References
A contemporary approach for the management of generalized tooth wear
From Volume 45, Issue 6, June 2018 | Pages 569-577
Article

Section 1. Pre-treatment assessment
Patient details
Initial referral
Patient complaints
History of presenting complaint
Relevant medical history
Past dental history
Social history
Clinical examination: extra-oral features (Figure 1)

Smile assessment
Clinical examination: intra-oral features
Periodontal status
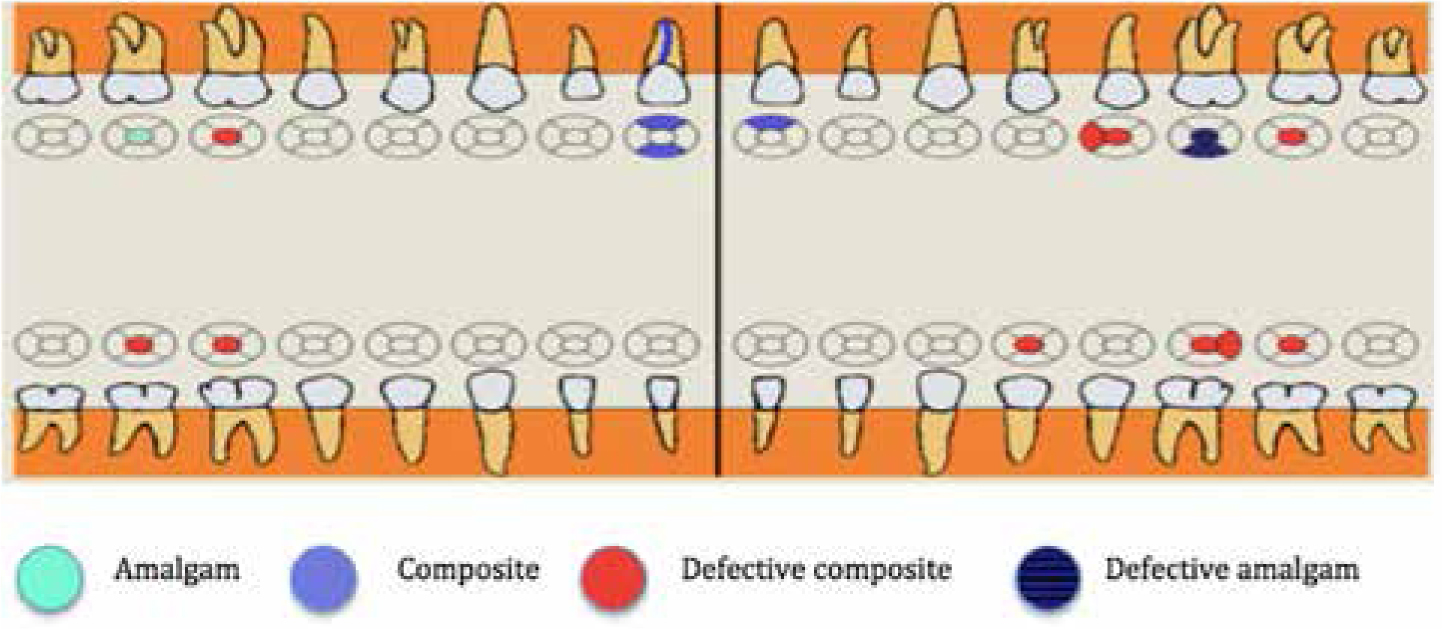
Charted teeth present (Figure 2) General dental findings
Occlusal features
Static occlusion
Dynamic occlusion


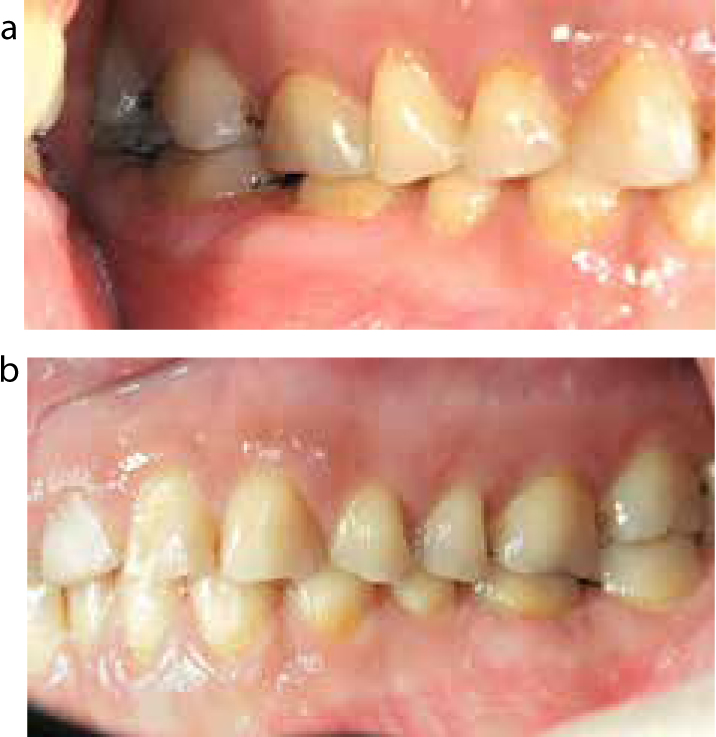
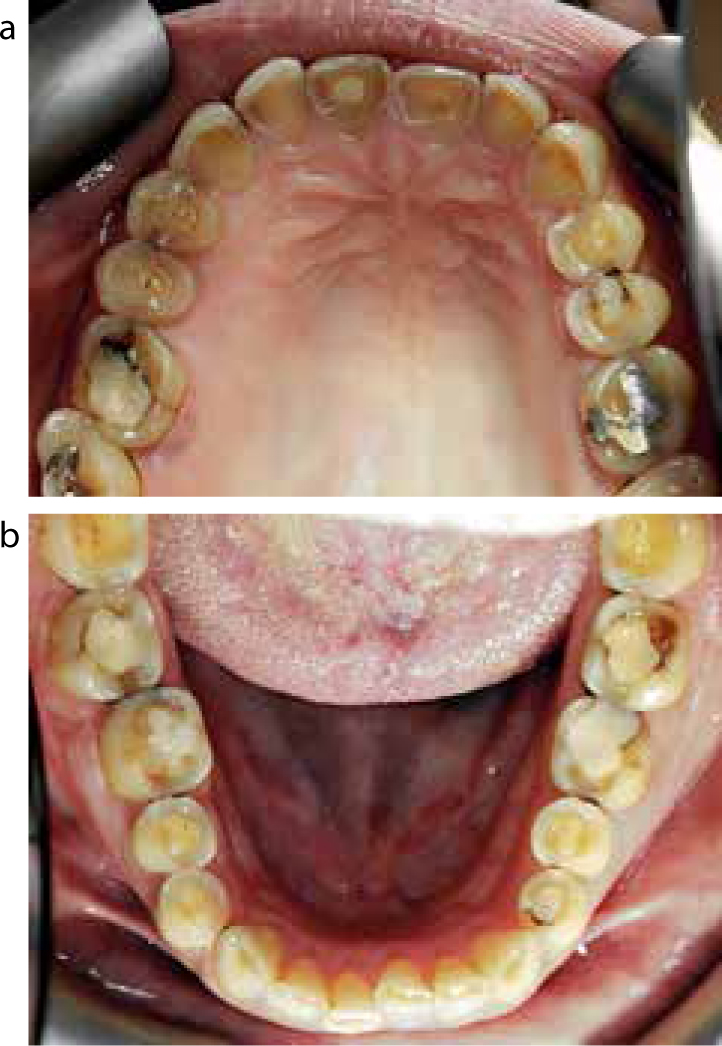
Pre-treatment views – intra-oral (Figures 5–7) Other special investigations

Sensitivity tests: All teeth excluding (UR1) tested positive to Endo-lce and electrical pulp testing.
Percussion test: None of the teeth was tender to percussion.
Pre-treatment radiographic examination (Figure 8)
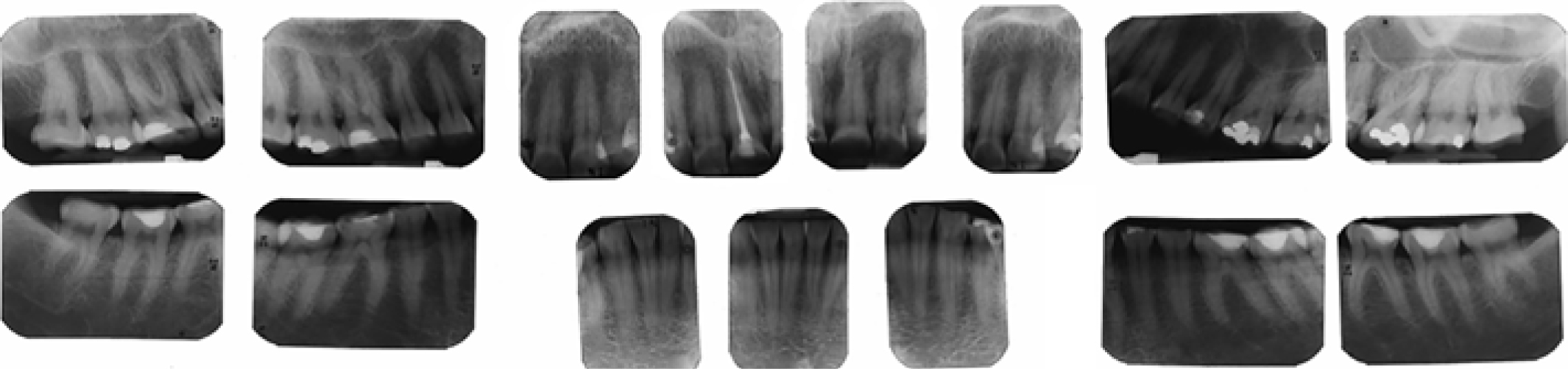
Relevant radiographic observations
Root fillings
Diagnosis
Aims and objectives of treatment
Treatment plan
1. Immediate
2. Transitional
3. Reconstruction
4. Maintenance
Section 2. Treatment
Key stages in treatment progress
Immediate phase
Transitional phase




Reconstruction phase
The maxillary anterior teeth (UR3 to UL3) were restored with a combination of indirect palatal composite resin veneers and direct labial composite resin build-up restorations (Figure 12). The mandibular anterior teeth (LR3 to LL3) were restored with direct composite resin with the aid of a clear silicone index (based on the diagnostic wax-up) (Figures 16-20).





Following restoration of the anterior dentition, the posteriors were stabilized with resin-modified glass ionomer occlusal stops (Figure 21).

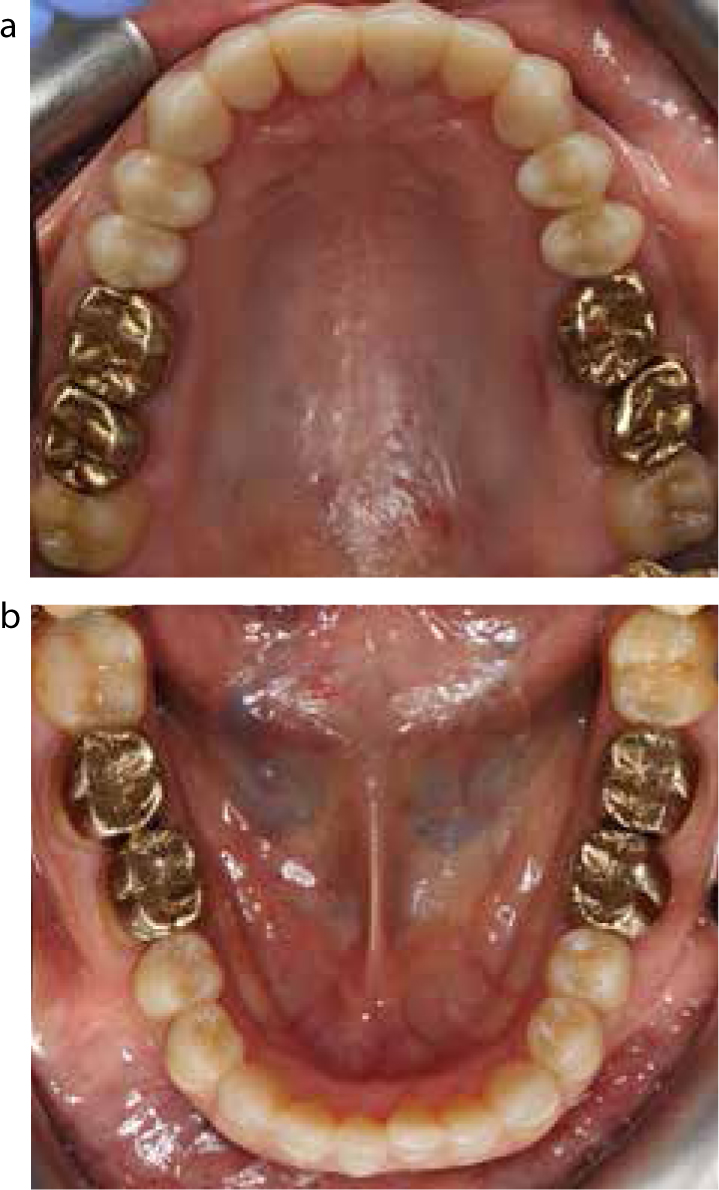
An impression was taken and wax-up was completed to proceed with the posterior reconstruction. All 1st and 2nd molars were restored to the established OVD with adhesive gold onlays (Figure 22).

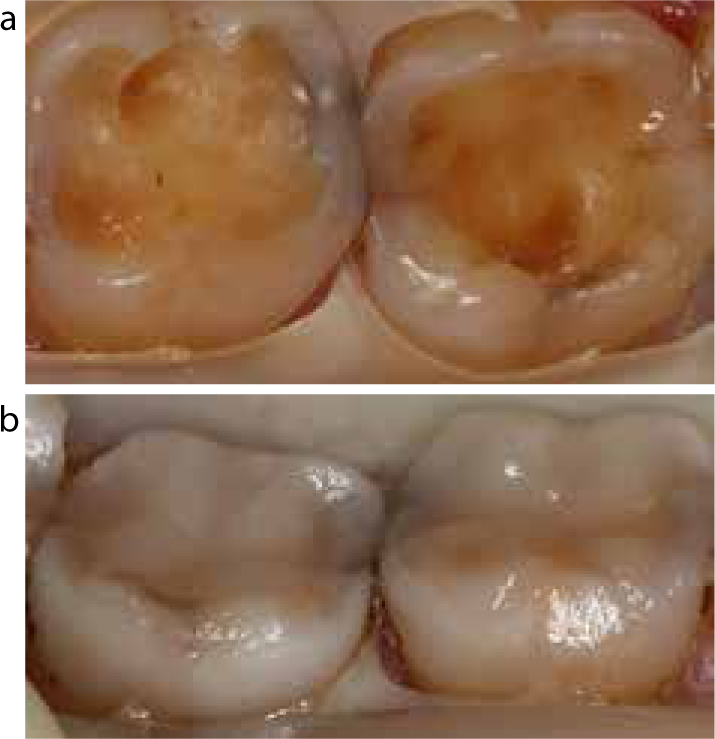
Following the completion of 1st and 2nd molars, definitive restorations, all premolars (Figure 23) and third molars were restored directly with composite resin with the aid of a clear silicone index of the diagnostic wax-up.

Maintenance
Post-treatment a maxillary hard occlusal splint was fitted (Figure 24). The patient was then on supportive periodontal therapy and review with her GDP.

Post-treatment views (Figures 25–29)




Discussion
The patient presented with tooth wear affecting her anterior and posterior dentition. The tooth wear was moderate to severe and had affected the buccal and palatal surfaces of the anterior dentition and the occlusal surfaces of the posterior dentition. The patient was concerned with the appearance of her front teeth, gummy smile and the wear of her posterior teeth. She had suffered from acid reflux for some years and was treated medically by proton pump inhibitors.
The objectives were to highlight and assist the patient in reducing the cariogenic/erosive dietary intake and optimize oral hygiene level. The aim was to restore the patient's dentition to a stable and functionally comfortable occlusion with a pleasing appearance. Informed consent was given by the patient to the proposed treatment.
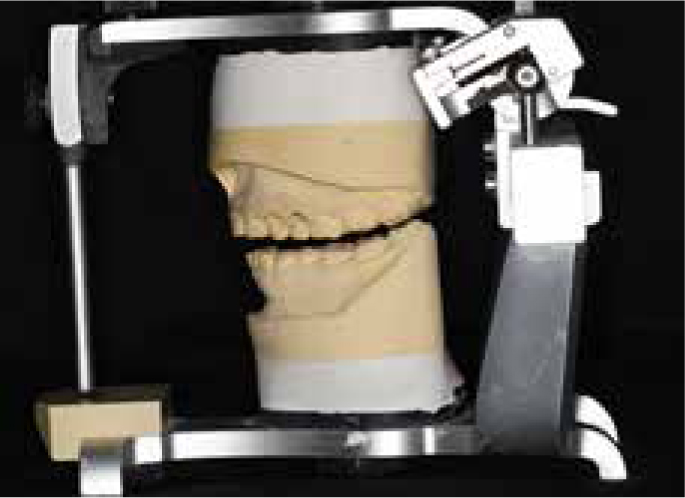
The generalized tooth wear seems to have been accompanied by dento-alveolar compensation. As a result of this, there was insufficient interocclusal space for restoring the worn down dentition. The lack of space anteriorly and the need for multiple posterior teeth restorations dictated that the case used a reorganized approach working in the retruded axis position (RAP) at an increased occlusal vertical dimension. A pre-operative hard maxillary occlusal splint was fabricated to assess the new planned occlusal vertical dimension and to achieve muscle relaxation to allow reproducible closing at retruded axis position. Jaw registration was carried out in RAP at increased vertical occlusal dimension post splint therapy. The working occlusal vertical dimension was established from the diagnostic wax-up and a mock try-in. In addition, a mock try-in was aimed to assess the aesthetics prior to crown lengthening surgery and phonetics.
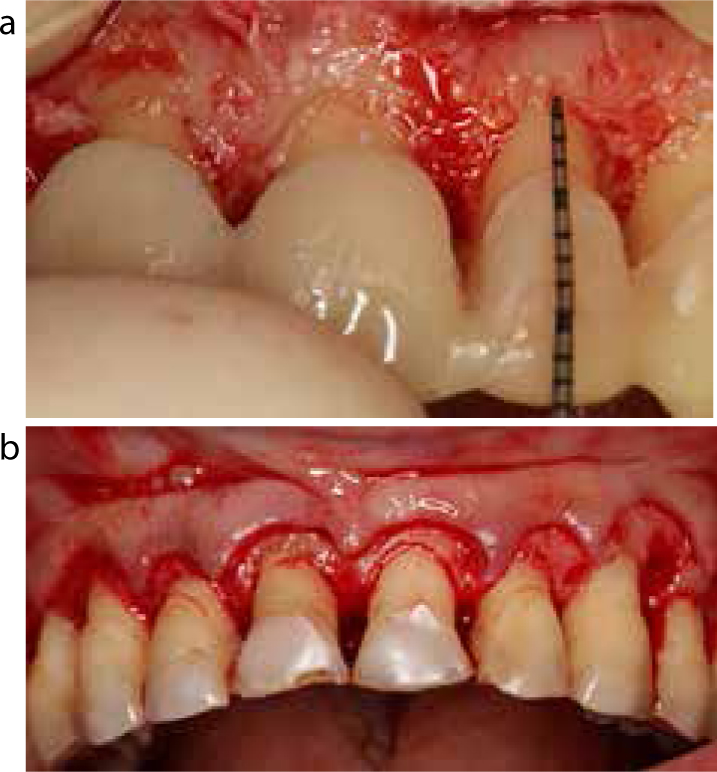
A crown lengthening procedure, including resective osseous surgery, was completed in order both to improve the gingival contour as well as gain sufficient coronal tooth structure for the build-up of the composite resin restorations. The surgery was guided by an acrylic stent fabricated from the diagnostic wax-up. A period of six months after surgery was allowed for the stability of the gingival margin prior to composite resin restoration.2
The patient was treated in a conservative manner with predictable restorations in order to enhance both her oral function and aesthetics. A rim of enamel was present around the margins of all teeth, thereby improving the predictability of the bonding of the resin-based material to the tooth structure. The anterior teeth were restored with composite resin restorations, which are based on good survival time and provide a non-destructive option.4
The posterior dentition was minimally prepared for restoration with adhesive cast gold onlays, which have been considered to have 89% survival probability at 60 months.3 Following the definitive phase of treatment the patient was given a post-operative occlusal maxillary splint to protect the restorations.
A good prognosis can be expected if the oral hygiene level is kept optimal. The patient was advised of the necessity for a regular need for composite resin polish, repair and occasional replacement. At the conclusion of the treatment the patient was very pleased with the appearance and functionally comfortable.

