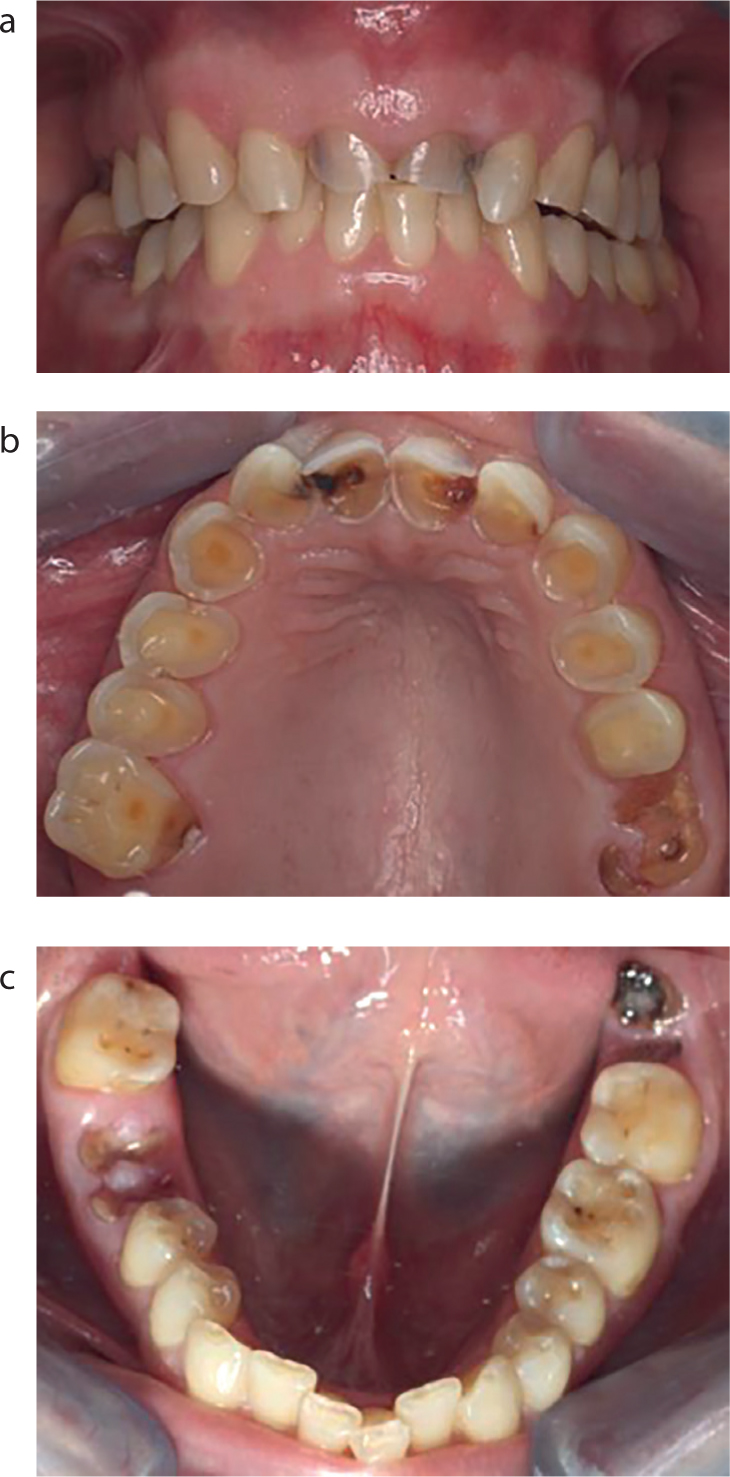
Abstract
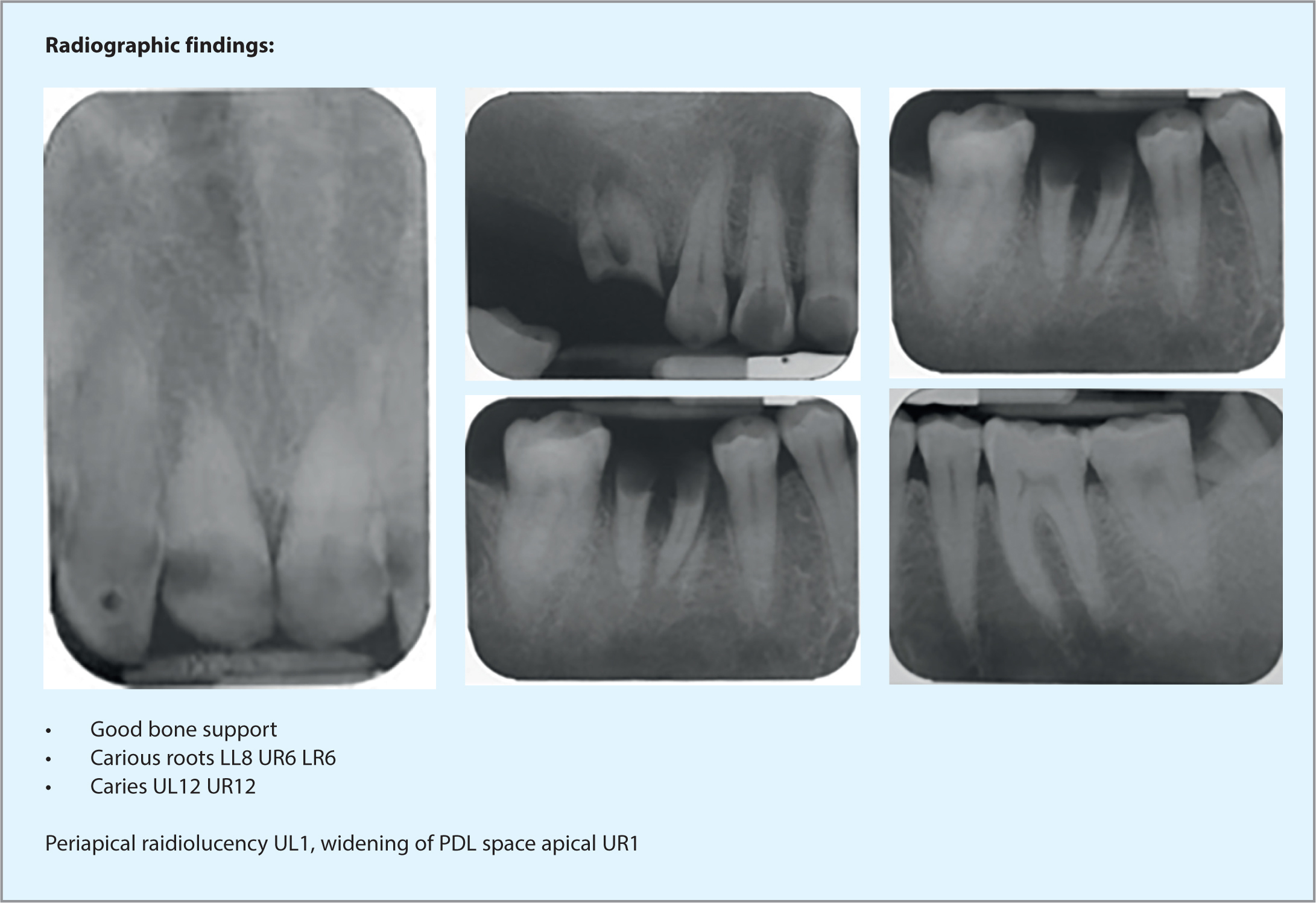
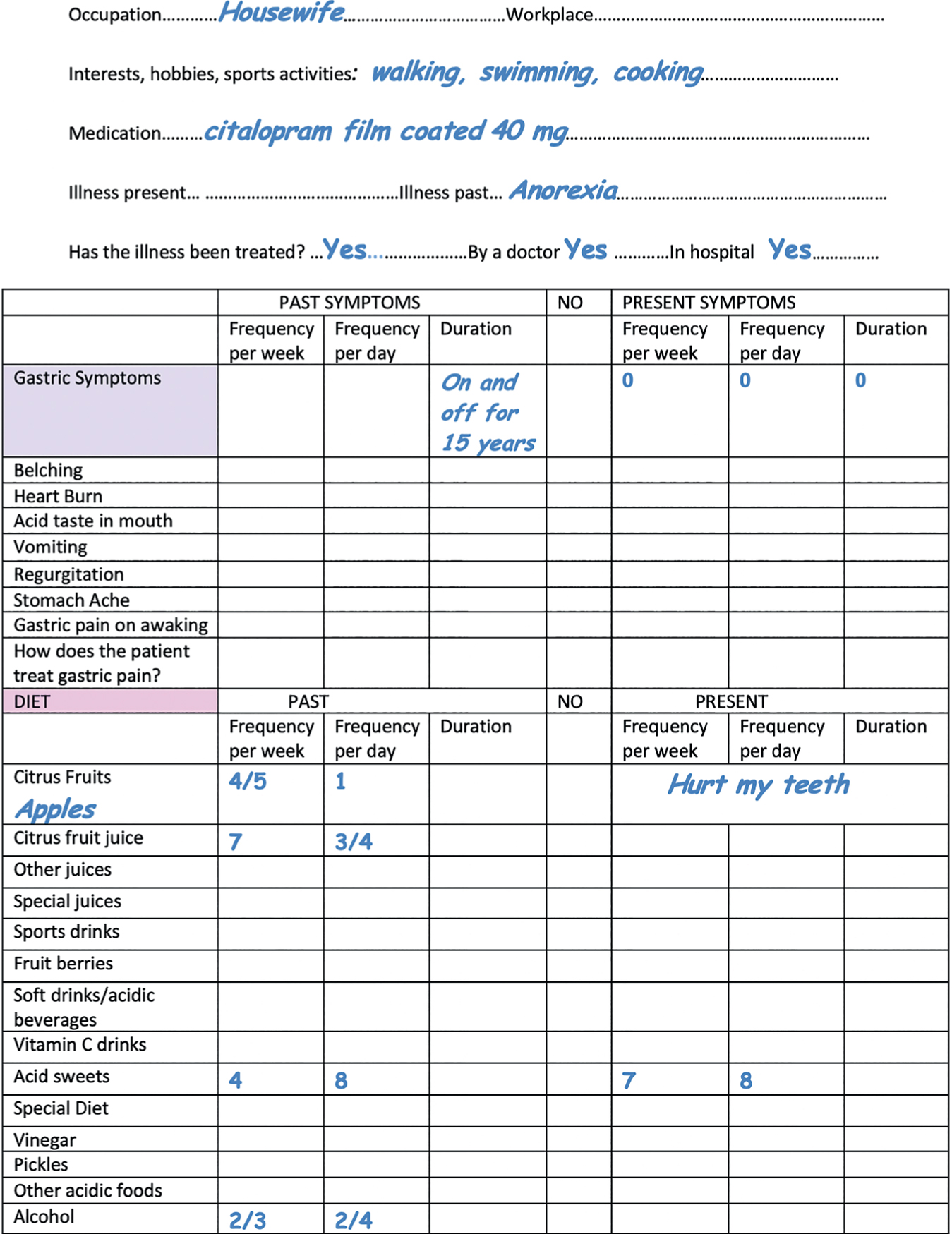
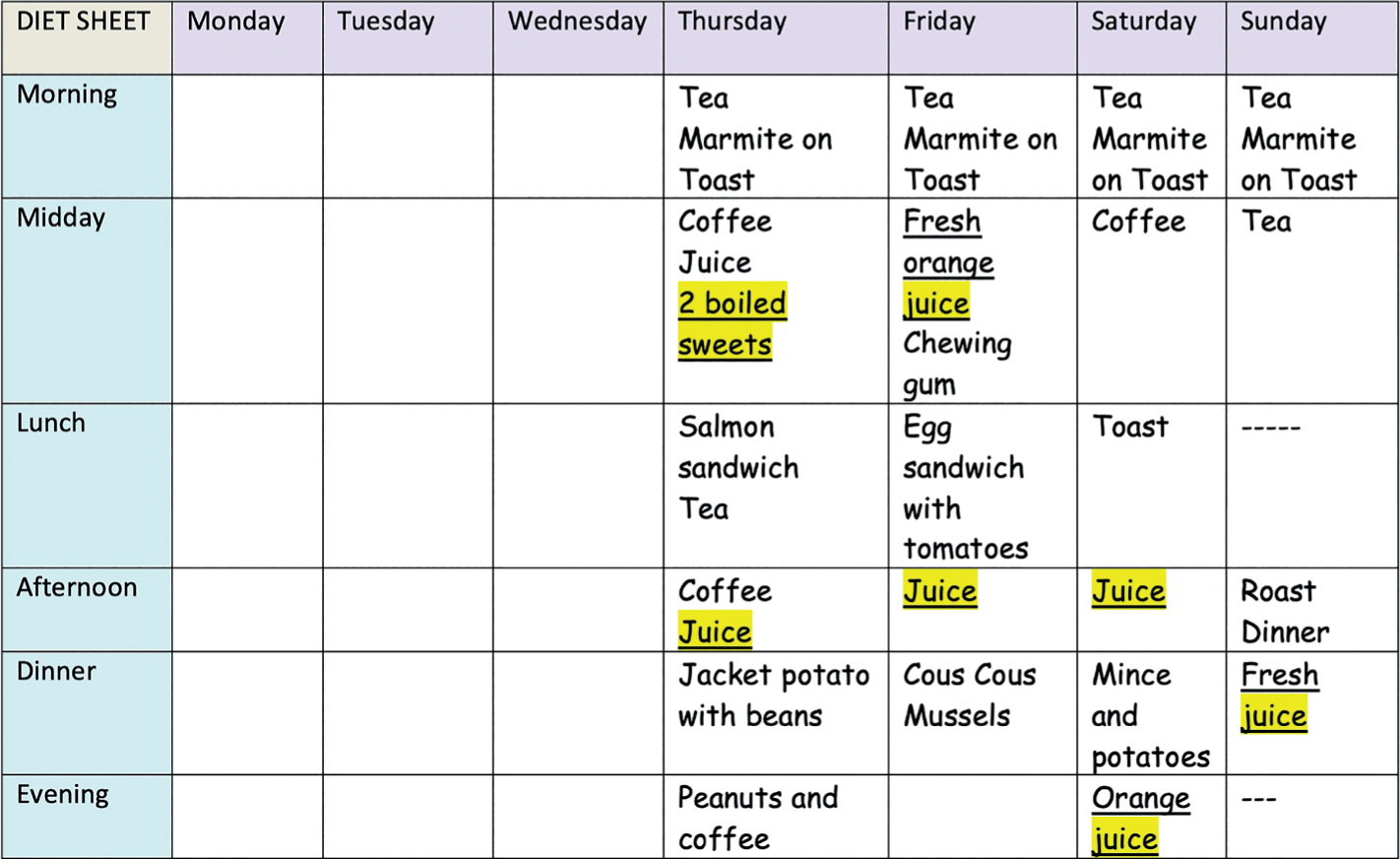
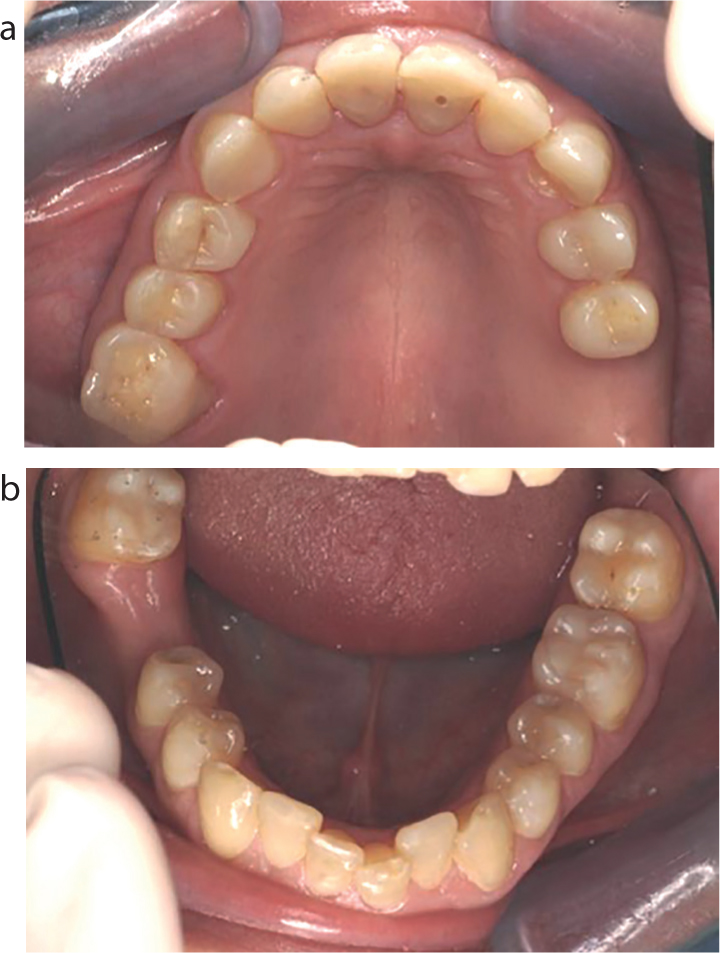
This paper presents a case demonstrating treatment of localized severe toothwear and generalized moderate toothwear, in a previously bulimic and anorexic patient. The treatment plan and rationale for treatment is discussed. The case shows the analytical diagnostic steps taken to formulate the treatment plan, which focused on prevention, treatment of disease and restoration of teeth affected by toothwear, in order to achieve the objective of establishing oral health, function and aesthetics.