References
Complications in managing tooth wear; exploring a potential pitfall of using the dahl approach – a case study
From Volume 45, Issue 4, April 2018 | Pages 320-326
Article

Tooth wear (tooth surface loss) is often defined as loss of the dental tissues by any cause other than trauma or caries. It is a common condition in the dentate population, with the 2009 Adult Dental Health Survey recording 77% of British adults presenting with some form of wear to their anterior dentition, 15% of adults showing moderate and 2% showing severe wear.1 Severe wear is significantly associated with increasing age2 and, when considering the data from the Adult Dental Health Survey showing increased tooth retention throughout life,1 the incidence of tooth wear is set to increase overall. Such information highlights the importance for general dental practitioners in assessing, diagnosing and managing cases of tooth wear.
The aetiology of tooth wear for each individual wear case should be identified. These cases usually show elements of erosion, attrition, abfraction or abrasion, but it is important to note that these often do not occur in isolation and each case is usually multifactorial. Elements can then be addressed through diet analysis, oral hygiene instruction, fluoride therapies and other preventive aids. Age is an important factor when assessing risk; the level of wear present in an 82-year-old could be deemed acceptable as it has occurred slowly over many years, but the same amount in an 18-year-old could be alarming, requiring greater intervention. A number of diagnostic or grading criteria exist to assess wear, such as the Smith and Knight Wear Index3 (Table 1) or the Basic Erosive Wear Examination4 (Table 2). The use of such an index may help guide users as to the severity of wear present and thus the level of intervention required.
| Score | Surface | Criterion |
|---|---|---|
| 0 | B/L/O/I |
No loss of enamel surface characteristics |
| 1 | B/L/O/I |
Loss of enamel surface characteristics |
| 2 | B/L/O |
Loss of enamel exposing dentine for less than one-third of the surface |
| 3 | B/L/O |
Loss of enamel exposing dentine for more than one-third of the surface |
| 4 | B/L/O |
Complete loss of enamel, or pulp exposure, or exposure of secondary dentine |
| Score | |
|---|---|
| 0 | No erosive tooth wear |
| 1 | Initial loss of surface texture |
| 2 | Distinct defect, hard tissue loss <50% of surface area |
| 3 | Hard tissue loss ≥50% of the surface area |
The management of moderate to severe wear can be complicated by reduced space for restorations and the associated need to change the occlusal vertical dimension (OVD). In 1975, Dahl first discussed the concept of using a cobalt chrome splint worn for 12 months to allow space to restore a worn anterior dentition.5 This work was further refined in 1982 when Dahl demonstrated that the splint provided space by allowing the intrusion of anterior teeth and eruption of posterior teeth over time.6 In contemporary clinical practice the Dahl concept has evolved, with composite resin now in use instead of a metal splint. This approach has proven successful, with a recent systematic review of composite used in wear cases, suggesting survival rates of over 90% at 2.5 years and that increasing the OVD resulted in posterior occlusion re-establishment within 18 months for 91% of patients.7
This success is reflected by the number of publications discussing the Dahl approach and the number of case studies demonstrating its use. Unfortunately, as far as the authors are aware there are few publications dedicated to discussing the issues which may be encountered whilst using the Dahl approach. The following case report aims to address this subject by detailing an uncommon problem experienced during the rehabilitation of a patient with excessive wear by first attempting to apply the Dahl method. The report discusses difficulties encountered related to the severity of the Class II skeletal profile, the unusual challenge it poses whilst managing a wear case and how similar difficulties could be addressed in future. The treatment was carried out by a Final Year Dental Student at Newcastle Dental Hospital.
Clinical report
A 45-year-old female patient was referred to Newcastle Dental Hospital in 2009 concerned about the appearance of her teeth and complaining of tooth sensitivity. Medically, the patient reported acid reflux for which she had recently been prescribed omeprazole. The patient did not smoke and consumed about 28 units of alcohol a week; interestingly, she admitted that amounts had been higher in the past.
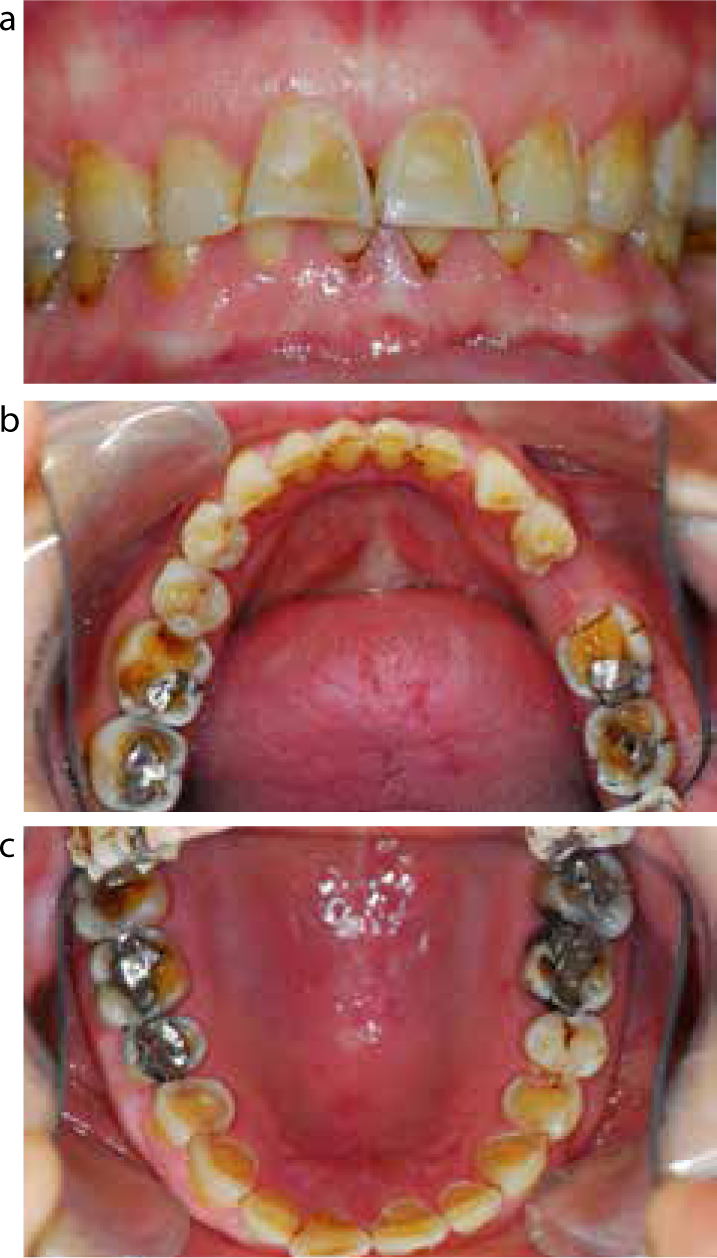
Extra-oral examination revealed slight hypertrophy of the masseter muscles bilaterally, possibly indicating a history of parafunction. Intra-oral examination revealed a reduction in clinical crown height, a Class II division 1 incisal relationship and an apparent Class IV Ackerly traumatic incisor relationship8 (Table 3). A pattern of generalized tooth wear was seen, as shown in Figure 1, with an appearance suggesting a combination of erosion and attrition. This was graded as a combination of 2s and 3s using the Smith and Knight Wear Index3 (Table 1).
| Class | Description |
|---|---|
| I | Mandibular incisors impinge into the palatal mucosa behind the maxillary incisors |
| II | Mandibular incisors impinge into the gingival sulcus of the maxillary incisors |
| III | Maxillary and mandibular incisors are lingually inclined, causing both impingement of palatal mucosa by mandibular incisors and labial gingiva by maxillary incisors |
| IV | Abrasion facets present on palatal surfaces of maxillary incisors |
Radiographic examination demonstrated generalized tooth wear, deficient restorations in the LR6 and UL6 and a lost restoration in the UL4. Alveolar bone levels were largely concurrent with age and no signs of periapical pathology were observed.
The following diagnoses were made:
A preventive regimen was initiated through dietary advice which highlighted the high consumption of wine and carbonated drinks. High-strength fluoride toothpaste and fluoride mouthrinse were prescribed.
Once the oral environment was considered to have been stabilized, the planning of the tooth wear management was undertaken. Articulated study casts were mounted in centric relation using a facebow (Whip Mix, Model 8645, USA) and a bite wafer taken with Beauty Pink Hard Wax (Integra Miltex, USA) in pre-contact centric relation; this facilitated the creation of a diagnostic wax-up. The diagnostic wax-up was designed to increase the OVD by 3 mm anteriorly, allowing space for restorations, and was shown to the patient who was happy to proceed. It was decided that this increase could be best achieved using directly placed resin composite restorations so as to preserve as much tooth tissue as possible. Restorations were designed on UR3–UL3 with cingulum palatal stops. The space seen posteriorly would then be reviewed to observe for a ‘Dahl effect’.6
To assist in the placement of these restorations, an unmodified thermoplastic matrix was constructed from the diagnostic wax-up. This was sectioned between the anterior teeth UR3–UL3, with a cellulose strip placed interproximally on the matrix. Each tooth was then restored sequentially by placing composite into the matrix, seating in the mouth and curing, with the restorations adjusted until the correct occlusion was established and then polished. This technique has previously been discussed in detail by Daoudi and Radford.9 On completing the upper labial segment, it was observed that the patient was not occluding on all of the cingulum stops; as such, it was decided to review the patient before proceeding further.
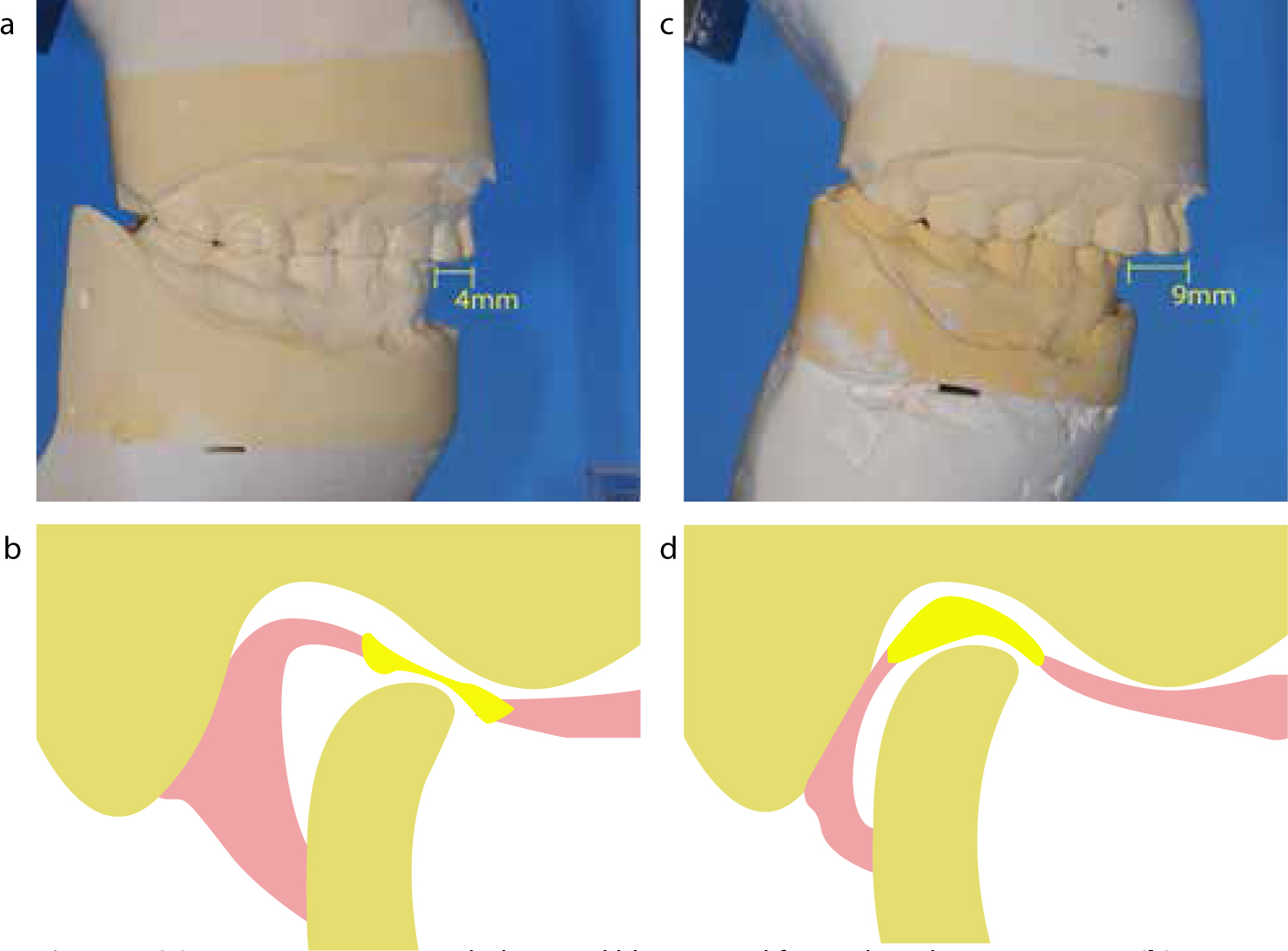
At review, 2 weeks later it was determined that the patient's ICP (intercuspal position) had changed, with the condylar position becoming further distalized from where we had initially estimated it would be in CR (centric relation). The result is shown in Figure 2 with a change in overjet from 4 mm to 9 mm giving the appearance of a more pronounced Class II division 1 incisal relationship. The tips of the mandibular incisors were now occluding 0.5 mm behind the cingulum stops but light contacts were still present on the canines. It was determined that this change was most likely a result of an error at registration, with the patient habitually posturing forward to find anterior tooth contact and therefore CR not being captured. This new occlusal relationship more accurately represented the patient's true centric occlusion. It is therefore difficult to determine if any increase in OVD had been achieved, however, as the mandible had effectively been distalized, such an increase was no longer required, with the translation providing space both anteriorly and posteriorly. Due to the presence of this posterior space and the stability of this occlusion, it was decided to restore the remaining dentition by conforming to this newly established occlusion rather than altering it further.
A modified treatment plan was agreed with direct resin composite restorations placed to UR7, UR4, UL4, UL5 and LL2–LR2. Deficient amalgams in UR6, UR5, UL6, UL7, LL7, LR6 and LR7 were removed and replaced with composite. This material was selected to preserve tooth tissue and would ensure correct interproximal and occlusal contacts, conforming to the newly established mandibular position. Finally, a soft splint was provided for night-time use to reduce further tooth wear and act as a retainer for the anterior dentition.
Following this the patient was reviewed as shown in Figure 3 and, despite the challenges encountered, treatment from her perspective was judged to have been a success. The patient was comfortable with a reduction in tooth sensitivity. She was able to function (chewing and speech) freely, the aesthetics were acceptable and the occlusion appeared to be stable.

Discussion
When initially planning this case it had been thought that, although the patient already showed a Class II division 1 incisor relationship, she could be adequately restored using the Dahl approach. The extent of the incisor relationship and underlying skeletal pattern proved this was not the case. This relationship was masked by the severity of the patient's mandibular posturing to find ICP, which was interesting in that it still allowed posterior contact in occlusion, possibly due to the anterior wear. It is clear now that the strength of such posturing meant that CR was not accurately captured for the planning of the occlusion. Subsequently, the patient's mandible distalized following the anterior build-ups, revealing the true extent of the incisal relationship and allowing the adoption of an ICP which more closely resembled the patient's CR.
One explanation for the severity of this posturing is that this patient could represent a dual bite. This is a term usually applied to a patient for whom the anteroposterior difference between RCP (retruded contact position) and ICP is greater than 2 mm and for whom two occlusal positions exist which fit easily together and which the patient can easily use.10 A difficulty in applying this term to this case is that the strength of the posturing meant that it was not easy to move the patient between the two positions, meaning that this case may not represent a true dual bite. An alternative theory is that this could represent a ‘Sunday bite’, a term used in Orthodontics for the tendency of Class II patients to posture the mandible forwards, making the occlusion appear better than it is.11
Despite these terms, there is very little within the literature devoted to how wear should be managed for different skeletal classifications. However, both demonstrate the importance of accurately capturing CR and, with hindsight, a case of such habitual posturing could have benefited from the use of a deprogramming device, for example a lucia jig12 or stabilization splint. Each of these devices could have aided in allowing the operator to estimate CR accurately. In addition, a stabilization splint could have tested the patient's tolerance of a proposed change in occlusal vertical dimension. This highlights how a period of wearing such a device during the prevention and stabilization period might aid with treatment planning.
It was the distalization of the mandible in this case which ultimately allowed space to restore the anterior and posterior dentition. Distalization has been used previously to manage wear and, in 1984, Turner and Missirilian13 listed this as one of three methods to manage wear cases. Category 2 patients, were described as having excessive wear without loss of occlusal vertical dimension but with space available, representing cases with adequate posterior support but with wear anteriorly causing posturing to an edge to edge incisal relationship. Turner and Missirlian suggest that these patients often had a significant slide from CR to ICP and that stabilizing the patient in CR could provide sufficient space for anterior restoration.13 Furthermore, in 1993, Dahl discussed the ability of excessive tooth wear to lead to a more anteriorly adopted ICP, resulting in an increase of the distance between ICP and CR, and listed exploitation of this difference as one of three ways in which space can be created for restorative materials.14
There is therefore a precedent for managing wear by mandibular distalization, but it is worth noting that none of these publications mention how much of a difference from CR to ICP to expect, meaning that this will likely be variable in amount and a slide of the size seen in this case would be unusual in most cases. This means that this technique of mandibular distalization, or exploiting the difference between CR and ICP, represents a potential challenge that dentists should be aware of when managing wear cases, rather than a technique which should be adopted in every case. For those cases where such a significant difference does exist, this technique for reorganization could allow an improvement to both aesthetics and function without needing a significant rotation of the mandible.
If mandibular distalization was to be undertaken, the large horizontal difference needs to be considered as it may be challenging for patients to tolerate. In addition, as in this case, the absence of contact between the maxillary and mandibular incisors could be an issue, leading to overeruption or proclination of the incisors in an attempt to re-establish occlusion. It was for this reason that a soft splint was provided to act as a retainer and the need for regular check-ups was stressed to the patient. Happily, in this case, neither of these appeared to be an issue for the patient, who reported an improvement to both function and aesthetics at the end of treatment, while no sign of anterior movement was seen upon review.
Prior to the publication of this report, contact with the patient to offer another review appointment was attempted but unsuccessful. This review would have focused on assessing for any further signs of mandibular posturing, considering replacement of posterior composite with extra-coronal restorations and attempting to determine splint tolerance as well as assessing for anterior movement.
Conclusion
The diagnosis and subsequent management of tooth wear can be challenging where there is a strong postural position of the mandible retained by a patient. The reported case highlights issues that should be considered when planning and managing tooth wear, particularly when attempting the Dahl approach:

