References
Foreign bodies in the nasal cavity: incidental findings during routine orthodontic radiographs
From Volume 45, Issue 4, April 2018 | Pages 351-354
Article

Foreign bodies (FB) in the nasal cavity are an unfortunate but common occurrence in children. The highest incidents are amongst young children 0–5 years-old as they explore their senses and it has been shown to drop significantly after the age of ten.1,2 It has also been shown to be more prevalent in boys than girls.3 FBs in the nasal cavity usually occur unilaterally and the most common objects are seeds, nuts and beads.1
The FB can be classified into two groups, organic and inorganic. Organic substances such as food, wood, paper and rubber absorb water and therefore are more likely to cause an inflammatory response and become symptomatic. These cases will need medical attention. The sequelae of foreign bodies in the nasal cavity include prudent discharge, epistaxis, sinusitis and respiratory symptoms.3,4,5 If left untreated this can lead to mucosal necrosis, cutaneous fistula, rhinolith formation and chronic pain.5,6
Inorganic matter such as plastic, metal and stone are usually inert and can remain in situ and be asymptomatic for many years before being discovered, often as incidental findings.7,8,9 However, there are two inorganic objects that are very hazardous on inhalation/ingestion; they are magnets and batteries. Children are known to try imitating adult piercing using magnetic jewellery, such as those worn on the nose. They are often made of a type of magnet called neodymium, produced by mixing iron, boron and neodymium powders before pressing them into the required shape. This type of magnet is considered to be the strongest available, being five to ten times stronger than plain iron magnets.6 The magnetic force can be so strong that it can cause pressure necrosis just after a few hours, inflicting severe pain and making the use of metallic instruments for their removal problematic. The second objects, button batteries, spontaneously leak alkaline electrolyte when exposed to moisture and can cause liquefying necrosis of adjacent tissues.10 The size and shape of button batteries, that is round and smooth, also make them the most challenging to remove.5,11 The lack of symptoms can lead to late diagnosis and thereby increase the risk of complications.
Techniques used to remove FBs include direct instrumentation using forceps, Foley catheters, suction, nasal wash, positive pressure and adhesives.5
An FB in the nasal cavity also runs the risk of aspiration, therefore careful removal as soon as it is detected is indicated.5,12 Dental radiographs used to assess the full dentition and jaws also capsulate the nasal cavity. It is therefore important to evaluate the radiograph and patient's history thoroughly and consider FB as differential diagnosis on interpretation of dental radiographs.
Here, two cases are presented in which FBs were an incidental finding on orthpantomographs (OPTs) discovered prior to orthodontic treatment.
Case report 1
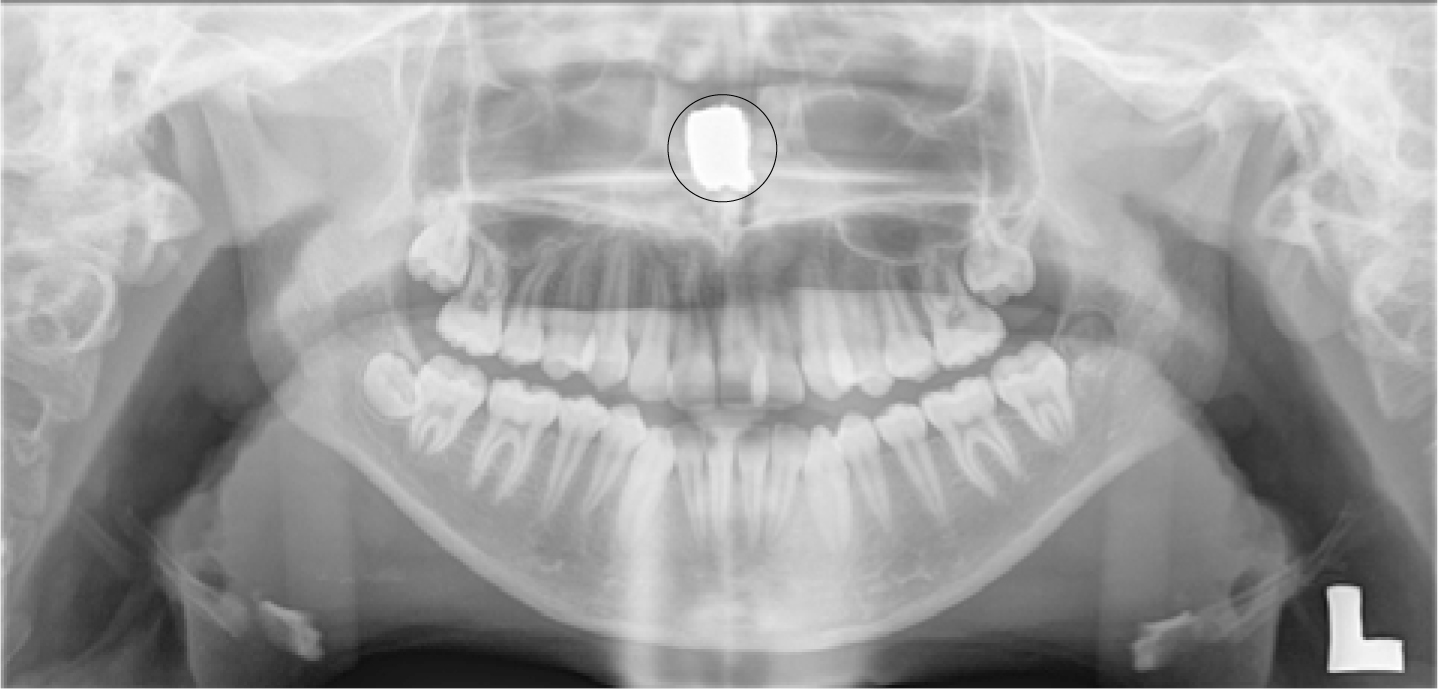
A 13-year-old female, LB, was referred to Derby Teaching Hospitals NHS Trust Orthodontic department, as she was unhappy about her ‘crooked teeth’. The patient gave a history of not being able to breath through her nose properly and had been under the care of the ENT team for three years prior to her referral to the Orthodontic department. Routine radiographs were taken as part of her orthodontic assessment, upon which an incidental finding of a foreign body in the nasal cavity was discovered. The object was very radio-opaque, cylindrical in shape, with dimensions of approximately 15 x 15 mm in size and located mid-point, anteriorly of the nasal cavity (Figures 1 and 2).

When questioned, the patient did not recall any trauma or possible foreign body incidents.
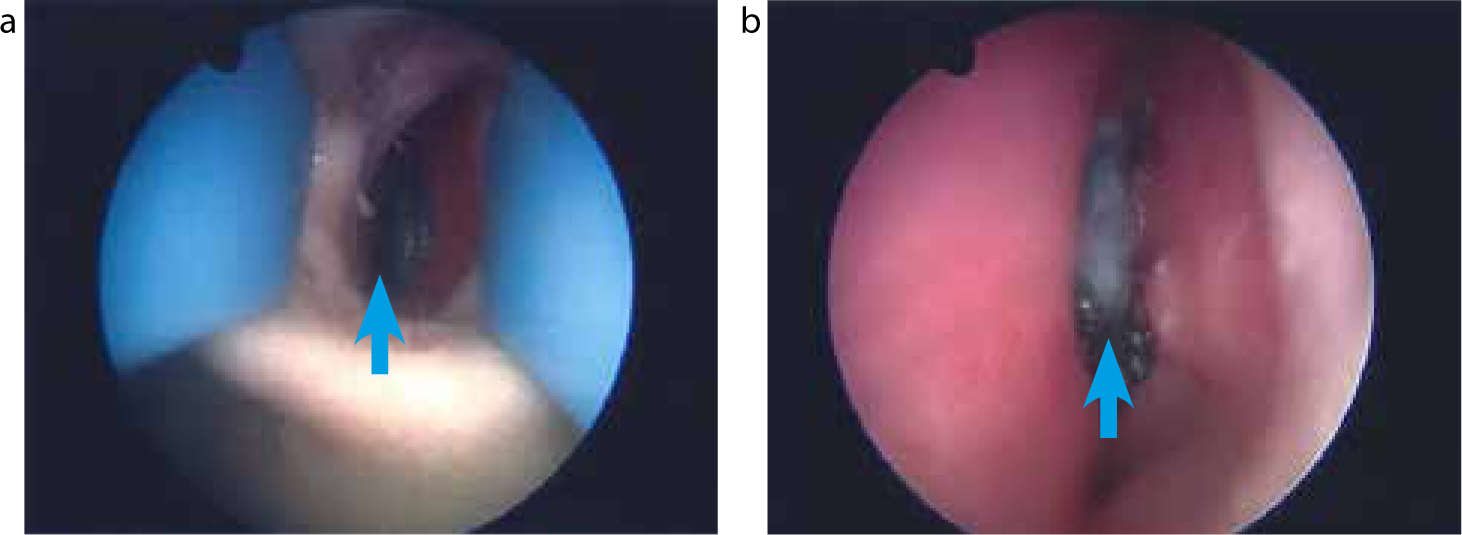
The patient was subsequently transferred to ENT and the foreign object was successfully removed by endoscopic surgery under a general anesthetic. The FBs were two spherical magnets amalgamated together, measuring 15 x 20 mm in size.
It was not until after the removal of the foreign object that the truth was elicited from the patient. It transpired that she was given a science kit for Christmas a few months before and decided to experiment to see if the magnets would work between her two nostrils! They certainly did and the force was so strong she was unable to remove them. She was too embarrassed to tell anyone and even to admit to it when they were discovered on the radiographs. Since the magnets were so firmly fixed together and had been present for at least three months before removal, this resulted in perforation of the nasal septum (Figures 3 and 4). The patient recovered well and proceeded to undergo her orthodontic treatment.
Case report 2
An 11-year-old male, LH, was referred to the Orthodontic department at Derby Teaching Hospitals from his general dental practitioner (GDP) due to his extensive hypodontia. An OPT was enclosed, which showed the patient to be in mixed dentition and having congenitally missing upper right lateral, both lower second premolar and all second and third molar teeth. There appeared to be a faint halo opacity approximately 10 mm in size, just above the nasal cavity floor lining and adjacent to the developing upper right canine apex (Figure 5). There was no mention of this from the referring practitioner.
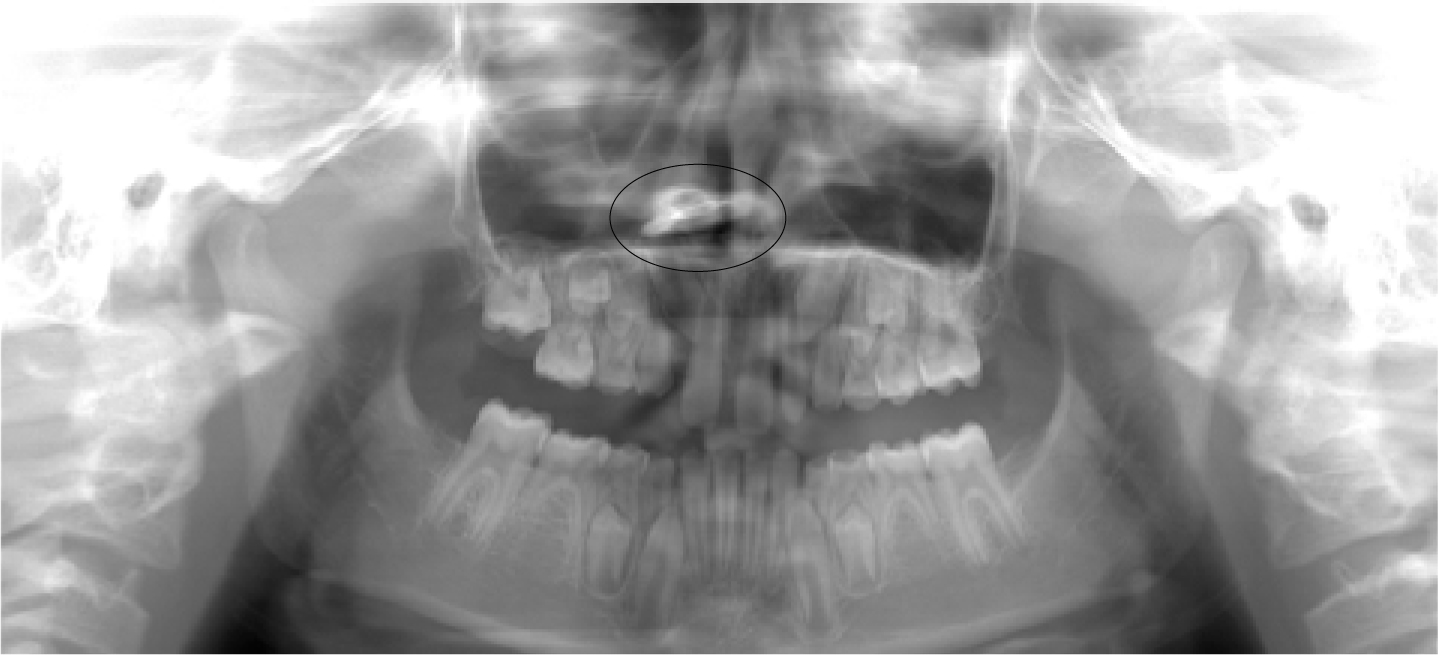
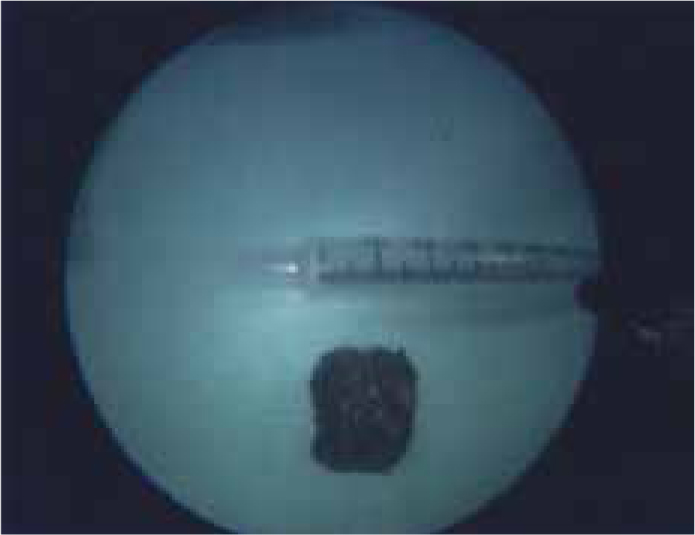
The differential diagnoses included a foreign object and radiographic artefact. A radiologist's opinion was sought, who advised a repeat of the OPT in six months. This was carried out and subsequently gave a clearer diagnosis that it was in fact a foreign object (Figure 6). The culprit was a button and it was successfully removed by endoscopic surgery under a general anaesthetic (Figure 7). The patient recovered well and has since started his orthodontic treatment (Figure 8). The patient's mother informed us that the patient had suffered from terrible halitosis prior to the removal of the button. However, the patient still maintains, even after removal of the foreign body that he has never ever pushed a button up his nose!



Discussion
The cases reported above have outlined common FB injuries that have been found in the nasal cavity but on older children.13 Their incidental findings illustrate the importance of thorough analysis of radiographic imaging in identifying FB injuries in children,4,8,14 particularly given the oversight in the histories given by the patients that exemplifies the length teenagers will to go to conceal themselves from embarrassment.
In both cases, there were signs and symptoms representative of dislodgement of the FB in the nasal cavity, which were: difficulty in breathing through the nose and halitosis of the nasal cavity, respectively. Nevertheless, in neither case was the presence of FBs suspected or explored, leading to a delay in diagnosis and treatment.
In LB's case, she had been investigated previously for breathing problems and it was immediately concluded that the foreign objects had been present for a long time. Close questioning, however, confirmed that the magnets had been in position for a relatively short period of time, so her nasal septum had been compressed between two spherical neodymium magnets for more than three months only. The strength of the magnets was so strong they had fused together and had to be removed as a unit (Figure 3). Much earlier detection or, indeed, confession by LB and removal of the magnet could have prevented her resultant perforated septum.6,15
In the case of LH, the GDP's OPT was inconclusive of a FB and, as the patient concealed his symptoms, this led to a delay in the diagnosis. However, on reflection, it could be reasoned that an upper occlusal radiographic view would have been justified and could have led to an earlier diagnosis of the FB. This also demonstrated the lengths that LH was willing to go to in order to conceal the presence of a FB in his nasal cavity.
Conclusion
The presence of a foreign body in the nasal cavity should be a differential diagnosis for cases presenting with symptoms relating to the sinus, especially in children. Dental radiographic imaging, principally OPTs that are often used to assess the developing dentition, also provide a good overview of the nasal cavities. Therefore, it is important to evaluate the OPT thoroughly and investigate any suspicion of a foreign object within the air spaces. Early detection and removal of a FB is paramount in order to prevent any permanent damage and in resolving the patient's symptoms and discomfort.

