References
Systemic sclerosis: a case report and considerations for general dental practitioners
From Volume 45, Issue 8, September 2018 | Pages 742-748
Article

Systemic sclerosis (SSc) is a rheumatic autoimmune, connective tissue disorder of excess collagen production, which can affect multiple organs, including the vascular, gastrointestinal, renal and musculoskeletal systems. The most prominent features include vasculopathy (fibrosis and disregulation of repair of blood vessels1), fibrosis of the skin and/or internal organs and specific autoantibodies production.2 The true pathogenesis is still unknown, however it has been attributed to genetic, environmental and immune-related factors. The immunological presence in SSc is usually found to involve auto-antibodies and activated lymphocytes, with increased levels of cytokines and growth factors detected.1
SSc tends to present in the 4th and 5th decade of life, with initial presenting symptoms including Raynaud's phenomenon and tightening of the skin. It is a rare condition, with prevalence 140.2 per million3, but it is of importance as this group of patients has a higher mortality and morbidity rate than healthy individuals, namely due to cardiac, renal and pulmonary complications.4,5
Systemic sclerosis can be divided into several sub-groups:
These patients are more likely to have renal and cardiac issues, therefore have a higher morbidity and mortality than the healthy population.
The following is a case report of a patient who was initially referred due to temporomandibular disorder (TMD) without taking into consideration her relevant medical history.
Case report
A 56-year-old female patient was referred to the Oral Surgery department by her GDP regarding suspected TMD, with pain on eating, speaking and on wakening in the morning, along with restricted mouth opening.
At her initial assessment, her presenting complaint was reduced mouth opening for over 18 months and, by forcing her own mouth open, she had experienced pain, which had persisted. She reported pain whilst eating and on wide mouth opening such as yawning. She stated that the pain was worse in the morning, gradually easing throughout the day. She described her jaw joint as ‘being stuck’ and the mouth opening had decreased with time. She was currently managing her symptoms with a soft diet.
In the medical history, she revealed a diagnosis of rheumatoid arthritis and hypothyroidism, and stated a multitude of medications, including prednisolone, methotrexate, folic acid, ibuprofen and lansoprazole. She made no mention of systemic sclerosis and did not indicate or complain about tightness of the skin. She was not aware of any lung or kidney issues. Her social history was recorded as a non-smoker and no alcohol intake.
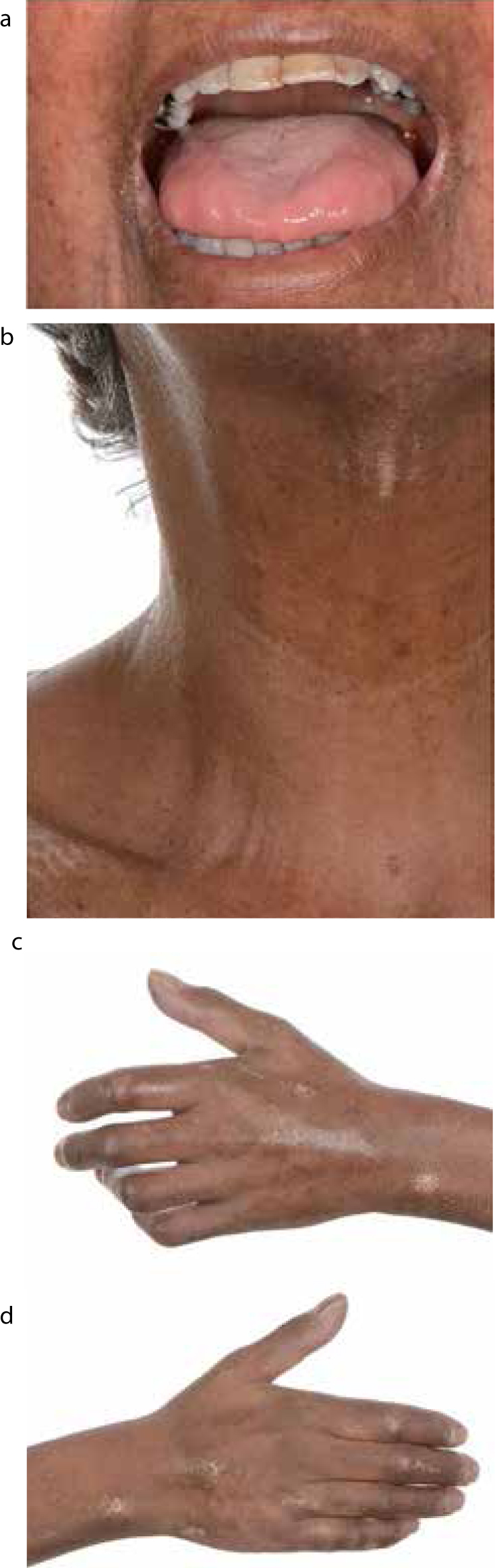
On clinical examination, using a ruler, she demonstrated inter-incisal opening of 20 mm, with no pain in the masticatory muscles on palpation. The patient pointed to the angle of her mouth as the area which had been causing her the most pain. The skin on her face was tight, creating mask-like facial features with reduced nasal ala aperture. Furthermore, her fingers were swollen and claw-like with the overlying skin tight and shiny, and evidence of calcinosis. It was also noticeable that she had increased pigmentation visible on the skin which was also a phenotypic feature of SSc. (Figure 1).
A request for medical history confirmation from her general medical practitioner was submitted, and she was referred for radiographic investigation. The orthopantomograph (Figure 2) was reported by the Oral and Maxillofacial Radiology consultant and was confirmed to demonstrate bony erosions affecting the condyle, ramus and angle of the mandible. These areas of erosion present as blunting of the bony anatomy, which is especially obvious at the angles. The report also stipulated generalized PDL widening, with the lamina dura still intact and moderate bone loss. This was a typical radiographic presentation of systemic sclerosis.7,8,9

The patient returned for review with medical history correspondence from the GMP, which confirmed systemic sclerosis diagnosis, with a positive blood test result for Scl-70 antibodies, and a record of presenting symptoms and signs of Raynaud's phenomenon, IBS and telangiectasia.
The patient was informed of the connection between her TMJ pain and restricted mouth opening to the systemic sclerosis diagnosis. She was reassured and instructed with conservative measures to manage her symptoms, such as soft diet, cutting food into small pieces before eating, analgesia as required orally and in the form of topical NSAIDs, and minimizing jaw movements by avoiding habits such as nail-biting and pen-chewing. She was referred onwards to our colleagues in the Public Dental Service for her routine dental care, periodontal therapy and education on jaw exercises.
Discussion
Systemic sclerosis tends to present later in life, and can progress rapidly, causing patients several health problems and limiting their quality of life and reducing life expectancy. The earliest sign of SSc is reported to be Raynaud's phenomenon – paroxysmal vasospasm, affecting mainly the hands and feet. Patients with this may suffer from colour change in the skin, usually turning white, blue, red or purple in cold environments or when in stressful situations. This can coincide with tightening of the skin and symptoms of pruritus. Patients may also complain of shortness of breath due to respiratory involvement. This should be urgently investigated to exclude other cardio-pulmonary causes.
The American College of Rheumatology/European League Against Rheumatism have produced a scoring system for the signs and symptoms to diagnose SSc definitively (Table 1). This allows specialists and generalists to classify the disease appropriately and therefore provide targeted treatment. At present, there is no current consensus on the definitive management of SSc, however treatment is usually targeted to involved organs and is dependent on the level of severity.
| Items | Sub-items | Weight/Score |
|---|---|---|
| Skin thickening of the fingers of both hands extending proximal to the metacarpophalangeal joints (MCPs) (sufficient criterion) | 9 | |
| Skin thickening of the fingers (only count the highest score) | Puffy fingers |
2 |
| Finger tip lesions (only count the highest score) | Digital tip ulcers |
2 |
| Telangiectasia | 2 | |
| Abnormal nailfold capillaries | 2 | |
| Pulmonary arterial hypertension (PAH) and/or interstitial lung disease (ILD)* (*Maximum score is 2) | PAH |
2 |
| Raynaud's phenomenon | 3 | |
| Scleroderma-related antibodies** (any of anti-centromere, anti-topoisomerase) (**Maximum score is 3) | Anti-centromere |
3 |
| [anti-Sd 70], anti-RNA polymerase III | Anti-RNA polymerase III | |
|
Total Score
|
||
For Raynaud's phenomenon, management requires lifestyle changes, such as warm clothing and avoiding cold temperatures. Use of vasodilators, such as calcium channel blockers (eg amlodipine, nifedipine, diltiazem, verapamil), may be indicated. In severe cases, where ulceration and gangrene has occurred, surgery and amputation may be required.
Management of gastric reflux is usually in the form of proton pump inhibitors, such as omeprazole, lansoprazole and other symptoms of gastrointestinal involvement, for example, constipation would be alleviated with laxatives.
Pulmonary hypertension may require diuretic therapy, reducing the amount of fluid in the body and therefore reducing the blood pressure within vessels. Patients can also be anti-coagulated to reduce the burden on the pulmonary system and prevent thrombosis. These patients are also treated with digoxin to manage heart failure, which can be right- and left-sided.
Immunotherapy/immunosuppression using agents such as methotrexate, azathioprine and rituximab can be used to manage active skin involvement, pulmonary fibrosis, cardiac sclerosis and renal crisis.10 These drugs can modulate the immune response, sometimes reducing the release of immune cells or cytokines, which can invoke more damage.
Oral manifestations of SSc often present with tightening of the skin on the face, restricting the mouth opening, causing microstomia. This can result in difficulties of accessing the mouth for dental treatment, especially when prosthetic measures are required. Therefore, it is of utmost importance for dentists to initiate a programme of dental prevention to avoid the need for intervention. A suitable regimen should include regular hygiene phase therapy, applications of topical fluoride varnish and prescribing high fluoride toothpaste, eg 2800 ppm or 5000 ppm. Diet advice which aims to reduce sugar intake and prevent acid erosion is also important.
The presence of autoimmune disease also introduces the complicating factor of xerostomia caused by fibrosis of the salivary glands, and this gives further strength to the preventive dentistry approach. Systemic sclerosis also presents with gastric reflux due to oesophageal dysmotility, which can cause dental erosion and, in some cases, oral ulceration. Again, it would be recommended for the patient to be placed on a high fluoride strength regimen to minimize the effects of these symptoms.
Patients with SSc have an increased prevalence of periodontitis, which may be attributed to poor oral hygiene due to reduced access, xerostomia, immunosuppressive drugs,11 which lead to alteration in the immune response and reduced capillary blood flow.12 Dentists should ensure that patients receive regular hygiene phase therapy and recall patients to monitor the periodontal condition closely.
On intra-oral radiographs, GDPs may notice widening of the PDL surrounding teeth. Those who have access to orthopantomography can witness bilateral erosion of the condyle, coronoid, ramus and angle of the mandible, although this has been reported to be a relatively uncommon sign.9 Some authors have cited that the erosions may be attributed to the pressures applied to the bone through fibrosis and atrophy of the masticatory muscles and skin. The effects of these mandibular erosions, in conjunction with tightness of the skin, can result in temporomandibular joint dysfunction13 symptoms, such as pain on function and restricted mouth opening. In the first instance, the patient should be educated on the relation of SSc to their TMJD, to allow them to realize that this will be a life-long symptom and unlikely to resolve. The patient should be informed of conservative management strategies, such as soft diet, analgesia and gentle jaw exercises, to ease mouth opening discomfort.14 In terms of more invasive management, there have been reports of successful use of temporomandibular joint replacements using custom-made prosthesis15 and autogenous grafts.16 However, this is not mainstream treatment for mandibular erosions in systemic sclerosis.
The erosion of the mandible can also give rise to pathological fractures17,18 and the patient may complain of malocclusion development and paraesthesia. This would need a referral to secondary care for management for further treatment, for example fixation of the fracture.
Considerations for the GDP
This case report demonstrates the importance of a thorough medical history, which would provide hints as to the cause of the reduced mouth opening. The case also indicates that educating patients on their condition would help them understand the symptoms they suffer and allow practitioners who do not have direct access to patient medical records to correlate their oral findings to the medical background. The GDP can liaise with the medical practitioner or rheumatology specialists to confirm the medical history. This will allow GDPs to provide tailored dental care and it is important in terms of medico-legal protection as the GDP has undertaken appropriate histories and liaised with other professionals to provide appropriate and effective care.
As discussed, the dental management of these patients should be focused on prevention using hygiene phase therapy, such as supra- and sub-gingival scaling every 4 months, together with oral hygiene instruction and a high fluoride regimen (topical fluoride varnish 22500 ppm, toothpaste 5000 ppm) to reduce the progression of periodontitis and to prevent caries. In relation to prosthetic replacement, there are several papers which have looked at methods of replacing teeth,19,20,21,22 including removable prosthesis, implant-supported rehabilitation and fixed restorations. It is evident that restoration of the dentition should be adapted to the patient's requirements and whether access will permit.
Conclusion
Although rare, systemic sclerosis can present to the GDP in the early stages of development and it is advantageous to be aware of the warning signs. In patients with already diagnosed SSc, the dentist is an integral part of the management team and should be able to prevent or reduce the progression of intra-oral disease through preventive treatment plans and regular recall.

