References
The application of occlusion in clinical practice part 1: Essential concepts in clinical occlusion
From Volume 45, Issue 11, December 2018 | Pages 1003-1015
Article

According to The Glossary of Prosthodontic Terms 9th edn, the term ‘occlusion’ has been defined as: ‘1. the act or process of closure or of being closed or shut off; 2. the static relationship between the incising or masticating surfaces of the maxillary or mandibular teeth or tooth analogues.’1 However, given that the masticatory system includes anatomical components beyond the occluding surfaces, an alternative definition has been proposed that describes occlusion as ‘an integral (but not necessarily central) part within the stomato-gnathic system (SGS) that relates teeth, not only to other teeth but, importantly, to the other components of the SGS during normal function, parafunction and dysfunction’.2 Accordingly, the SGS includes the temporomandibular joints, muscles of mastication, the periodontium along with the mandibular and maxillary teeth. Indeed, it is common to refer to the articulation of the teeth as the anterior determinants of mandibular movement and the temporomandibular joints and associated structures as the posterior determinants.3
The topic of clinical occlusion which, of course, not only embraces the theoretical aspects but also the more pragmatic/practical elements, does, however, have the potential to cause confusion amongst dental practitioners. Some of this confusion is likely to stem from:
Consequently, many practitioners may inadvertently fall into a habit of not giving the subject of occlusion the level of attention that it may duly deserve,4 which may result not only in restorative failure, but also contribute to other problems affecting the SGS.
The aim of this series of three articles on clinical occlusion is to provide an account of many of the concepts surrounding this subject in relation to the dentate (or partially dentate patient). Part 1 will focus on the occlusal assessment and the proposed features of the ‘ideal occlusal scheme,’ Part 2 will aim to provide an account of the process of taking of occlusal records and, in Part 3, the manner by which the application of the information obtained from any evaluations and assessments can be used to plan and provide restorative treatment will be described. Where possible, throughout this series, clinical case examples will be used to help convey the significance and application of the subject matter to routine practice, with the ultimate goal of helping to improve the delivery of patient care.
The occlusal examination
As per the FGDP (UK) Clinical Examination and Record-Keeping; Good Practice Guidelines 2016,6 when a patient attends a practitioner for the first time for a routine dental examination, an appraisal of the nature of the occlusion would be recommended and, where appropriate, the presence of any occlusal abnormality or disharmony ascertained. Given that the relationship and alignment of the dental arches is one of a dynamic nature (especially evident amongst the developing dentition, in cases of active tooth surface loss, amongst patients with periodontal disease, in the presence of mesial drift and the tilting, drifting and over-eruption of teeth into extraction spaces),2 there may also be an indication to perform occlusal assessments during recall examinations, to take account of any changes that may have taken place since the previous dental inspection.
It has been suggested that, in the case of a new patient attendance (as part of essential practice), an assessment should be made of; the occluding surfaces of the teeth, the incisal angle and molar relationships, as well as an evaluation of the tooth-related guidance during lateral excursive and protrusive mandibular movements.7
In the context of restorative dentistry (with reference to dentate or partially dentate patients), there are however, some specific clinical scenarios where the patient's presenting signs and/or symptoms, or indeed the actual proposed treatment plan/treatment provided would support the need for a comprehensive occlusal assessment.
These include:
The means for carrying out such assessments is described below.
The protocol for the undertaking an occlusal examination
The undertaking of an occlusal assessment will allow the clinician to carry out an appraisal of the clinical features that may diverge from the ‘ideal.’ The concept of the ‘ideal occlusion’ has been discussed further below. However, prior to carrying out the process of conducting a clinical examination, it is of course important to attain (and keep contemporaneous records of) a detailed, accurate and contemporaneous patient history, so as to help establish an appropriate diagnosis. The process of carrying out the examination may be divided into the extra-oral and intra-oral aspects, respectively. The account given below will also focus on matters that are most relevant to the restorative dental practitioner.
The extra-oral assessment
Given the role of the TMJ and associated musculature in the articulatory system, the occlusal assessment should commence with an extra-oral examination of these components. The process of undertaking a TMJ and muscle examination has been described by Gray and Al-Ani.10 This aspect of the clinical assessment should aim to assess the following.
The range of movement
The degree of maximum mandibular opening should be determined by measuring the interincisal distance; any distance less than 35 mm is considered to be restricted. The degree of maximum movements upon the undertaking of lateral movements should also be determined; the normal is accepted to be about 12 mm. A note of the presence of any mandibular deviation upon opening and closure movements is advised.
TMJ tenderness
The presence of any TMJ tenderness may be initiated by the palpation of the anatomical features in the pre-auricular region, and by palpation involving the placement of the index fingers into the external auditory meati and concomitantly asking the patient to open and close, while attempting to manipulate gently their mandible into its retruded arc of closure.
Joint sounds
The detection of any anomalous joint sounds (ideally with the aid of a stethoscope). It is appropriate to note the presence of a ‘click’ and, if present, to determine whether the click may be associated with the symptom of pain. The presence of a single or multiple clicks and the point of the opening/closure cycle when the sound is heard (early or late) should also be established. Variations may help to determine a likely diagnosis. The presence of ‘dislocation’ or ‘crepitation’ sounds should also be noted.
Muscular examination
The muscular examination should involve the bilateral palpitation of the masticatory muscles. This is performed by pressing the muscles between the thumb placed extra-orally and index finger intra-orally whilst concomitantly noting the presence of hypertrophy, tenderness or discomfort, particularly in areas of muscle insertion. The anterior and posterior temporalis muscles and the superficial and deep masseter muscles are perhaps the most relevant in this context. Some clinicians also aim to assess the anterior digastric, sternomastoid, trapezius and medial and lateral pterygoid muscles, respectively. Masseteric hypertrophy has been associated with the pattern of wear by attrition.
The skeletal relationship of the jaws
As part of the extra-oral examination, the skeletal relationship of the jaws should also be ascertained, as this can have an important effect on the dental arch relationship. It is perhaps most common to describe the anteroposterior pattern with the mandible at rest or with the teeth in the intercuspal position. A Class I relationship occurs where the mandible is normally related to the maxilla; Class II when the mandible is positioned posteriorly relative to the maxilla and Class III when the mandible is too far forward: this can have an impact on the facial profile when viewed from the side with the patient's teeth in occlusion (Figures 1, 2 and 3).



Facial symmetry
An assessment of the patient's facial symmetry should also be performed, as well as an evaluation of the amount of maxillary incisal edge display at rest (in mms), commonly referred to as the lip line.7
Occlusal vertical dimension
The term occlusal vertical dimension (OVD) refers to the vertical distance between two selected anatomical points when the maxillary teeth are occluding with the mandibular teeth. The loss of tooth tissue may be seen amongst cases of severe tooth wear or with the loss of multiple (antagonistic) teeth in general, with some patients developing an ‘overclosed’ appearance (Figure 4). The loss of OVD has been described to have the capacity to affect patient function, comfort and aesthetics.11 The loss of OVD at this stage may manifest as an increase in the freeway space (FWS). The latter represents the difference between the vertical dimension when the mandible is at rest − resting vertical dimension (RVD) and the OVD.

It has been suggested that the physiological FWS should be approximately 2 to 4 mm. Perhaps the most popular way of determining the OVD, RVD and FWS involves the use of a set of callipers or a Willis Gauge. It should be noted, however, that the latter methods are by no means highly accurate.11 Other techniques that can be used for the evaluation of vertical dimension include the use of phonetic assessments (particularly the sibilant sounds), facial soft tissue contour analysis, jaw tracking and the use of electrical muscle stimulation techniques.12 Knowledge of these dimensions can prove important when planning future restorative care, as discussed further in part 3.
The intra-oral assessment
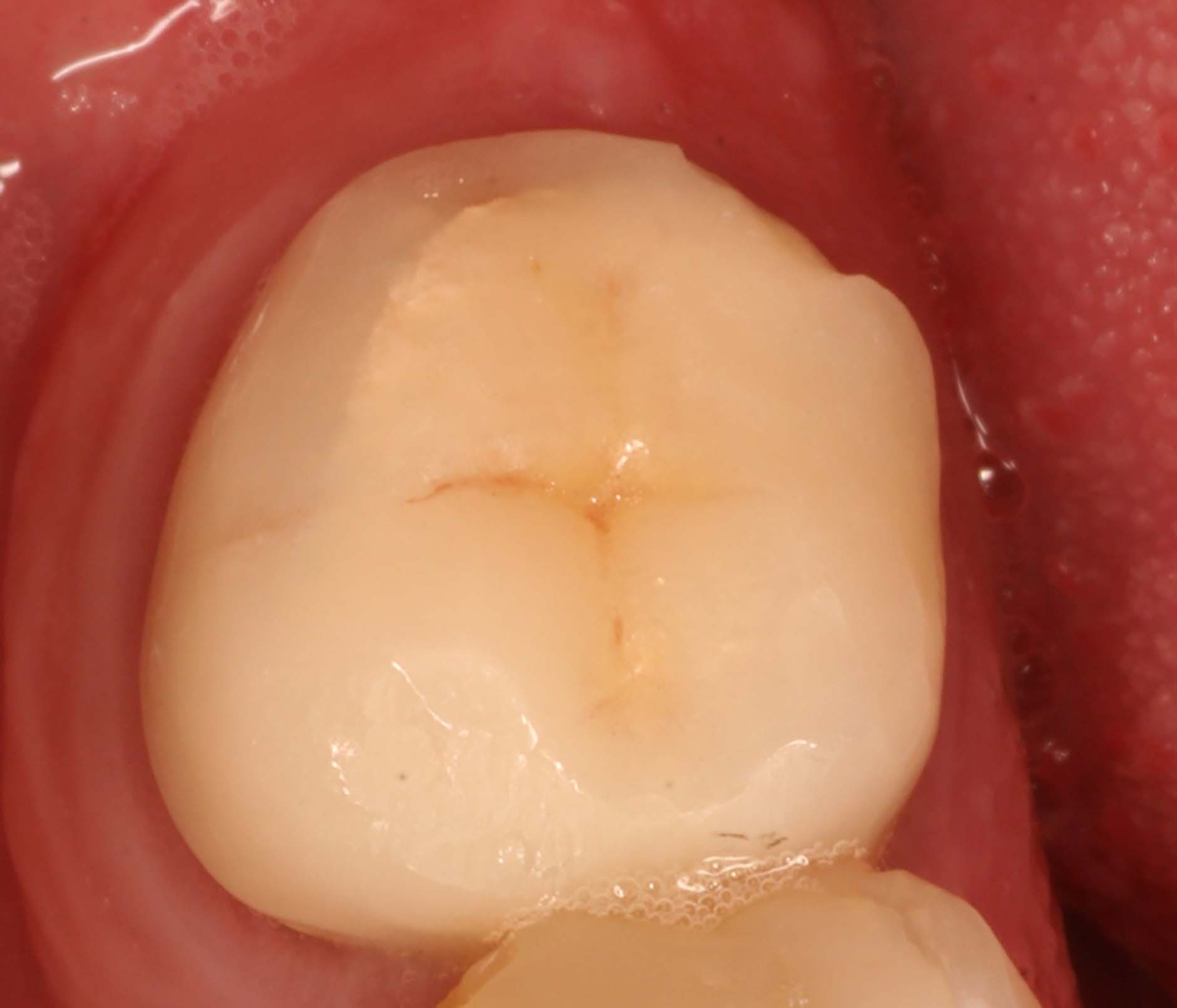
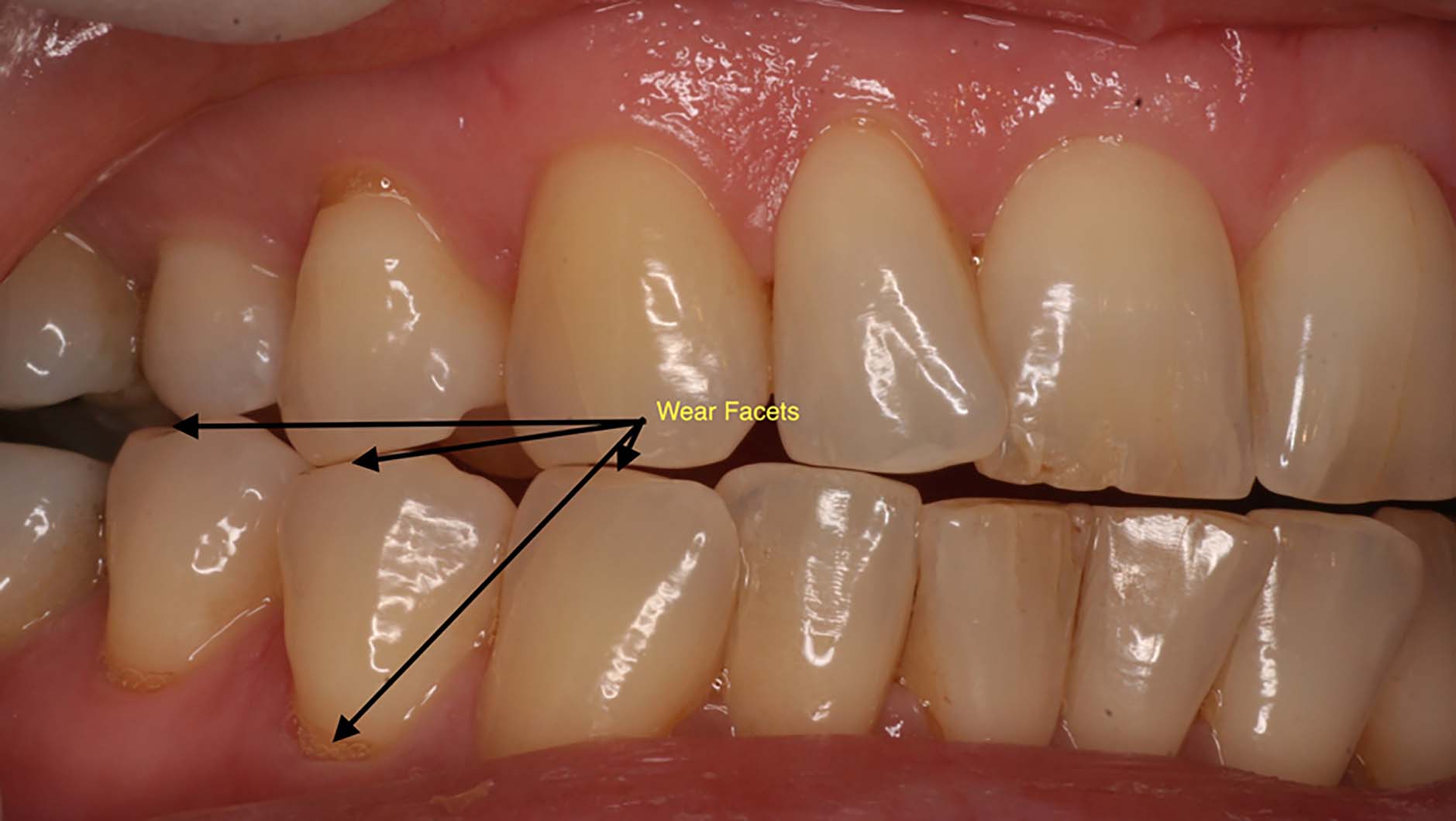
As part of the intra-oral assessment, an overall appraisal should be conducted to take note of features such as; the presence of tooth/restoration fracture(s), wear facets, lesions that may be of abfractive aetiology, vertical enamel fractures,13 dental caries, signs of periodontal pocketing/recession/clinical attachment loss, gingival inflammation, the standard of oral hygiene, the presence of any open contacts with signs of food trapping and tooth mobility (of particular note, the presence of any fremitus). Fremitus has been defined as ‘a vibration perceptible on palpation; in dentistry, a vibration palpable when the teeth come into contact.’1
The occlusal component of intra-oral assessment should also take into account both ‘static’ and ‘dynamic’ components of the patient's occlusal scheme. The latter terms make reference to whether the mandible will be making any movements in relation to the maxilla.4Table 1 provides a summary of the features that should be appraised and recorded during the performance of an appropriate occlusal examination.
| Extra-oral examination: | ||||
|---|---|---|---|---|
| Maximum opening | Inter-incisal distance….mm/Range of lateral movement…. mm | |||
| Joints sounds | Y/N – Click: single/multiple/description……. | |||
| Muscle/Joint tenderness | Yes… No… | |||
| Facial Proportions/well balanced: | Y/N – comments: OVD: mm/RVD: mm/FWS: mm/ | |||
| Skeletal Pattern: | I / II / III | |||
| Facial Symmetry: | Horizontal: Y/N Vertical: Y/N | |||
| Intra-oral examination | ||||
| Incisal Relationship | I / II div 1 / div 2/ III | |||
| Overjet =……………mm | ||||
| Overbite =…………..mm | complete/incomplete | |||
| Super-eruptions:…………… | ||||
| Tilting:…………… | ||||
| Spacing:…………… | ||||
| Crowding:…………… | ||||
| Drifting:…………… | ||||
| Fremitus:…………… | ||||
| Mobility/Grade of mobility I/II/III……… | ||||
| Number of tooth contacts | ||||
| (Shimstock holds)……………………………….. | ||||
| Loss of posterior support………………….. | Y/N | |||
| ICP = RCP/ ICP ≠ RCP | Slide: | vertical; | horizontal; | lateral |
| First point of contact (RCP):………………. | ||||
| Dynamic features/Guidance (chart teeth) | ||||
| Protrusion: | ||||
| Lateral excursion: | Left: |
Right: |
||
The static occlusal assessment
The static occlusal examination should commence by taking note of the presence of any of the following features:
The assessment of the above features will help to establish the presence of any malocclusions, and further categorize the inter-arch occlusal relationships (such as the incisor, canine and molar segment classifications). It is also important to establish the loss of posterior support at this stage, and whether this may be a factor to consider in cases displaying further anterior tooth wear.
Subsequently, the inter-arch relationships that are perhaps most relevant to the restorative dental practitioner are the:
The intercuspal position (ICP)
The intercuspal position (ICP), commonly also referred to as the maximal intercuspal position (MIP), centric occlusion (CO), the bite of convenience or the habitual bite in the dental literature,4 should be initially appraised. The ICP is the position when the maxillary and mandibular teeth are maximally meshed together, when maximum interdigitation (intercuspation) takes place.
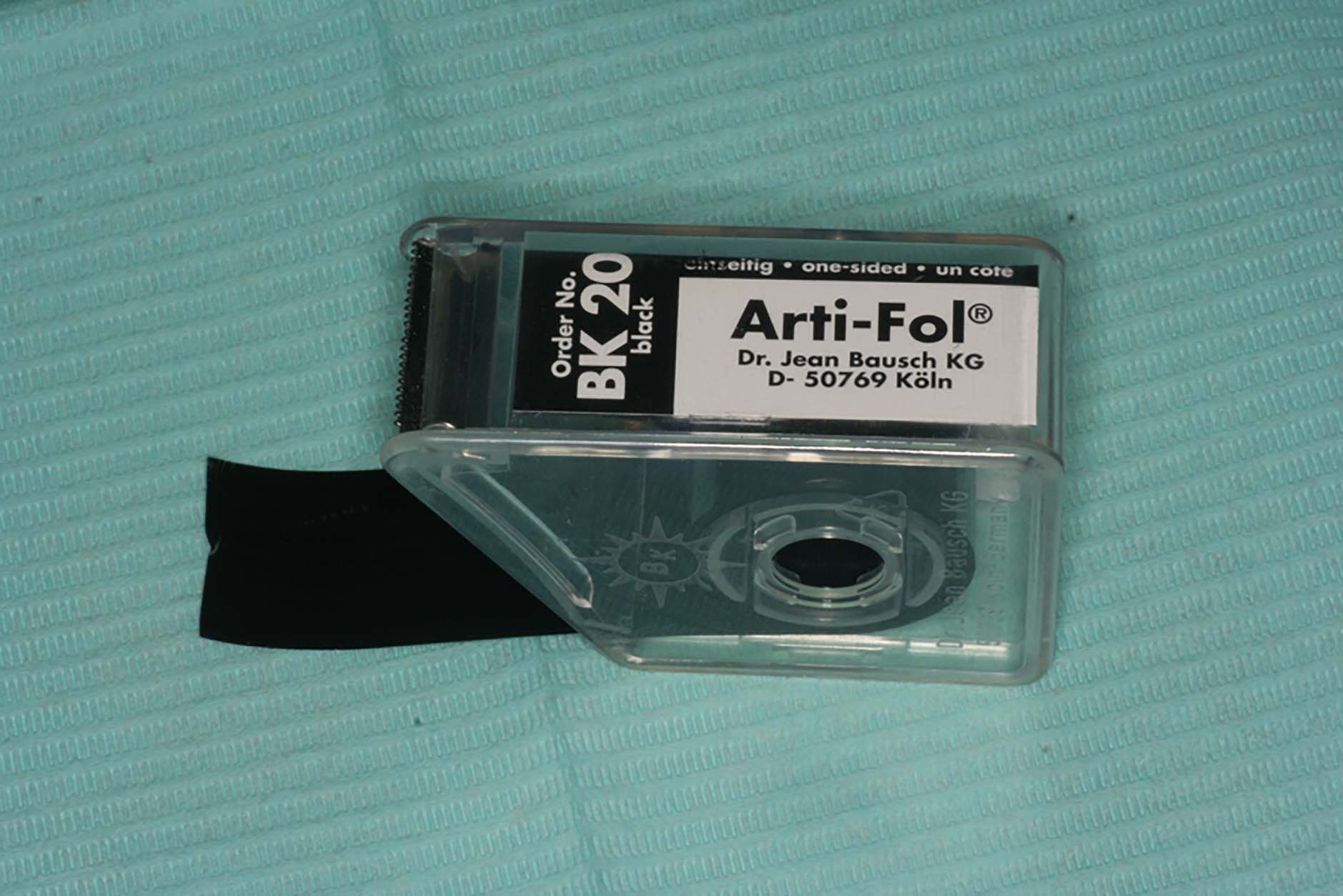
Intercuspal contacts may be identified and recorded using Shimstock articulating foil (usually of 8 to 10 μm in thickness) (Figure 5).13 The foil is ideally supported by a set of Mosquito forceps or Artery forceps (Figure 6).7 Occlusal contacts in the intercuspal position may also be marked up using proprietary articulating paper (ideally less than 20 μm in thickness), however, in order to ascertain a clear recording, it is important to make sure that the teeth are suitably dried.13 The use of GHM Hanel double-sided occlusal indicating paper (GHMDental, GMBH, Germany) supported using a set of Miller's forceps (Artery forceps have also been advocated for this purpose).7 The latter type of articulating paper is available in a small range of differing colours, which can prove helpful when marking up occlusal contacts in differing mandibular positions. It has been suggested that, amongst younger patients (with the absence of any signs of wear), the contacts when marked in ICP should be of the small and discrete variety, with multiple contacts ideally being present on each tooth, which would help to ensure occlusal stability.13 However, where the contacts may be ‘broad and rubbing’, this may be a sign suggestive of possible occlusal instability.13 Single-sided articulating coloured marking foil can also prove useful when identifying occlusal contacts (Figures 7 and 8).



The taking of high quality photographs of the intercuspal contacts, as established by the use of articulating paper, may also prove to be of assistance in relation to the recording and documentation of the findings, as may the use of accurate study/diagnostic casts, as will be discussed in part 2. The use of a digital device such as T-Scan Occlusal Analysis System (Tekscan Inc Boston, USA) to analyse the patency of the contacts in ICP further (in both 2D and 3D) is also gathering popularity.
The presence of any possible fremitus may also be evident by visual inspection and/or by palpation of the tooth/teeth as the teeth make contact in maximum intercuspation.
It is generally accepted that, when undertaking a limited number of restorations that may involve a modification of the anatomical form of the occlusal table, the occlusal endpoint should conform to the existing intercuspal position unless, of course, it may be deemed unstable (indicated by the presence of occlusal instability), or by the signs and/or symptoms of temporomandibular joint dysfunction or masticatory muscle fatigue, respectively.14 This matter will be discussed further in part 3.
The retruded contact position (RCP)
In the sagittal plane (dividing the body into right and left parts) the mandible can only exhibit rotational and translational movement.3 The ease with which the patient's mandible can be manipulated into its retruded arc of closure should be established during the undertaking of the clinical occlusal examination. It has been suggested that the initial rotational movement of the condyles is limited to about 12 mm of incisor separation before translational movements of the condyle down the articular eminence will commence.3 The latter form of movement would be controlled by the action of the temporomandibular ligaments and the anatomical structures anterior to the mastoid process (once the rotational movement has completed).3 Translation has been described to continue up to a maximum inter-incisal (opening) distance of 50 mm.2
The term centric relation (CR) is used to refer to the maxilla-mandibular relationship at the point where the condyles are located in the most anterior-superior position in the glenoid fossae. When the mandible is at CR, only rotational movement of the condyles within the glenoid fossae will be possible. It is thus imperative to be appreciative of the fact that a centric relation, unlike that of the intercuspal position, is a mandibular position that is independent of any given position of tooth contact.
Centric relation is also often referred to as being a fixed and a relatively reproducible position in the dental literature.15 The latter is partly based on the observations that CR has been found to be reproducible within less than 0.08 mm (likely to be accounted for by the non-elastic nature of the TMJ capsule and associated capsular ligaments).15, 16 In addition, given that at CR the movement of the condyles will be one that only displays a simple hinge motion (prior to any translatory movement taking place), this spatial relationship (between the condyles and glenoid fossae) should be transferrable (or perhaps reasonably duplicitous) with that of the condylar housing of the dental articulator, where rotational movements of the condylar component of the articulator will take place against the corresponding articular eminences of this device thereby, to some extent, simulating what may be taking place in-vivo, however, now in the extra-oral environment.
Indeed, most clinicians will most probably be aware from their time of undergraduate training, that CR is traditionally advocated when constructing complete denture prostheses where there is, of course, the lack of any teeth to provide any occlusal guidance. The latter approach will therefore permit the positioning of the teeth that is consistent (‘fixed’) between that of the dental articulator and the patient's mouth, as well as being an anatomical position that is relatively reproducible in the patient's mouth (between successive appointments).
In an analogous manner to the above, it would also seem sensible to use this position as a reference point when undertaking complex occlusal rehabilitation, where the intercuspal position may not be readily identifiable and/or is unstable/undesirable, as in the case of a severely worn dentition, or a heavily restored and failing dentition.17 This approach to treatment planning/provision will not only provide a relatively reproducible reference point that concomitantly serves as a fixed position between the patient and the dental articulator, but also results in a clinical scenario whereby the restored dentition will now display an ICP that is co-incident with the retruded contact position (RCP). The latter is a term that refers to the position of the mandible when first tooth contact occurs during its retruded arc of closure. Where treatment is provided in this manner, it is referred to as a re-organized rehabilitation (and will result in the loss of the slide between RCP and ICP) as discussed further below.
It has been shown that, whilst approximately 90% of adult patients have a slide between RCP and ICP (with ICP being anterior and superior to CR by 1.25 mm +/- 1.0 mm), amongst the remaining 10% RCP and ICP are in fact co-incident.16 Indeed, the discrepancy between RCP and ICP (commonly termed the RCP-ICP slide) may result in a level of inter-occlusal clearance (in the vertical, lateral and/or horizontal dimension) that may prove beneficial when attempting to provide restorative treatment for a patient displaying tooth wear, as the resultant space may be effectively utilized to place restorative materials (when re-organizing the occlusion) and, therefore, in some cases help to alleviate the need to increase the occlusal dimension and/or the need for subtractive tooth preparation to accommodate future restorations.17 It may therefore be relevant to identify the presence, direction and extent of any occlusal slides between ICP and RCP (horizontal, lateral as well as vertical) when planning care for such patients, as discussed further in part 3.
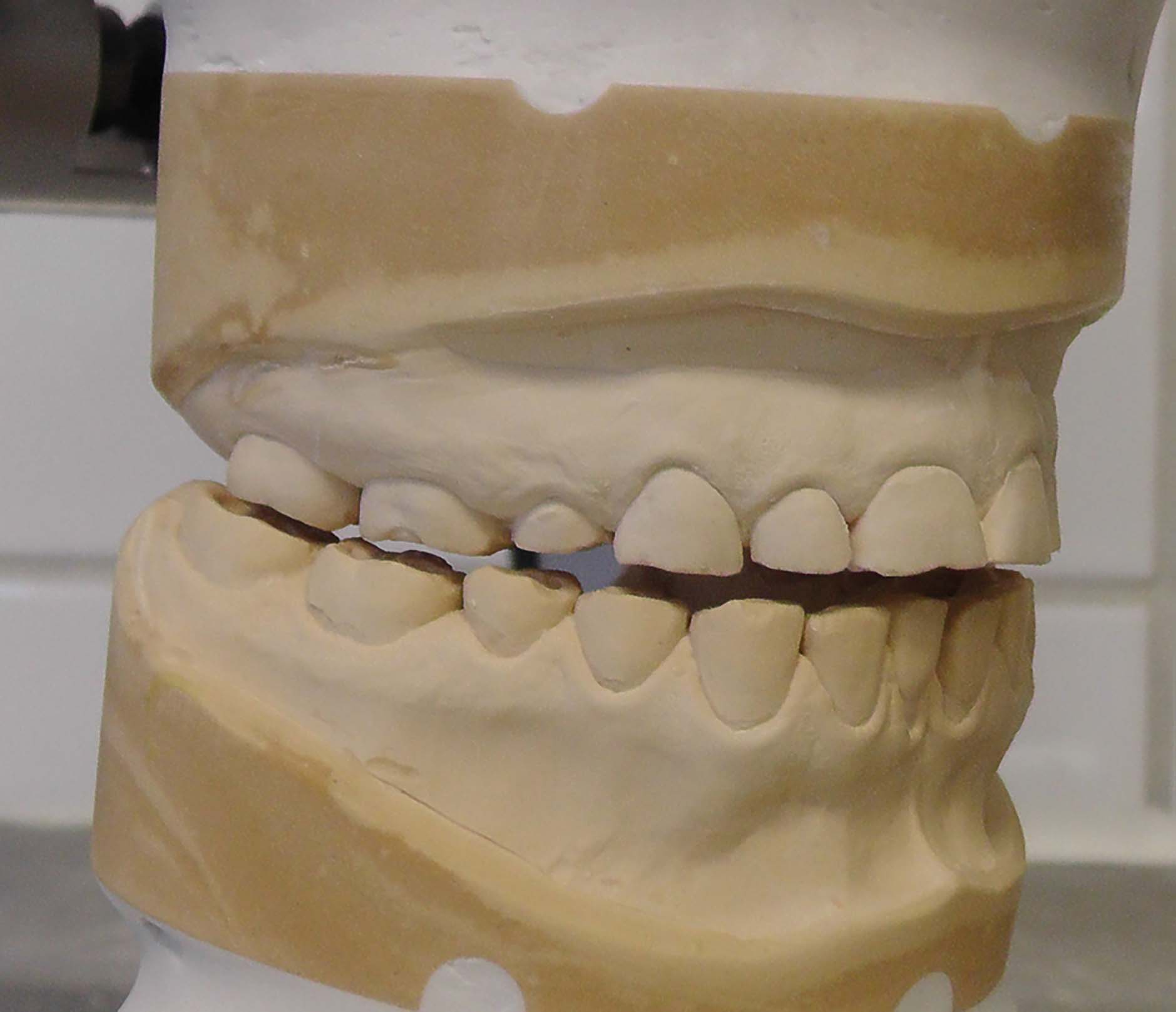
Accordingly, it is appropriate to mount a set of study/diagnostic casts in CR, where RCP can be identified following closure of the elements of the articulator in the retruded arc of closure (Figure 9), which will be the position of the mandible (as per the envelope of movement described by Posselt16) that serves as the starting point (prior to ICP and/or before the taking place of any eccentric mandibular movement). This may be especially relevant when there may be a plan to adjust and/or to re-organize the occlusion (inclusive of the need to increase the OVD, such as for a patient with tooth wear).13, 16, 17 The use of mounted study casts in this manner will allow the assessment of CR/RCP, as well as any movements from this position in the absence of the interference of the soft tissues and the patient's neuromuscular protective mechanisms. The criteria for the mounting of working casts in CR will be discussed further in parts 2 and 3.
Finally, in relation to the term retruded contact position, a number of synonyms have been used. These include; the centric relation contact position (CRCP), the retruded axis position (RAP) or the terminal hinge position (THP).15 The latter can sometimes lead to confusion when trying to develop a better understanding for this concept.
The term ‘long centric’ (or ‘freedom in centric occlusion’) is also often used by clinicians, and requires some further discussion. This concept essentially describes the scenario of being able to close the mandible into RCP (or slightly anterior to it), without altering the vertical dimension of the anterior teeth.2, 4 The absence of freedom in centric can sometimes be seen in cases with Angle's Class II division 2 relationships and/or amongst patients where multiple anterior restorations have been placed (with sub-optimal contour of the occluding surfaces) that will only permit very limited/or no movement when the posterior teeth are in contact, thereby having the effect of ‘locking’ the patient's jaw. The latter scenario is sometimes not very well tolerated. Clinically, however, it may ultimately manifest in pain and discomfort, premature restorative failure and have an adverse effect on the supporting structures, and/or culminate in unwanted tooth movement. This situation may sometimes be seen amongst cases where restorative rehabilitation has been provided for patients presenting with anterior tooth wear.
The clinical location of CR, however, is not always a straightforward matter.7, 15 Whilst this may sometimes be due to the presence of protective neuromuscular reflexes (which may frequently be encountered amongst patients with parafunctional habits), or amongst cases where considerable occlusal disharmony is present,7 there are a number of additional factors that have been described by Wilson and Banerjee that may influence the ease with which CR may be located.15 These include:
A variety of ‘operator-guided techniques’ for the manual manipulation of the condyles (for dentate patients) into the desired position recording of CR have been described.15 The technique of bimanual manipulation, as described by Dawson, is frequently used and warrants further appraisal.18 With this approach, the patient should be comfortably seated in the dental chair in a supine position, with the operator seated directly behind. The operator's thumb and index finger of each hand should be placed behind the angle of the mandible and in front of the angle, respectively, to allow the condyles to be directed antero-superiorly. The middle fingers should be bilaterally positioned on the inferior border of the mandible, the index fingers should be positioned submentally in the midline and the thumbs placed laterally to the symphysis.15 The patient should then be instructed to relax the jaw, and allow the operator to control the jaw movements. The mandible should then be slowly and gently arced upwards and downwards with minimal force. The upward movement should then be gradually increased until the first point of contact is reached. If undertaken correctly, the mandible will be hinged along its retruded arc of closure; it may indeed be possible to palpate this portion of the condyle by placing a finger into the patient's external auditory meatus.
It is important, however, to avoid the use of a forceful action with the above technique, as it may inadvertently push the mandible backwards towards a downward translatory movement, as well as result in some level of mandibular flexion, overall culminating in an erroneous record as well as in patient discomfort (resulting in resistance to the applied load).15
It is also worthwhile asking the patient if he/she may be aware of the side of the jaw where the first point of tooth contact occurs in CR. The patient should then be requested to squeeze the teeth together, with the operator noting the direction of the slide of the jaw into ICP. The first point of tooth contact can be marked up ideally using two different colours of GHM occlusal indicating paper to mark up the slide from RCP to ICP.
In some cases, however (given some of the difficulties described above in locating CR), the use of techniques such as those described above will not allow CR to be properly determined and appraised. Under such circumstances, an alternative approach, broadly involving the use of a variety of anterior de-programming devices, may prove helpful, which in general will aim to overcome the neuromuscular reflexes that are initiated by tooth contact by causing tooth separation and will also provide an anterior reference point/stop to help stabilize the mandible during the act of taking the record. These devices and their clinical application to help identify and record CR will be discussed at length in part 2.
The dynamic occlusal assessment
In relation to the dynamic mandibular movements, it is important to assess the relationships during the lateral and protrusive jaw movements.
The term anterior (or incisal) guidance refers to the guidance provided to the mandible by the contact formed between the palatal surfaces of the anterior maxillary teeth and their antagonists, whilst the term protrusive guidance is used to describe the effect stemming from the combined influence of the condylar guidance (developed between the condyles, fossae and articular eminence during anterior mandibular movement). The angle formed by the path of the moving condyles within the sagittal plane compared with the horizontal plane is referred to as the protrusive condylar angle and has been stated to be of the mean value of 45˚ (within a range of 30˚ to 60˚).2
Where the occlusal scheme is considered to be stable (‘mutually protective’), when the patient displays a protrusive mandibular movement, the anterior guidance coupled with the inclination of the condylar path should collectively aim to separate (or disclude) the posterior teeth from each other (Figure 10), thereby avoiding any harmful occlusal contacts which may otherwise culminate in cuspal fractures, repeated restoration fracture, recurrent decementation of indirect restorations, pathological tooth wear or fremitus. This culminates from the fact that the posterior teeth are closest to the fulcrum, ie the TMJ where the forces are the highest in a third order lever situation. In the position of maximum intercuspation, only light occlusal contacts should exist between the anterior segments, with occlusal loading primarily taking place between the posterior teeth.

The steepness of the anterior guidance provided by the anterior teeth should also be evaluated (often described in the literature as being steep, moderate or shallow). The effect of altering the anterior guidance on the posterior dentition must be carefully evaluated, especially when the clinician may be contemplating a macroscopically irreversible alteration in the anterior guidance, such as during the process of prescribing and providing of multiple anterior crowns. Ideally, the anterior guidance should be shared between the anterior teeth to optimize stress distribution; however, this may not always be possible. Nevertheless, care should be taken to avoid providing protrusive guidance on a single tooth, especially that of a maxillary lateral incisor tooth.2 Clearly, however, the steeper the anterior guidance, the more likely it is that posterior disclusion will take place. In the alternative scenario, however, in the presence of an incomplete overbite, there may be the delayed disclusion of the posterior teeth before the anterior teeth come into contact.
The orientation of the occlusal plane will also influence the anterior guidance. In the case of a curved or steep occlusal plane (to the horizontal), posterior tooth disclusion will take place less readily than in the case of a patient displaying a relatively flat occlusal plane. The manner by which an appropriate level of anterior guidance can be predictably determined when undertaking restorative rehabilitation will be described at length in part 3.
In an analogous manner, the lateral movement of the mandible is also influenced by the tooth relationships, as well as the condyle-fossa arrangement during the undertaking of such movements. The term ‘working side’ is used to refer to the direction in which the mandible has moved during a lateral excursion; the other side being the ‘non-working side’. Lateral guidance to the mandible may be provided by the canine teeth – ‘canine guidance’ (Figure 11) or by multiple teeth, referred to as ‘group function’.

The morphology of the canine tooth makes it a very suitable candidate to provide guidance during lateral excursive movements, as discussed further below. The presence of a canine-guided occlusion/canine-protected occlusion helps to permit posterior tooth disclusion upon lateral excursion, which may otherwise lead to similar undesirable consequences as discussed above. Please note, a dynamic relationship which may initially involve group function may also be frequently observed, but the presence of canine guidance may be noted with further lateral excursive movement (Figure 12).

With reference to the condylefossa relationships that take place during the process of making a lateral excursive movement, the principle movement within the TMJs is on the non-working side (the side away from which the mandible moves in lateral excursion).19 During this action, the head of the condyle moves forwards, downwards and medially. The angle of downward movement is referred to as the condylar angle, whilst the angle of medial movement is referred to as the Bennet angle.19 The latter has an average value of 7.5°.2
The movement that takes place at the working side (which is immediate) is referred to as the immediate side shift or Bennett movement. The average level of lateral movement is approximately 1 mm.2 The effect of the presence of an immediate side shift when undertaking restorative rehabilitation of the posterior teeth has been detailed below.
The presence of any occlusal interferences (which may be considered to be undesirable contacts that occur between opposing teeth in any mandibular position which may cause mandibular displacement on either the working side, the side towards which the mandible moves during a lateral excursive movement, or non-working side, the side away from which the mandible moves in lateral excursion) should also be noted. When undertaking restorative rehabilitation involving a re-organized approach, in the ideal scenario, lateral guidance should be provided by the canine teeth, with the absence of any occlusal interferences on either the working side or non-working side (Figures 13 and 14). However, it is important to appreciate the fact that the presence of non-working side contacts (when not associated with the presence of signs or symptoms of pathology) does not necessarily constitute the presence of an occlusal interference; such contacts may be seen amongst patients with malocclusions or natural occlusal schemes that do not otherwise conform to the mechanical ideal (Figure 15).


Non-working side contacts that are, however, occlusal interferences, may be associated with the presence of the signs and symptoms of:2
Excursive and protrusive contacts can be marked using articulating paper; ideally, they should appear smooth and unbroken.13 It has been suggested that the presence of an irregular, broken or doglegged appearance of the marked contact relationship may be suggestive of an interference on the tooth itself or, indeed, at another location in the oral cavity.13
A number of alternative occlusal schemes have also been described in the literature, such as that of a balanced occlusion (bilaterally balanced occlusion) or unilaterally balanced occlusion. The former is used to describe a relationship recommended when undertaking complete denture prosthodontics, to ensure denture stability during dynamic movements. For further details, please consult a reputable textbook on complete denture prosthodontics.
Good quality, accurate paralleled periapical radiographs may also be indicated as part of the occlusal assessment. It is important to establish the presence of any signs of alveolar bone loss to help establish a diagnosis. Other features that may also be elicited upon radiographic evidence include; the quality of the bone support, the presence of any angular bone defects, the presence of a widened lamina dura, the root surface morphology, anatomy of the pulp chambers of affected teeth, quality of pre-existing endodontic treatment(s), presence of dental caries, widening/disturbance of the lamina dura, presence of retained roots or any signs of periapical pathology (radiolucencies or radio-opacities).8
The effect of the posterior determinant − the TMJ and associated structures
Hopefully, it now becomes apparent that the anatomical relationship between the condyle and the glenoid fossa (particularly as the condyles move against the glenoid fossae) will have a marked influence on jaw movement during mandibular movements in differing directions (as will of course the teeth).
The above can be seen and described in relation to the making of a protrusive mandibular movement, where the steepness/inclination of the articular eminence of the TMJ will have a notable impact (especially in the case of missing anterior teeth/tooth contact or a shallow anterior guidance) on the rate and level of posterior tooth separation. Accordingly, in a patient with a steep articular eminence, posterior discussion will take place relatively rapidly and to a relatively greater extent (than in the case of a shallower eminence). This has practical significance in relation to the design of any posterior restorations or indeed for the diagnosis of oral disease, whereby the tolerance for longer cusps and steeper cusp angles will be greater in the former scenario. Conversely, if the eminence is shallow, the cusps must be kept short to avoid clashing, as the mandible is more likely to pursue a horizontal pathway (in the case of a shallow anterior guidance).3
The axes of rotation of the condyles will also influence the morphology of the occlusal table of the posterior teeth. In order to permit the smooth passage of the antagonistic teeth during a lateral excursive movement, the cusps of the mandibular teeth must pass through the buccal grooves and marginal ridges of the maxillary teeth. In the case of undertaking the restorative rehabilitation of posterior teeth, the presence of an immediate side shift (especially where relatively more movement of the condyles against the medial wall of the glenoid fossae becomes possible) may require the clinician to give further attention to the location of the cusp tips and buccal grooves as the smooth passage between opposing teeth may not take place, often resulting in the clashing of antagonistic cusps. Under such circumstances, it would be appropriate to maintain the presence of relatively flat occlusal surfaces when undertaking restorative treatment or, in some cases, there may therefore be a need to ‘copy’ the existing occlusal prescription, which can be done by means of the use of a facebow record and a customized guidance table, as discussed further in part 3.
Analogously, the patient's intercondylar width may also influence the means by which posterior teeth make contact during lateral excursive movements. It is therefore important that the intercondylar width is determined when using a dental articulator to design restorations, which can be done by means of the use of facebow records, as discussed further in part 2.
The concept of the ‘ideal occlusion’
From an orthodontic perspective, the Angle's Class I relationship is often considered as being ‘normal.’ As part of this arrangement, the mesio-buccal cusp of the maxillary first molar occludes with the buccal groove of the mandibular first molar, with an overjet and overbite of 2 mm, respectively. However, from the restorative point of view, matters are somewhat more complex.
It is perhaps relevant at this stage to draw distinction between the concept of the ‘ideal occlusal scheme’ and that of a ‘correct occlusal scheme.’1 According Davies et al, an occlusal scheme may be described at three levels:14
In order to meet the criteria of the ideal occlusal scheme, there is the suggested need for the presence of a multitude of precise features that would be expected at each level so as to fulfil the overall mechanical and neuromuscular requirements. These features have been listed in Table 2. It should be noted, however, that much of the information contained in relation to this ideological concept is largely based on clinical opinion.
|
|
In contrast, an incorrect occlusal scheme could be considered to be one that, at the time of carrying out the examination, would be suggestive of the presence of occlusal dysfunction on the basis of the presenting clinical signs and symptoms. Such signs and symptoms may include:14
However, it is common to encounter patients who do not have any of the above signs or, indeed, the presence of an ideal occlusal scheme (Table 2), where it may be perhaps improper to diagnose the presence of an incorrect occlusal scheme. Under such circumstances, for instance where a patient may have signs of some degree of TW and the lack of an ideal occlusal scheme, caution needs to be exercised in diagnosing the presence of an erroneous occlusal scheme, and therefore the temptation to prescribe invasive treatment(s) as an attempt to attain the mechanical ideals.
From a pragmatic perspective, the concept of the mutually protected occlusal scheme (MPO)20 is often applied by many practitioners when considering restorative rehabilitation (assuming the absence of any crossbites, the presence of a full complement of teeth, the presence of an Angle's Class I occlusion and healthy periodontal/alveolar support)3 or, indeed, as a baseline to indicate mechanical stability. The existence of the MPO scheme implies:
Additional features that may be desirable of a functional occlusion include:
A canine-guided occlusion is relatively easier to accomplish from a technical/clinical perspective when undertaking restorative rehabilitation (as a means of providing lateral guidance) when compared with the scenario of mandibular guidance being provided by a number of posterior teeth on the working side (group function), especially when aiming to ensure that working aide and non-working side interferences on lateral excursion are duly avoided.22
Indeed, canine teeth (of good health, form and bone support) are suited to the role of absorbing occlusal forces, on the basis of:
However, it should be noted that there is no substantial evidence to support the notion of a canine-guided occlusion as being superior to any other form of occlusal scheme (such as that of group function).5 Furthermore, it would appear as if canine-guided occlusal schemes (as opposed to group function) only exist in about half of the population; with group function being more common amongst older patients (likely to be accounted for by the progressive wear of the canine teeth).13 It is neither uncommon to find the presence of canine guidance on one side of the patient's mouth and group function on the other or, indeed, the presence of group function at the start of the lateral excursive movement, followed by canine guidance at the end of the motion.2
It has, however, been suggested by Eliyas and Martin that, in relation to the management of a worn dentition of a dentate patient, a mutually protective occlusion or a canine-protected occlusion should be considered as an appropriate and desirable end point.22 The latter is of course based on the assumption that the canine tooth is suitable for this purpose. The manner by which the above features can be predictably incorporated into a patient's occlusal scheme when undertaking restorative rehabilitation of a severe and/or pathologically worn dentition will be discussed in part 3. Figures 16 and 17 show examples where, following tooth wear, the contact relationships have been influenced during excursion and the static relationship.

Conclusion
In part 1 of this series an attempt has been made to provide the definitions and description of the terminology that is often encountered when dealing with the subject of occlusion. Parts 2 and 3 will focus on the application of the principles and further elaboration of the clinical significance of the various components.

