References
3D printed tooth model – a patient education tool and surgical aid in endodontics
From Volume 45, Issue 7, July 2018 | Pages 655-659
Article

The advantages of CBCT are well known in all fields of dentistry. It provides advantages above the conventional 2-Dimensional (2D) imaging in terms of diagnosis, treatment planning and improving the predictability of the procedure.1 Today, conversion of virtual images to materiality has been made possible by 3-Dimensional (3D) printing. 3D printing has opened up a whole new world of diagnosis, anatomical structure evaluation, treatment planning and patient education in the field of dentistry.2 The technique of 3D printing can be used as an effective motivational and educational tool, quite apart from its other advantages,3 and act as a visual aid to patients in the acceptance of treatment. The case below explains how a patient, unwilling for the use of surgical intervention, was motivated to accept the treatment modality using 3D printed models generated from CBCT data.
Case report and technique
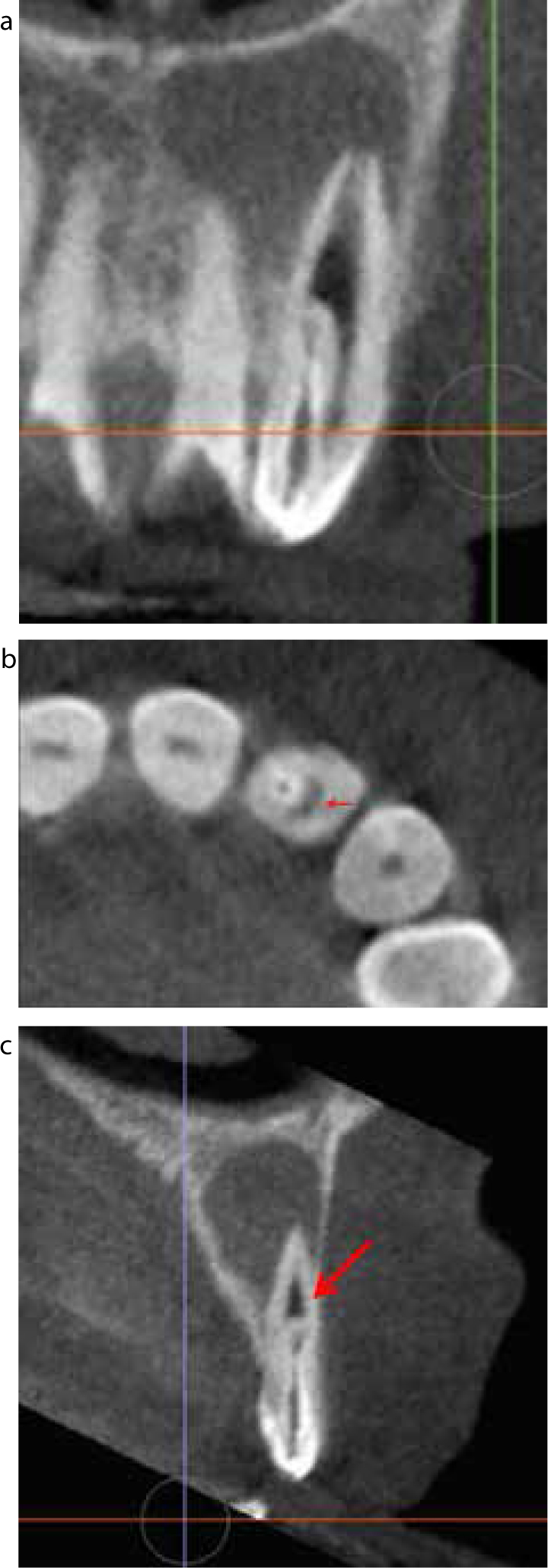
A 37-year-old male patient was referred from a private practice complaining of pain in the upper left side anterior region of his mouth for a few days. There was history of pus discharge from that region, but no history of trauma. Medical history was non contributory. On examination, UL2 exhibited a developmental depression on the palatal surface and elicited tenderness to percussion (Figure 1). Pulp sensibility tests were negative for UL2 and positive for UL1 and UL3. An intra-oral periapical radiograph from the referring dentist revealed infolding of the radio-opaque structure within the crown of UL2 extending up to the cervical third of the root. A large periradicular radiolucency was also seen surrounding the root of the tooth (Figure 2). The pre-operative IOPA suffered from artefacts but it was deemed necessary to obtain CBCT images for proper treatment planning and hence another IOPA was not taken at that time. CBCT images revealed the anatomy of the tooth. The invagination was extending to the middle third of the root (Figure 3a). The main canal exhibited C-shaped anatomy up to the level of invagination (Figure 3b) followed by a broad canal, part of which was obscured beneath the invagination (Figure 3c). There was no obvious connection between the invagination and the main canal and the coronal opening of the invagination was situated on the incisal edge. Based on clinical findings and investigations, a diagnosis of chronic apical periodontitis and dens invaginatus type 3A with respect to UL2 was reached. Based on the anatomical considerations, it was decided to treat the invagination by orthograde endodontics and the main canal using a retrogade technique. Surgical treatment was planned for the patient but the patient was unwilling to undertake surgical treatment, even after one session of counselling. Following this it was planned to motivate the patient using a 3D printed model, assuming that it would be easy for him to comprehend the anatomy of the tooth and therefore accept the treatment plan. Two models were printed using the data acquired from CBCT: one enlarged model (Figure 4a) for patient education and one original sized model (Figure 4b) for surgical treatment planning. The models were printed using ‘Make 3D’ Pratham 3.0 model (Figure 4c). It is based on FDM (Fused Deposit Manufacturing) technology using an ABS (Acrylonitrile butadiene styrene) filament of 1.75 mm diameter with a 4.0 nozzle having two extruders and a large build size.


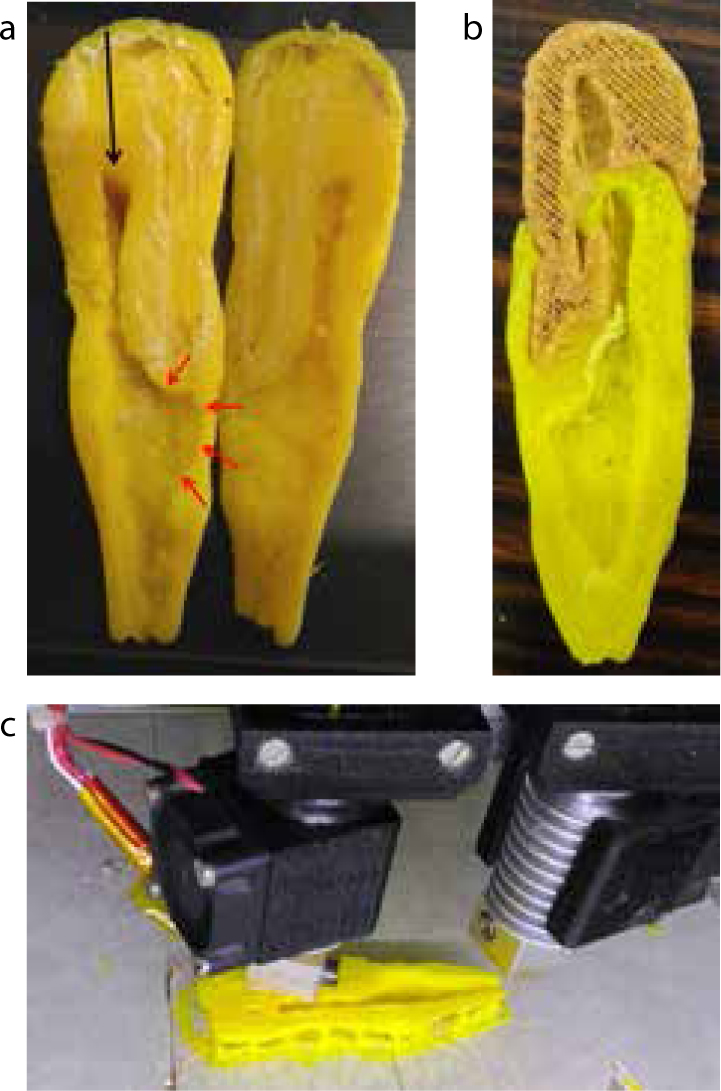
Using these models, the patient was educated regarding the areas which were inaccessible from the conventional approach (Figure 4a) and how the surgical approach would provide convenience and better results. Following the counselling session, there was a remarkable change in the patient's attitude and consent for the surgical treatment was achieved. The model also helped in evaluating and understanding the angulation of the instrument which would be required to retrofill MTA. Following this the treatment was implemented:
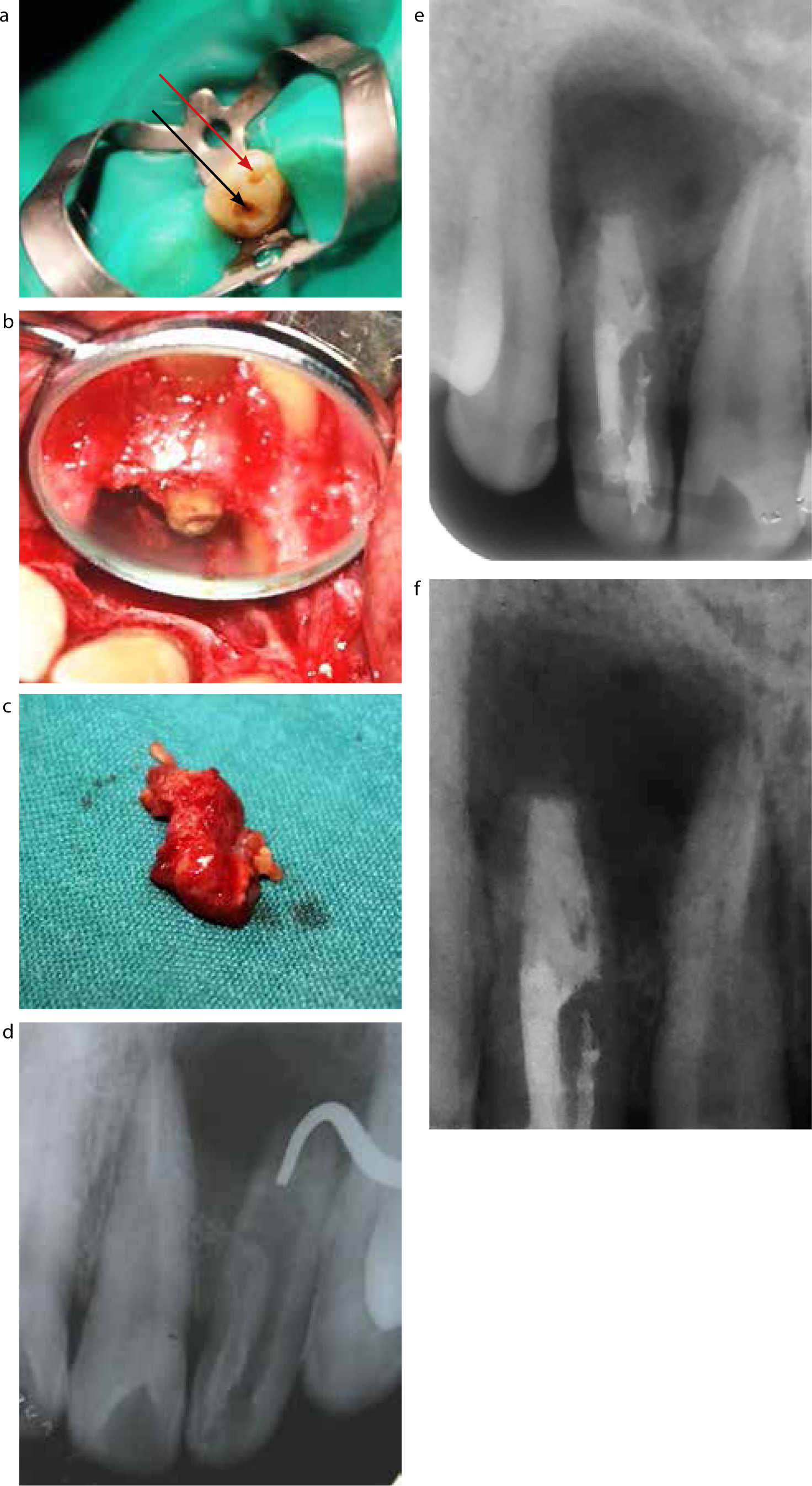
A six-month follow-up radiograph revealed continued healing of the tooth (Figure 5f).
Discussion
Healing of a chronic apical periodontitis is dependent on complete disinfection of root canals. In the above case, surgical treatment was warranted because a major portion of the main canal was hidden beneath the invagination.4,5 Cleaning and shaping of such anatomy with an orthograde approach may lead to incomplete disinfection and obturation.6,7
CBCT has unveiled the potential of 3D imaging in dentistry as an aid to improved diagnosis and treatment planning. An anomalous tooth like dens invaginatus can be a perplexing problem to the dentist because of the challenging anatomy. 3D imaging may be employed in the execution of the treatment plan. In the above case, the mapping of the anatomy of dens invaginatus and the main canal allowed precise and separate access openings for them. The C-shaped anatomy of the main canal detected using the scan allowed for the modification of the biomechanical preparation technique to conventional circumferential filing rather than the use of a rotary system. However, digital images have their own limitation when it comes to patient education. 3D printed models may be used to bridge that gap efficiently and complement digital images, as seen in the above case.
A patient's acceptance of treatment not only allows the execution of plans most suitable for the patient, but also limits the anxiety level of that patient, which is important during surgical treatment. A motivated and calm patient is a better contender for surgical treatment compared to an anxious patient, who may suffer from tremors, sweating and other symptoms during surgery.8 In this way, 3D printed models can directly influence the patient motivation levels and indirectly help in keeping the patient calm during the procedure.
3D printed models are accurate to the actual anatomical dimensions and are being increasingly used in dentistry for surgical and implant treatment planning.9 The use of 3D printed models have been reported recently for tissue retraction during surgery, which improved the soft tissue handling10 and also to gain access into the root canal while treating anomalous or normal teeth.11,12 3D printing can be utilized for patient education, treatment planning or during therapeutics for a single case. In the present case, the primary objective was to educate the patient regarding the anatomy of the tooth and the requirement of surgery. Guided access using a 3D template was also a possibility, but it would have resulted in excessive loss of coronal tooth structure, as a major part of the main canal was hidden beneath the invagination. Therefore, a larger sized model was deemed necessary for patient education. A second model, accurate to dimensions, was printed to allow customization of a plugger in terms of length and angle which was to be used for retrofilling of MTA. This case highlights the way this technique can be incorporated in the field of endodontics for patient education and treatment planning while dealing with complex anatomy
Conclusion
3D printed models can prove to be a useful tool in dealing with anxious or non-cooperative patients who require surgical endodontic therapy.

