References
Essentials of light curing
From Volume 45, Issue 5, May 2018 | Pages 400-406
Article

Every day, dentists use their curing lights when making resin-based composite (RBC) restorations, curing sealants, bonding brackets to teeth or cementing all-ceramic restorations. Unfortunately, light curing is seldom given the attention it deserves, as evidenced by technique articles on how to deliver successful resin-based composite restorations.1 Recent surveys have revealed that there is a wide range of technical knowledge and safety awareness about light curing procedures.2 Dental resins vary in their energy requirements for adequate curing. Undercuring resins may cause increased rates of post-operative sensitivity, increased wear and fracture, more debonding, more bulk discoloration or marginal staining, and increased incidence of recurrent caries and pulpal pathoses. The following is a brief evidenced-based list of the key points to ensure safe, effective and efficient light curing protocols in clinical practice. These recommendations are based on the research literature and a series of consensus statements developed by a group of key opinion leaders who have met regularly at Dalhousie University in Halifax, Canada for the last five years (Figure 1).3,4

Light curing unit selection
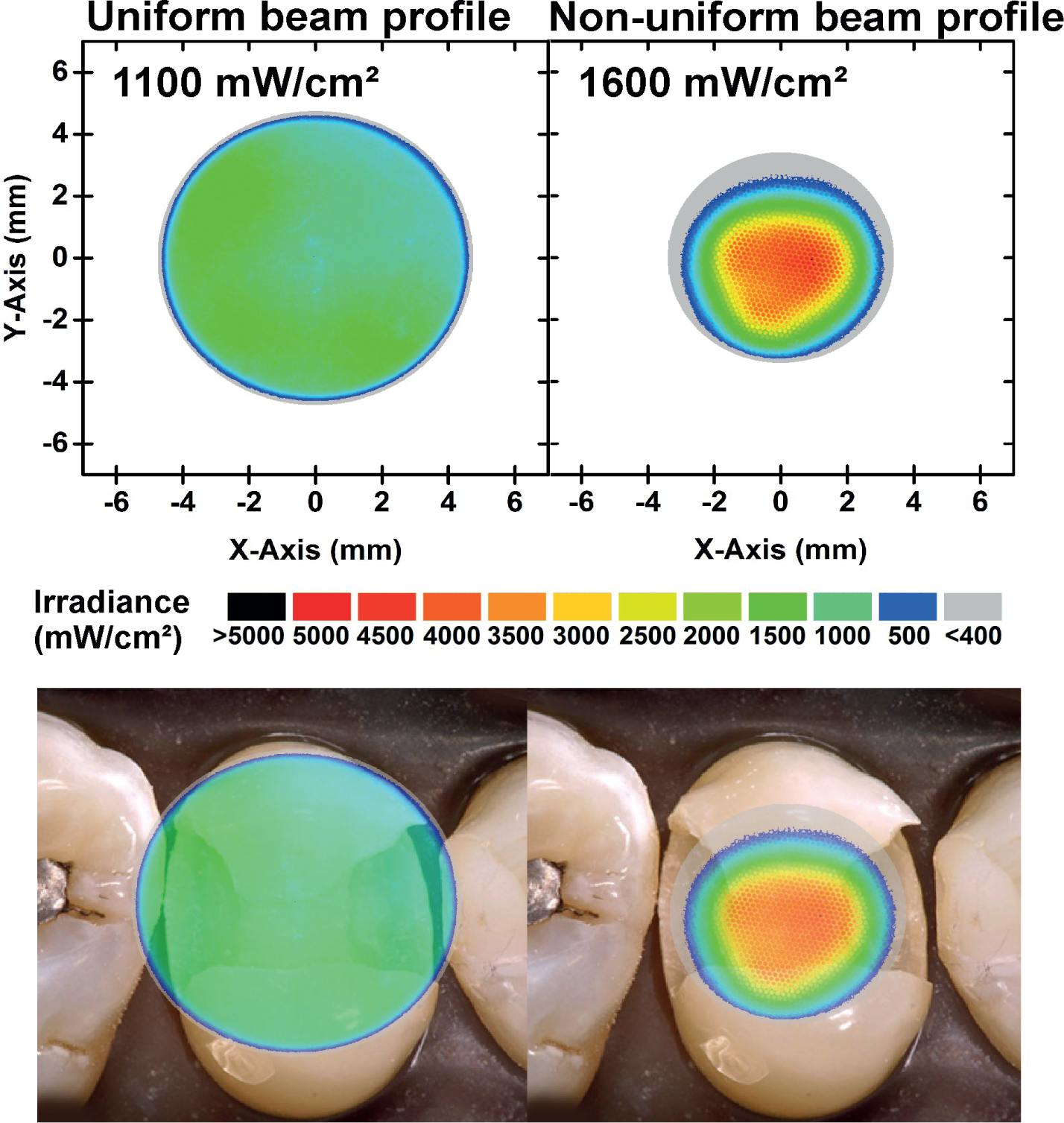
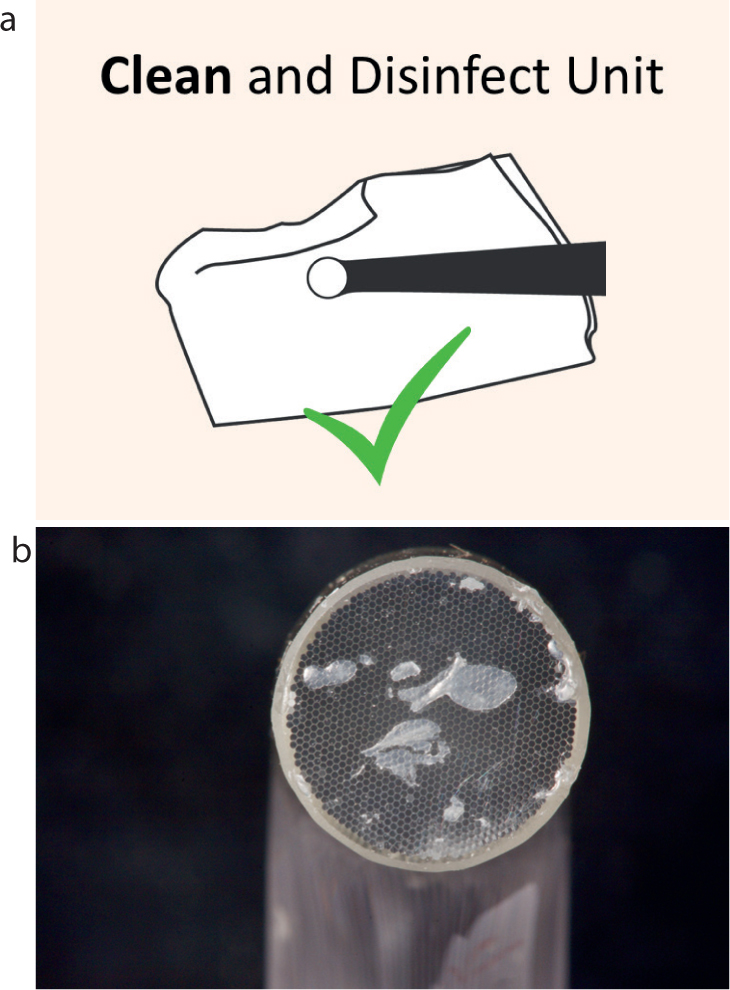
Despite many manufacturers producing excellent curing lights, the units in many dental offices are often not performing effectively and dentists generally have no accurate way of assessing their light output. LED lights are rapidly replacing the older quartz tungsten halogen lights because they are lightweight and compact, often cordless, the LEDs can potentially last for 1,000s of hours, and they are spectrally efficient. However, they have some problems. A major issue is that the light usually comes from a relatively small LED emitter and the light output is frequently not uniform across the exit face of the light source. This produces irradiance ‘hot and cold’ spots of light (Figure 2). Practitioners may be tempted to purchase uncertified units that can have poor optical designs and inferior electronics from online sources for a low price. The risks of using such an uncertified device frequently do not become apparent until it is too late.
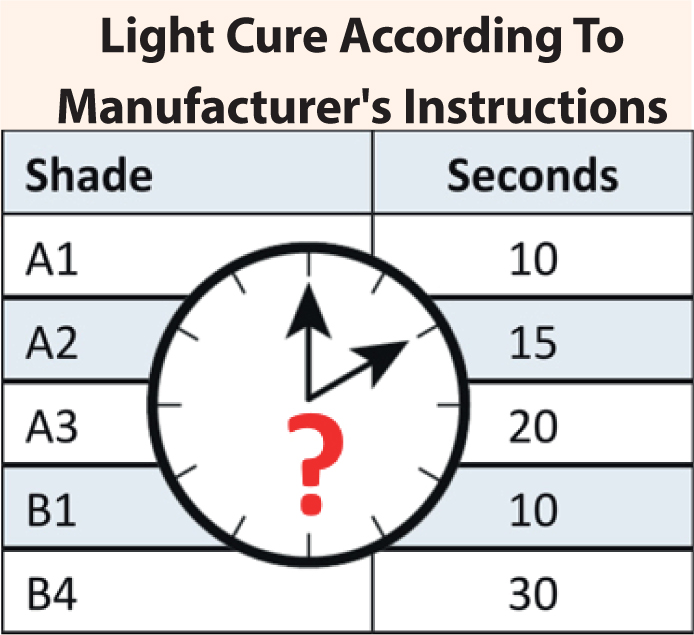
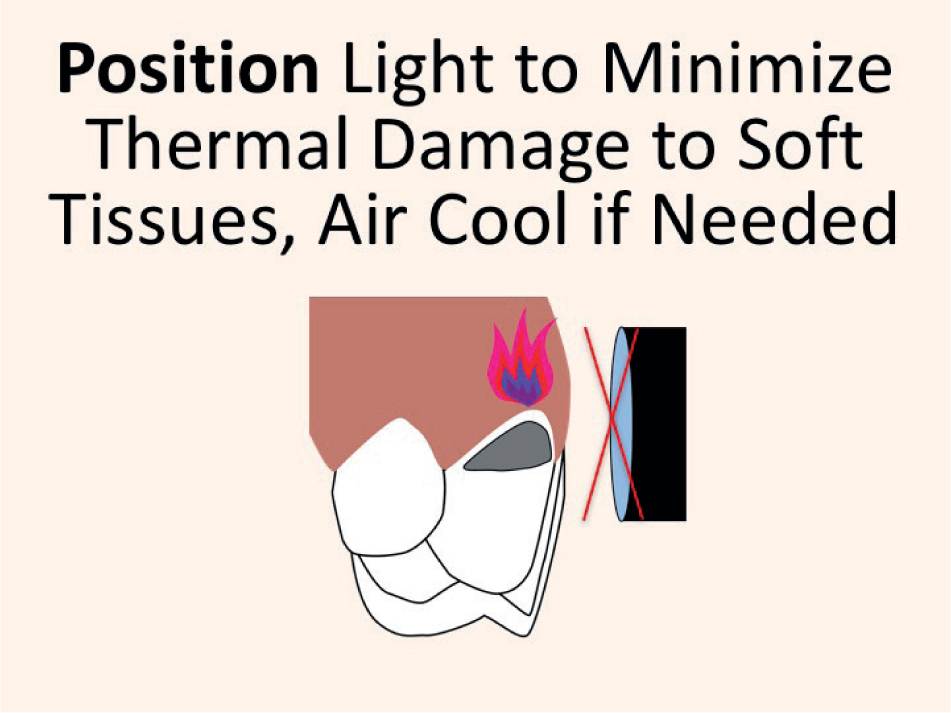
Appropriate irradiance ranges
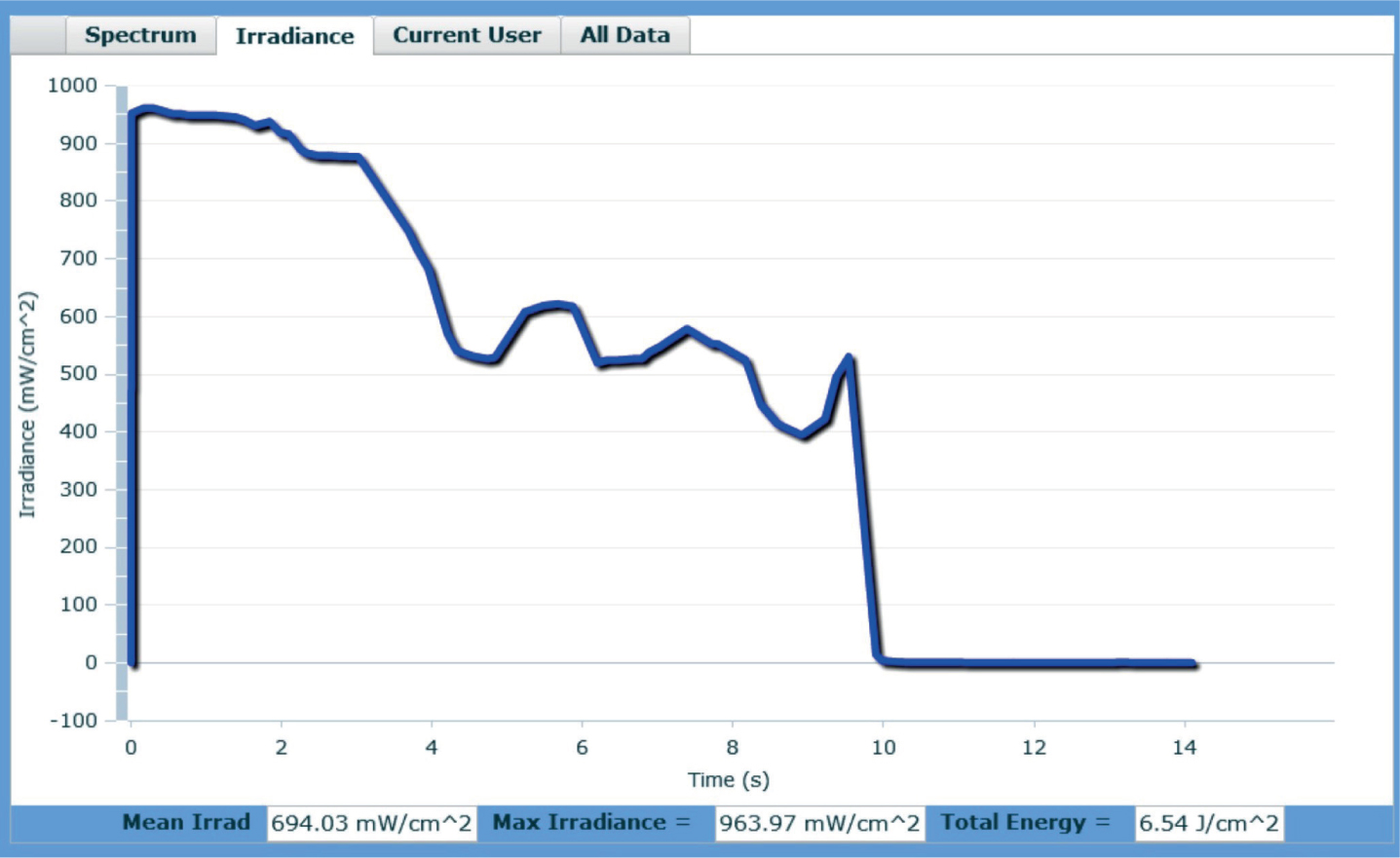
Dentists are recommended to purchase their new curing lights from major reputable manufacturers who have designed high-quality, well-tested, safe and effective equipment. The goal should be to deliver sufficient energy safely to cure the resin adequately without overheating the tooth and adjacent soft tissues. With today's resins, lights that deliver an irradiance >2,000 mW/cm2 and claiming cure times under 10 s should be used with caution. Longer cure times of 10−20 s with irradiance range 1,000−1,500 mW/cm2 are generally recommended. Blowing air or using high volume aspiration to draw air across the tooth helps to minimize temperature rise. Some guidelines to help dentists select, care for and use curing lights have recently been published.5,6
Influence of training
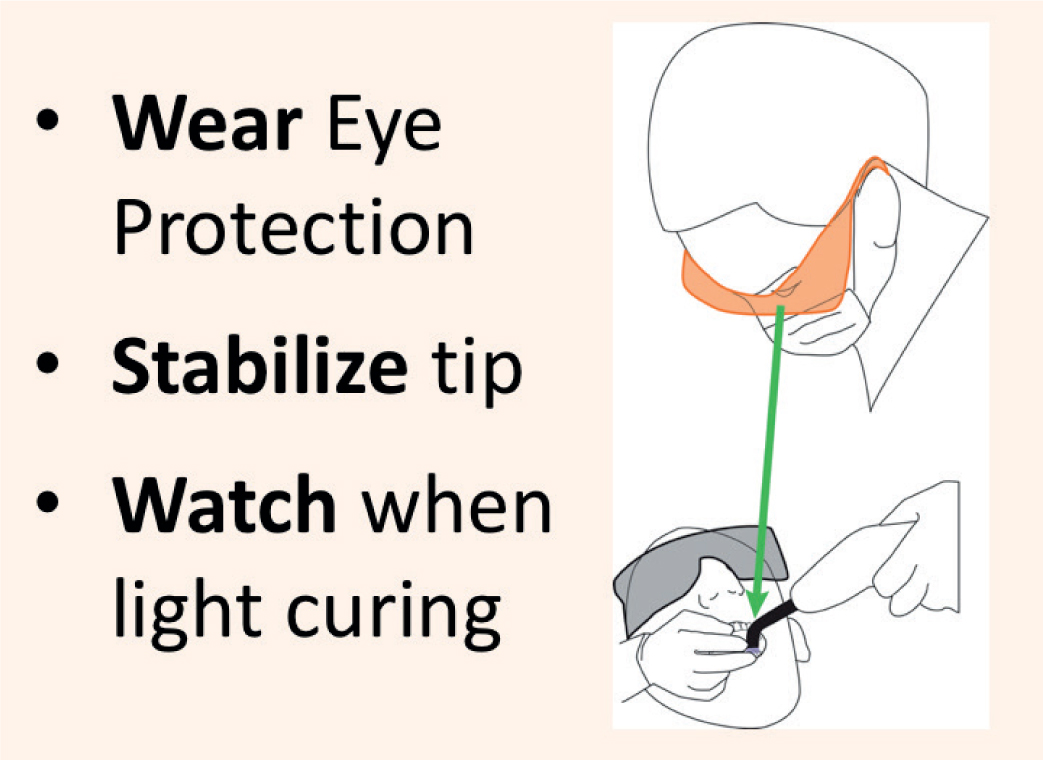
Studies have shown that successful light curing is not trivial and there can easily be a 10-fold difference between operators in the amount of energy they deliver to a standard preparation in the same time using the same curing light. It is not as simple as switching the light on, looking away, and hoping that the resin gets hard at the bottom (Figure 3).5,6,7
Before starting

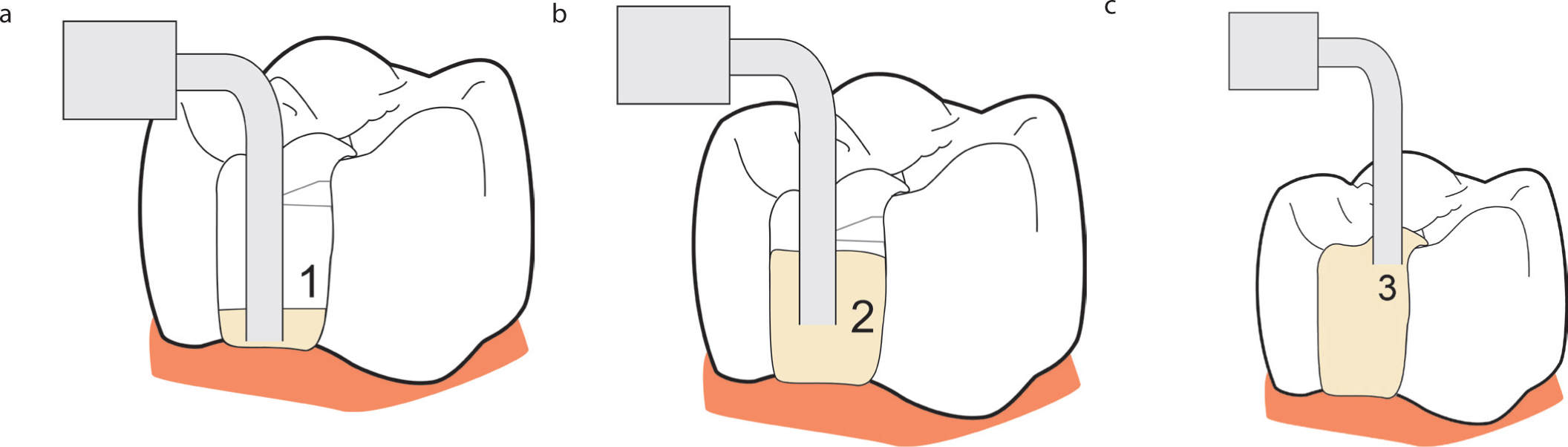
When filling
When filling, ensure increment thickness does not exceed manufacturer's IFU. If using a flowable resin, FILL the preparation from the BOTTOM UP to minimize the risk of trapping air (Figure 9).
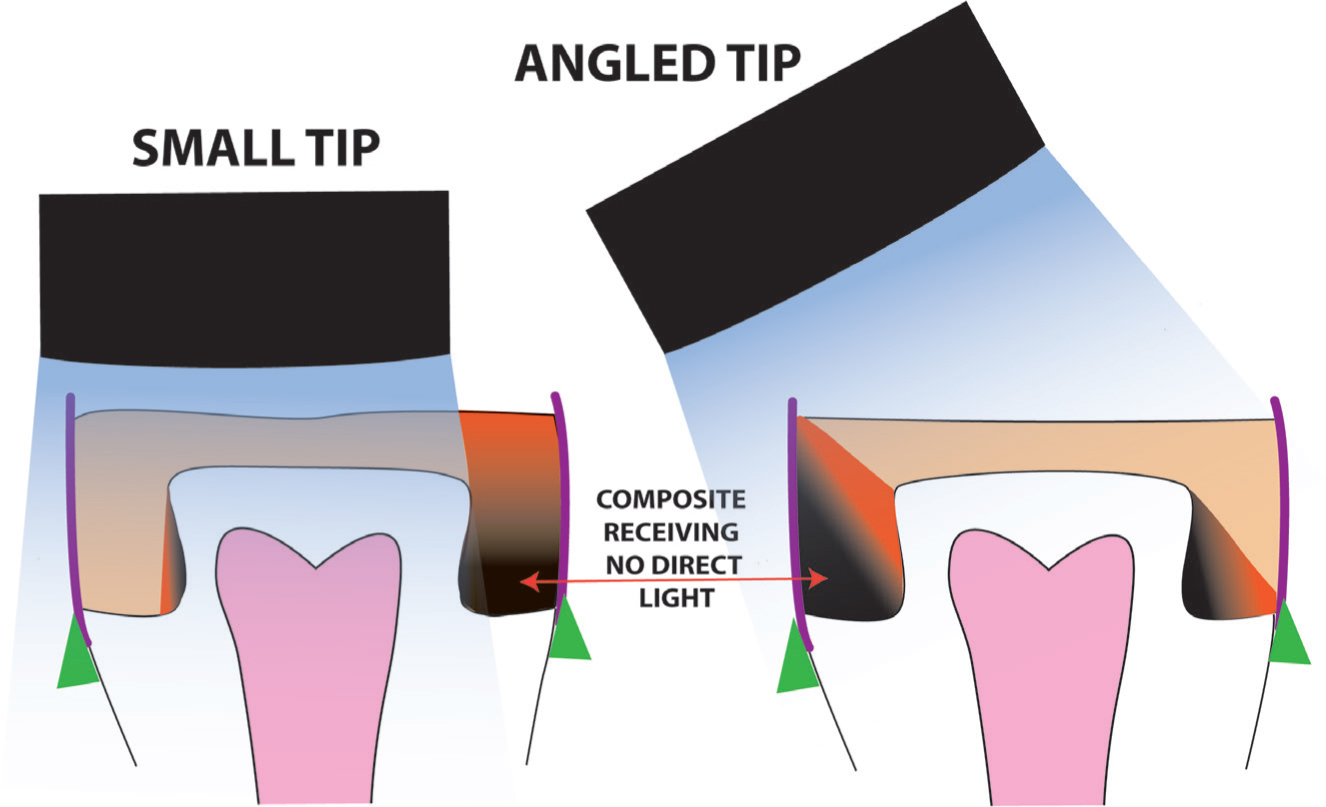
Take aim and light cure
The light source must be directed to cover all of the resin and to avoid shadows, even if this requires overlapping cure cycles. Position the light directly over the region of the restoration to be cured, making sure to minimize soft tissue coverage (Figure 10). Re-irradiation of proximal box regions from the buccal and lingual after the matrix band is removed is an effective means of supplementing curing from the occlusal surface, but it should not be relied upon to provide all the light.9,10
Conclusion
This article provides a summary of the key points that should be considered when light curing RBC restorations. Practical advice is given on protocols which will allow safe, effective and efficient restorative practice.

