References
Immediate dentures part 2: denture construction
From Volume 45, Issue 8, September 2018 | Pages 720-726
Article
In the first part, the advantages and disadvantages of immediate dentures were discussed, followed by a discussion around assessment and treatment planning for immediate dentures. This section will focus on the various stages of immediate denture construction. Immediate removable prostheses are usually fitted on the day that teeth are extracted, unlike conventional dentures which replace teeth historically lost to dental disease. For this reason, some stages of denture fabrication may not be undertaken. Each case is different and has to be assessed individually as certain factors may alleviate the need for every single denture construction stage. Sufficient information must be provided to the technician in order to fabricate an optimal and predictable prosthesis for the patient. As always, good communication between the clinician and technician is necessary in order to ensure a predictable result.
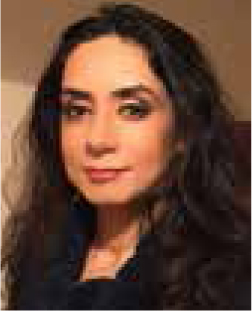
Several factors can impact on an immediate denture construction, such as multiple teeth requiring extractions. This increases the challenge and unpredictability of the final prosthesis, particularly where teeth in the opposing arch are being extracted, leading to a change in the occlusal vertical dimension (OVD). Clinicians need to be aware of this limitation, as do patients. Additionally, certain denture stages, such as jaw registration and wax try-in, may not be required or even possible if patients have retained their natural teeth and are having extractions for the first time. In situations where there are spaces due to missing teeth, these can be utilized to carry out the stages as normal (Figure 1). Where occlusal re-organization has been planned, one can anticipate greater difficulty in fitting the final prosthesis, especially in situations where it has not been possible to carry out the jaw registration stage. For example, when multiple teeth are extracted from opposing arches causing loss of stable occlusal contacts. Periodontally involved teeth which are mobile can cause problems, particularly when taking impressions. These may require additional care in order to prevent iatrogenic removal, for example, by splinting to adjacent teeth.
While the situations mentioned above may impact upon the stages of immediate denture construction, and some cases may not require every clinical and laboratory stage to be carried out, in most situations the majority of the denture construction stages will be followed. This is indeed preferable as it can lead to a more predictable outcome.
Impression taking
Primary impression
Primary impressions for removable prostheses are taken in order to capture an overall picture which involves comprehensive recording of all teeth and denture-bearing areas.1 The main aim for primary impressions is to produce adequately fitting special trays, however, they can also be used for diagnostic purposes as well as to aid in denture design.
These are usually undertaken in stock trays which may need to be adjusted by trimming in over-extended areas or adding green stick compound in those places where it is deficient. After correcting the tray extensions, it is useful to assess the amount of space between the tray and tissues. If this space is considered to be excessive, an intermediate material can be placed to compensate for it, such as impression compound or silicone putty. Once the clinician is satisfied with the tray, the primary impression can be taken. A variety of materials can be used, including alginate, impression compound, addition or condensation silicones or polyethers. Selection will be based on various factors, including the number of teeth and degree of undercut present.2
An appropriate special tray can then be prescribed to the technician, based on the impression technique and material that will be utilized in the master impression.
Master impression
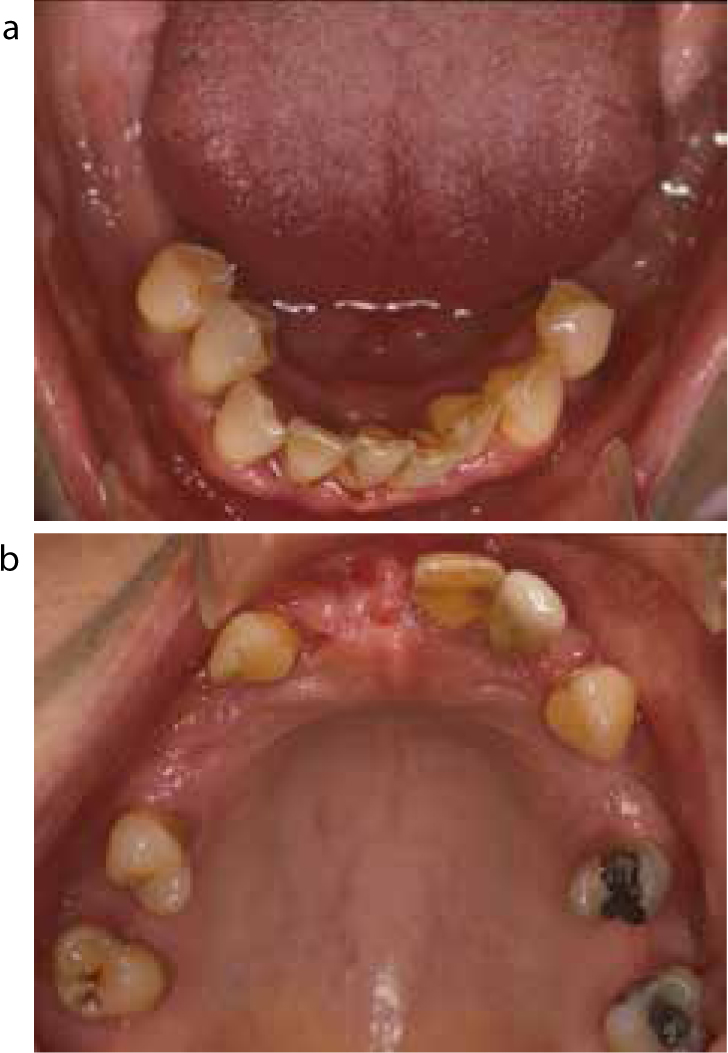
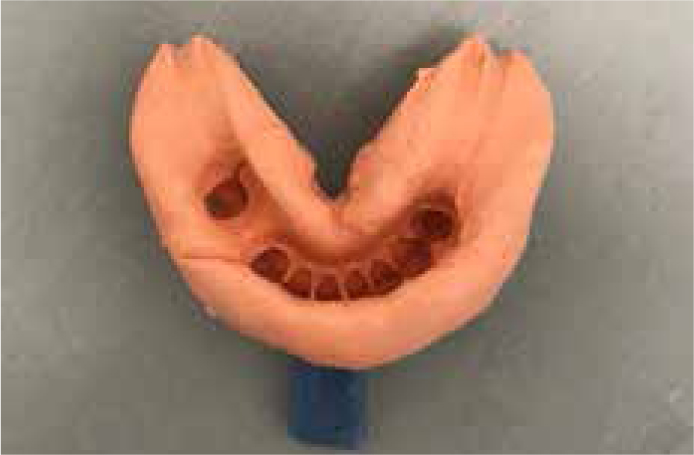
The aim of a master impression is to record contours of the teeth present, the remainder of the arch and the functional depth and width of all the areas of the oral cavity accurately. A special tray fabricated in the laboratory is used for this purpose. (Figure 2). The tray should be checked on both the cast and in the mouth to assess its adequacy and any overextension or deficiency corrected (as mentioned before) prior to the master impression being taken. Molding may be indicated for the intended saddle areas with green stick tracing compound to determine the functional width and depth of the buccal and lingual sulci prior to the master impression being taken.1 The reproduction of the remaining dentition is obtained by capturing the coronal and occlusal aspects of the remaining teeth accurately, including any prepared surfaces.1 Stabilizing primary disease along with a thorough scale and polish will ensure such an outcome.
A variety of commonly used materials include alginate, addition or condensation silicones or polyethers. The authors advise the choice of impression material to be made on a case by case basis, taking into account various factors such as number of remaining teeth present, any undercuts present, extent of alveolar ridge resorption, etc.
Challenges with taking impressions
When taking impressions for immediate dentures there is a risk, particularly when there are periodontally involved teeth, cavitated carious lesions or bridge work, that the impression material can engage the undercut around these teeth and/or fixed prosthesis. This can lead to potential iatrogenic removal upon withdrawal of the impression. There are a number of techniques that can be used to minimize this which include:

Jaw registration
The jaw registration procedure may vary depending on whether it is decided to conform to the patient's current OVD or to re-organize the occlusion. In general, conforming to the current OVD is less clinically and technically demanding, is more predictable, and tends to be better tolerated by the patient in general.
In situations where the OVD is to be maintained and patients retain most of their natural teeth with multiple stable contacts which are easily located, jaw registration can be taken using an appropriate bite registration material. However, where multiple teeth are missing and the OVD is planned for re-organization, it is necessary to use wax record blocks that are well fitted and adapted nicely to the underlying edentulous saddle. This will ensure that no movement or distortion of the rim occurs during the jaw registration.2 If needed, stability can be enhanced by fixing wire clasps to the wax bases in order to engage the remaining standing teeth.4 The wax rim is then reduced and shaped to determine the proposed occlusal plane and OVD. The registration is taken with the patient manipulated into the retruded arc of closure at the proposed OVD. This may be challenging, particularly as there may often be no tooth to tooth contact present. A bite registration material is then used for the final registration so that the technician is able to articulate the study casts without any movement or rocking of the casts.
The proposed aesthetics should be assessed in the form of the tooth size, shape, set-up and shade. An advantage of teeth being present is that one can assess if the patient is keen to maintain the appearance. This can serve as a guide, otherwise the selection is done in the same way as it is for conventional dentures. The setting up of the teeth should closely mimic the position occupied by their natural predecessors. However, there will be situations where replicating the natural appearance may not be desirable due to malocclusion or mal-alignment (Figure 4). Such patients may benefit from altering tooth position, size and shape. This decision is made jointly with the patient and prescribed to the technician.

Wax try-in/trial
A wax try-in of the prosthesis should be carried out where possible. This may not be possible in all cases due to the fact that the teeth have not been extracted and, in such situations, the patient should be shown the waxed-up prosthesis on the articulated casts to give an idea of what the final result is likely to be. This should be approved prior to construction.2
Where a wax try-in is possible, this should be fitted and assessed in the same way as a conventional denture. Any clinical, technical or aesthetic issues should be addressed prior to construction of the prosthesis. Where changes are required, these should be carried out and the wax try-in re-tried. Once the clinician and patient are both happy, the denture can then be prescribed for construction.
Extraction of teeth and immediate denture fit
Prior to extraction of any teeth, the prosthesis should be present and checked to ensure that it is as prescribed and will replace those teeth that are planned for extraction. A large part of the success attributed to immediate dentures lies with a good extraction technique.2 The extractions should be carried out as atraumatically as possible, preserving as much bone as possible, particularly the buccal and lingual plate so that bone loss and subsequent resorption is minimized (Figure 5). However, this is not always possible. In the past, there was a tendency to carry out alveolotomy and alveolectomy procedures in order to remove any undercuts in the labial sulcus.5,6 However, these procedures are rarely favoured today due to their destructive nature, and the onus is now on fabricating a denture that overcomes this issue.7 These procedures can also create challenges in the long term as treatment options can become limited. For example, implant placement may be difficult due to limited bone being available at the surgical site.


Once the teeth are removed, the denture should be tried in and checked that it sits in the correct position properly. Any interference from teeth as well as gross overextensions should be corrected. The denture should be checked for retention, support and stability. The occlusion should be checked both in a static and dynamic relationship and any interference corrected. Where there are no stable occlusal contacts, this will normally be in the retruded contact position. Since a large part of fabrication of an immediate denture involves guesswork to ascertain the level of alveolar ridge after extraction, it is likely that the denture may require significant adjustment prior to fit. Therefore, it is important to book sufficient time on the day of surgery in order to provide the patient with a comfortable, well-fitting denture prior to the patient leaving the surgery, otherwise the patient is less likely to wear the prosthesis. This can be challenging as the patient is ‘numb’ from the local anaesthetic used for the extractions, therefore the patient should be subsequently reviewed soon after, to re-assess the prosthesis. Patients may also be anxious and emotionally drained after the procedure, therefore, offering them extra support from the entire team will help them significantly as patients often appreciate care and attention at this critical stage. Providing them with written leaflets on post-operative instructions is useful as they may not be able to recall information correctly, especially if the extractions have been carried out under conscious sedation.
Post-operative instruction and review
It is recommended that patients should be advised to keep the dentures in the mouth for the first 24 hours.8,9 This is so that the soft tissue oedema does not prevent the denture from seating well. After that, the denture should be worn during the day and removed and stored correctly at night whilst the patient sleeps.
While there are no specific guidelines regarding the recall period, it would be sensible to review the patient 24 hours after the extraction to reassess the prosthesis and carry out adjustments as appropriate. After this the patient can be reviewed at one week and then one month. However, this needs to be determined on a case by case basis as various factors will influence the decision, including the number of extractions, fit of the prosthesis, patient compliance, etc. Once reviewed, adjustments may be carried out as appropriate. Resorption and bony remodelling will occur over time, which is likely to affect the retention and stability of the prosthesis and a reline often becomes necessary. This is particularly common and occurs sooner where multiple teeth have been extracted or where extractions were traumatic. Relines can be required as early as 4–6 weeks10 and can be carried out either chairside or in the laboratory. After 3–6 months post-extraction, the denture may loosen further and require rebasing or fabrication of a new prosthesis.10 Where possible, this should be delayed until the clinician feels that further bone resorption is unlikely to occur, otherwise this rebased or new prosthesis will quickly suffer the same fate. However, there may be certain situations where a reline or re-base would not be feasible for an immediate denture and a new denture may need to be made quite early, for example, where a large amount of early bone resorption may cause significant loss of retention. In such cases, a new denture can serve as a transitional/interim denture till bony remodelling is complete, at which stage a new permanent conventional removable prosthesis can be fabricated.
Some of the common problems with immediate dentures over time include compromised aesthetics and poor retention. Aesthetics is of particular concern in the anterior region where a gap may start to show between the alveolar ridge and the denture, especially when an open faced or partial flange has been used. For this reason it is prudent to review such patients in order to identify these issues regularly.
Addition to immediate dentures
It may become necessary to add teeth to the existing immediate dentures as and when subseqent teeth are lost due to various factors. The ability to add teeth to a prosthesis is dependent on the design of the prosthesis and the material used. Where possible, dentures should be designed to accommodate additions where teeth have a guarded or poor prognosis, as this will make addition to the prosthesis relatively straightforward.
The addition of teeth to acrylic immediate dentures can be carried out in the laboratory or chairside. For laboratory addition, an impression is taken of the arch with the immediate denture in situ and sent to the laboratory prior to extraction. The lab then casts the impression and adds the tooth/teeth to the prosthesis. This is then returned, the tooth/teeth extracted and the prosthesis fitted. The disadvantage of using this technique is that the patient is without the prosthesis for a period whilst this is carried out but, if it is planned in advance and arranged with the lab, then it can often be carried out within a few hours. The advantage with such a repair is that it saves chair time and the materials that can be used in the laboratory are often superior in quality to the ones that can be utilized within the dental surgery.
A chairside technique described in the literature can circumvent the issue of the patient being without the prosthesis.11 In this case, an impression is taken of the mouth with the denture in situ, the impression is then cast and the tooth/teeth planned for extraction are removed from it. The tooth/teeth are then extracted. Acrylic denture tooth/teeth are placed onto the cast where the missing teeth are and wax used to secure the acrylic teeth to the denture. This is then tried in the mouth for position, colour and shape. Any readjustments required are carried out. The denture is placed back on the cast and a putty index is made to record the position of the acrylic tooth in the arch. The modelling wax is then removed and vaseline applied onto the study cast. Using the putty index, the tooth is placed in position and fixed to the denture using auto-polymerizing acrylic resin. Once set, the denture is tried in the patient's mouth for any final adjustments.11 The advantage of this technique is that the patient does not have to be without his/her denture. However, this process takes time clinically and there is a need to have the ability to cast impressions within the practice, which may not always be possible.
Conclusion
Immediate dentures form a significant part of prosthetic dentistry and continue to provide patients with replacement of their natural teeth in the post-extraction period. They not only allow maintenance of appearance and function, but also help to prepare patients psychologically for the edentulous phase of their life. With the use of correct techniques, immediate dentures can be quite retentive and stable in the interim period and provide a rewarding experience both for the clinician as well as the patient.

