undiagnosed and untreated in the UK.9 In this respect, dentists trained in DSM are optimally placed to screen for the presence of signs and symptoms of OSA in their patients. Once identified, dentists can assess for suitability of provision of a MAA and refer to the patient's general medical practitioner (GMP), to help establish a diagnosis. This will entail the GMP referring the patient to secondary care designated Sleep Clinics, where they are likely to undertake an overnight sleep study. The British Society for Dental Sleep Medicine provides this training and access to treatment protocols and a care-pathway, designed to outline this process (www.bsdsm.org.uk).
Clinical practice guidelines
The need for collaborative working between physicians and dentists was recently recognized in the joint publication of the Clinical Practice Guideline for the Treatment of Obstructive Sleep Apnea and Snoring with Oral Appliance Therapy by the American Academy of Sleep Medicine (AASM) and American Academy of Dental Sleep Medicine (AADSM).10 This first official joint clinical guideline supports increased collaborative practice between physicians and dentists for optimal treatment outcome, recommending the use of MAA therapy in regard to the following sleep-related breathing disorders:
Thus, it would appear that the MAA plays a central role in the management of sleep-related breathing disorders, either as first-line or the alternative treatment choice. It remains important that dentists wishing to be involved in this emerging field of Dental Sleep Medicine acquire not only an understanding of the current management of sleep-related breathing disorders and, in the case of OSA, work in conjunction with the Sleep physician, but importantly acquire specialist training to provide MAA therapy. The provision of customized MAAs requires high quality accurate dental impressions of the upper and lower dental arches and, in some instances, a bite registration, with or without a degree of mandibular advancement.
This knowledge transfer remains two-way, with sleep physicians equally being advised to prescribe titratable MAA therapy for OSA adult patients rather than no treatment, in those instances where CPAP is not tolerated or ineffective. This is particularly in light of the fact that lower rates (56−68%) of discontinuation are observed in response to MAA treatment, when compared to CPAP.5,611
In terms of the overall treatment objectives for patients with sleep-related breathing disorders, managed with MAA therapy, the American Sleep Disorders Association, reporting on practice parameters, defines these as the following:12
It is of importance that OSA patients managed with MAA therapy are appropriately followed-up to ensure that they are being optimally treated. This assessment can be in the form of validated subjective questionnaires, as well as objective overnight sleep testing. The latter is particularly important when managing failed CPAP treatment or milder but symptomatic OSA. It is important to recognize that both CPAP and MAA therapy are life-long treatments, which are highly dependent on patient compliance and, as such, require periodic follow-up to help ensure maximum comfort and effectiveness.
Selection of mandibular advancement appliance design
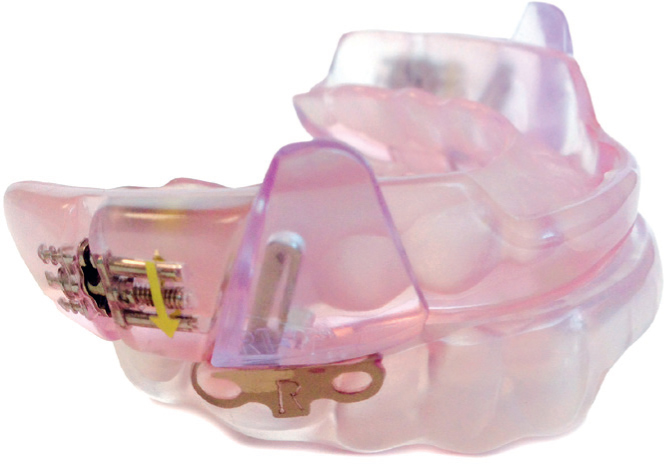
There is currently little controversy in the literature with respect to the selection of MAA design. The optimal properties of what has been described as a 3rd generation MAA have been well documented previously and include: good retention; sufficient mandibular protrusion to maintain airway patency; minimal vertical opening and full occlusal coverage.7 These have been further supported by the AASM/AADSM guidelines, recommending the use of a custom-made, titratable MAA over a non-customized oral appliance.10 The weight of evidence for the use of a custom-made, titratable MAA is supported by the greater reduction in AHI, oxygen saturation levels, quality of life, daytime sleepiness and, importantly, improved tolerance observed with custom-made, titratable MAA therapy.13,14 Given that there is great individual variation in the degree of mandibular protrusion attainable by patients, appliances that permit incremental advancement (titration) offer clear advantages. These include not only minimizing initial patient discomfort, by avoiding the need to posture the mandible forward excessively, but also in obtaining maximum therapeutic benefit, through gradual adaptation and subsequent self-adjustment (titration). Figures 1, 2 and 3 illustrate three such appliances with proven therapeutic value.15,16 Gao et al17 and Tsuiki et al18 have demonstrated the benefit of progressive advancement of the mandible in order to determine the most effective position to treat sleep-related breathing disorders.


Contra-indications to MAA therapy
Whilst MAA therapy has a role in managing patients with sleep-related breathing disorders, it is important that dentists involved in the provision of MAA therapy minimize any later potential complications and impaired quality of life for their patient through a careful initial assessment. The provision of MAA therapy is contra-indicated in the following circumstances:
Side-effects of MAA treatment
The use of these appliances is not without side-effects and they form an essential part of the consenting process, not least because of the long-term nature of their use. In general terms, these can be divided into short term, and of low impact, or long term, with the potential for significant impact.
Short term
With the advent of titratable MAA, many of the previously reported effects of discomfort in the muscles of mastication and dentition can be eliminated, as they are permitted to adapt to the level of mandibular protrusion gradually.19 Patients are likely to report excess salivation and altered bite sensation on awakening; these are reflective of the changes in neuro-proprioceptive responses induced by the forward posturing of the mandible.20,21 These effects are short-lived and the patient readily adapts to them within a matter of weeks.
Long term
These can have a potentially significant impact on the patient and warrant careful explanation:22,23
Conclusions
Dental sleep medicine is both an exciting and very rewarding aspect of care, which not only provides the opportunity to improve the quality of life of patients and their families, but offers dentists the opportunity to be part of a multidisciplinary team designed to manage sleep-related breathing disorders.

