Abstract
This paper, the first of two, provides an introduction to implant dentistry for the general dental practitioner.
From Volume 43, Issue 5, June 2016 | Pages 410-416
This paper, the first of two, provides an introduction to implant dentistry for the general dental practitioner.

The widespread use and published success1,2 of dental implant-supported restorations is encouraging an increasing number of GDPs to become involved in this treatment modality. A visit to the dentists' section of the Yellow Pages makes it difficult to ignore the fact that more and more practitioners are using the label ‘Cosmetic and Implant Practice’.
This paper aims to address the scope of dental implant treatment within the general dental practice environment taking into consideration:
The GDC's Scope of Practice describes the provision of implants as an additional skill that dentists could develop during their career.3 The Faculty of General Dental Practitioners (FGDP) implant training guidelines state ‘The skills and knowledge necessary for competence should be developed through a training course in implant dentistry, with a suitably trained and experienced clinician acting as a mentor.'4 Fortunately, there appears to be an increasing trend in teaching implant dentistry in the undergraduate curriculum,5 but the GDP of today must look to postgraduate education for the competencies required to introduce implant treatment to his or her practice. Such competencies and their means of delivery are well documented2 and increasingly frequently the use of Information Communication Technology (ICT) is being used to minimize disruption to the working routine of the busy GDP.6,7
From a marketing perspective, the UK market for implants and final abutments was the sixth largest in Europe in 2010 with 34 implants placed per 10,000 people, which is the lowest per capita penetration in all of the 17 countries surveyed. The same report predicted a compound annual growth rate in the implant market of 15.4% to 2017.8
Combine this with patient exposure to implant dentistry through the national press and media, along with patients' mind-set on dental implants as described by Pommer et al9 and it becomes understandable that more practitioners are becoming involved in implant treatment. The study by Pommer et al indicated that, when results of a survey carried out in 2003 were compared with a rerun of the same survey carried out in 2010, the awareness rate of dental implants was significantly higher, with the majority of the population surveyed stating that they would not be content with a removable denture to replace missing teeth.9
When one looks at the available education and training in implant dentistry, as Weber says in his foreword to the book Practical Implant Dentistry:
‘Due to the rapid development of dental implantology, and based on the fact that within dental implantology a unique unification of surgical and restorative procedures can be found, the academic and practical education within the dental education programmes is still lacking – although it is there.'10
A recent study examining the attitudes of GDPs towards providing implant dentistry concluded that dentists perceived implant-supported single tooth prostheses to be superior to natural tooth-supported prostheses, but goes on to state that GDPs' attitudes are not wholly in line with current evidence-based knowledge.11 This would suggest that there is a lack of appropriate education in implant dentistry within the profession.
The paper by Andersson et al1 suggests that success rates for single tooth implant prostheses provided by GDPs is equivalent to those provided by specialists, but highlights the fact that the GDPs involved in the study had received training in implant dentistry. However, the recent study by Da Silva et al12 concludes that the three to five years for success and survival of implants in general practices may be lower than those reported in studies conducted in academic or specialist settings.
The variety of treatments involving implants offered in general practice ranges from single tooth replacement to full mouth rehabilitation. Indeed, it is suggested that the implant-supported single crown will replace the 3-unit fixed partial denture (FPD)2 and widely accepted that the first choice standard of care in the edentulous mandible is the two implant-retained overdenture.13 The use of dental implants as temporary anchorage devices (TADs) in orthodontic treatment is also becoming more commonplace.14 The ultimate goal of the patient is to have the failing or missing teeth replaced in the shortest possible timeframe with the minimum expense. Consequently, we see protocols such as TeethXpress® (BioHorizons, Birmingham, Alabama, USA) and All on 4® (Nobel Biocare, Zurich, Switzerland) more frequently offered as treatment options. However, the author would like to stress the need for appropriate education and training in implant dentistry as described in the GDC Training Standards in Implant Dentistry document.4
The key to a successful outcome is thorough case assessment and treatment planning.15 There is a common saying in implant dentistry – ‘All implant systems work' but perhaps the following caveat should be added – when used by trained hands controlled by an educated mind. This emphasizes the need for comprehensive education and training in implant dentistry as opposed to the early, largely company run, programmes that focused solely on product knowledge.
The clinician should begin with the end result in view to determine whether or not it is achievable. This will be discussed in more detail in part two of the series. If the presenting alveolar foundation will not allow the desired implant-supported restorative outcome, then the treatment plan must be changed. For example, if there is inadequate bone volume to accommodate the implant in the ideal 3-dimensional position, bone augmentation may have to be considered. If there is inadequate space horizontally or vertically, orthodontics or bite opening may be required. Even when the criteria to provide a long-term successful implant-supported restoration can be met, alternative treatment options must be discussed as part of informed consent and the practitioner must be in a position to underpin his or her decision with supporting evidence.
As with all case assessment, the patient's medical history is central to decision-making. Much has been written of the more commonly encountered medical complications and social habits encountered in general dental practice that impact upon dental implant prognosis, such as diabetes, osteoporosis and smoking.
Current evidence suggests that the diabetic patient, when well controlled with a glycosylated (glycated) haemoglobin (HbA1c) ≤7%, can be treated with similar expectations as the non-diabetic patient.16 Thomas et al17 take the discussion a step further stating that the improved masticatory function provided by dental implant therapy may well have a positive effect on the control of the disease and therefore the diabetic patient in need of oral rehabilitation should seriously consider such treatment.
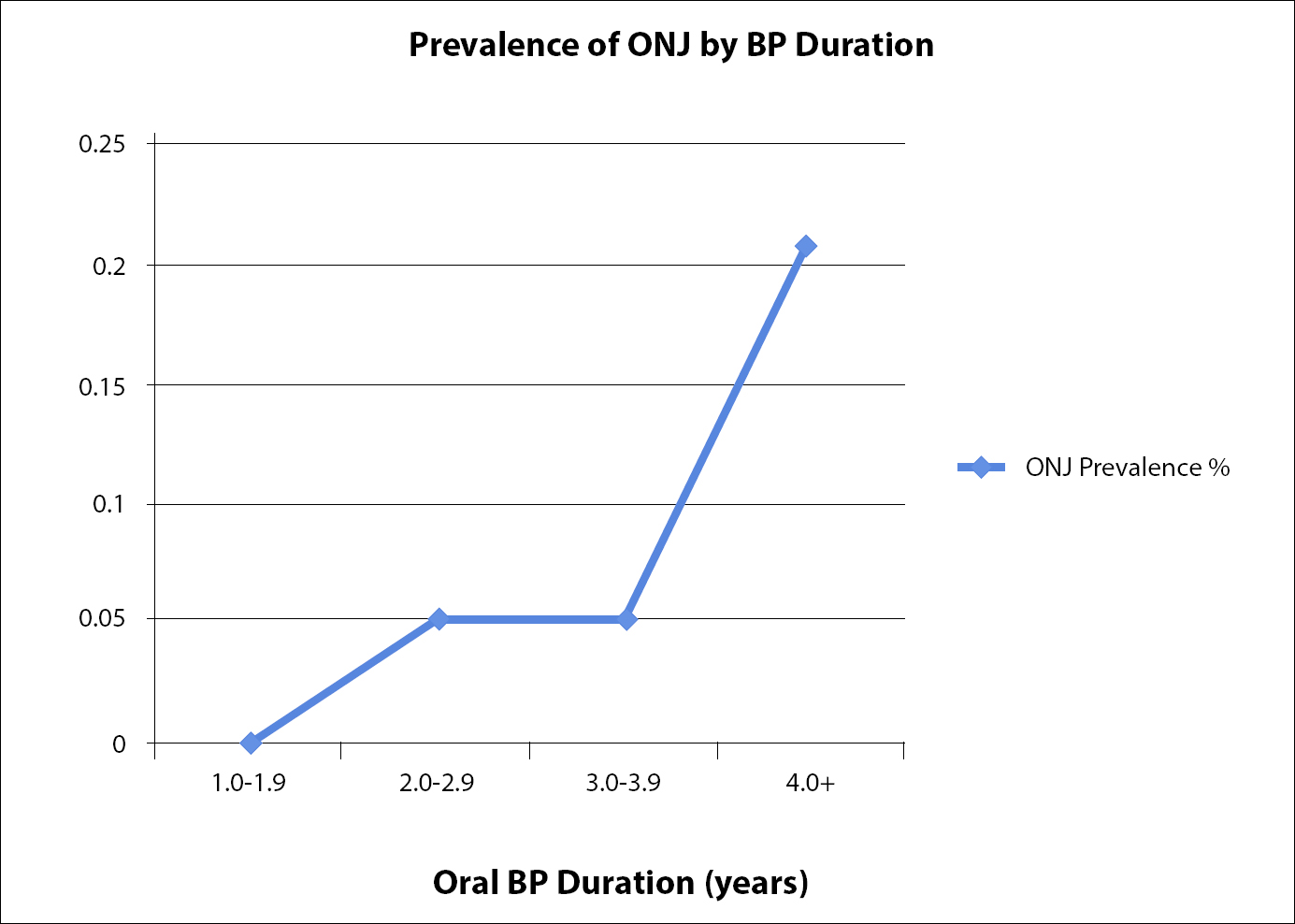
Owing to the widespread use of bisphosphonates for osteoporosis, the potential complication of bisphosphonate related osteonecrosis of the jaws (BRONJ) in patients being treated for the disorder has been very topical for the last few years. The American Association of Oral and Maxillofacial Surgeons (AAOMS) has taken a stance on the risk presented by dental surgery, including dental implants, and propose the term medication-related osteonecrosis of the jaw (MRONJ) due to the increase in the number of cases involving non-bisphosphonate anti-resorptive drugs.18 Others use the term chemo-osteonecrosis of the jaws (CONJ). This complexity of nomenclature invariably arises in idiopathic conditions. The Association of Dental Implantology UK19 quotes the risk for BRONJ from approaching 20% in patients treated with IV bisphosphonates, to the lowest risk of 0.34–4% in patients taking oral bisphosphonates. Patients receiving IV bisphosphonate should be treated in the hospital environment. Figure 1 graphically illustrates the relationship between prevalence of osteonecrosis of the jaws and duration of oral bisphosphonate therapy, showing the prevalence is only 0.2% even after 4 years of oral treatment.
The AAOMS state that the incidence of MRONJ resulting from implant placement is unknown, however, they consider the degree of manipulation of bone involved in the procedure to be similar to that of tooth extraction. The best current estimate for the risk of osteonecrosis of the jaw for patients exposed to oral bisphosphonates after tooth extraction is 0.5%.18 The concept of a drug holiday for patients receiving oral bisphosphonates has been much debated and, although there is little evidence to support current recommendations, the AAOMS consider a two month drug-free period prior to invasive dental treatment a prudent approach for patients who have been receiving oral bisphosphonate therapy >4 years.18
Where bisphosphonate is essential, as in hypercalcaemia of malignancy, oral surgical intervention must be avoided.
Bain and Moy20 were among the first to identify smoking as a significant risk factor to implant survival. The significance was quantified by Sanchez-Perez et al21 when they investigated the survival of implants in non-smokers, light to moderate smokers (<20/day) and heavy smokers (>20/day). They concluded that non-smokers had a 1.4% risk of failure, light to moderate smokers a 10.1% risk of failure, and heavy smokers a 31% risk of failure. Overall, smokers had a 15.8% risk of failure. However, this was a relatively small retrospective study and the reader should always be aware that it is difficult to isolate and investigate any one single factor relating to implant success or failure effectively. In a systematic review and meta-analysis, Streitzel et al22 investigated how smoking interferes with the prognosis of dental implant treatment. Their review included papers that ignored the number of cigarettes smoked per day and papers that varyingly classified smokers as ‘heavy’ or ‘light’, depending on the number of cigarettes smoked per day. The conclusion of the study was that smoking presents a considerable risk factor to the success of dental implants. The important thing is to be aware of the relevant evidence and to communicate that evidence to the patient as part of informed consent.
The dental history should be thoroughly investigated. Untreated periodontal disease is to be recognized as a marked contraindication to implant treatment. What was the reason for tooth loss? Is the patient a regular attender? As Rinke et al23 point out, patients should be informed of the absolute need of post-therapy care before undertaking implant treatment. Their study highlights the increased incidence of peri-implant disease in patients who do not attend for regular maintenance therapy, with even greater incidence if the patient is a smoker.
Are these realistic and can they be readily met with implant treatment? Figures 2 and 3 show an example where a 33-year-old female wished to have her upper incisors replaced with implants in order to improve their appearance. Her presenting complaint was that she did not like the ‘look’ (proclination) of her upper incisors. She wanted a ‘Hollywood smile’. This patient was referred for an orthodontic opinion.


The salient features of case assessment and patient selection for implant treatment are discussed in part two of this series: ‘Treatment planning’.
This should include facial symmetry, the resting lip-line and the smile-line. The implant-supported restoration can provide both aesthetic form and function but aesthetics are much more of a challenge to deliver predictably and, where the patient shows gingival tissue on smiling (Figure 3), one should proceed with extreme caution. Severe cases usually need a maxillary surgical impaction for aesthetic correction.
The patient presenting with a low smile-line (Figure 4) usually offers less of an aesthetic challenge. However, be very aware of patient's expectations. A definition of the aesthetic zone is often offered in implant dentistry and generally accepted as the area of tooth and soft tissue exposed when the patient smiles. A better description might be ‘wherever the patient thinks it is’. Consider the patient for whom you fit a crown on a second molar and the patient goes to great lengths to examine the restoration. It should not be taken for granted that a low smile-line will be less of an aesthetic challenge.

When examining a patient's removable partial denture, note the volume of pink acrylic present. This is an indication of the volume of lost hard and soft tissue. It is a relatively straightforward procedure to replace lost hard and soft tissue on a denture by adding pink acrylic, but much more challenging to do the same surgically on the patient by adding soft tissue, bone or a combination of both. The greater the volume of pink acrylic the greater should be the concern of the implant practitioner. Any indication of wear or damage to the prosthesis can also be a warning signal as it may indicate the potential for occlusal overload on the implant-supported prosthesis. The cause of the wear or damage should be clearly identified.


As was stated earlier, it is essential to envisage the final restoration and work back from there. Articulated study casts and a diagnostic set-up will greatly assist with this and also help convey the nature and proposed outcome of the treatment to the patient.
Appropriate radiographs should be taken following the ALARA (as low as reasonably achievable) principle. The use of Cone Beam Computed Tomography (CBCT) appears to be growing in popularity but, as with all radiographs, exposure of the patient must be justified by weighing the risks against the benefits.25 Fortunately, guidelines exist.26,27 The European Association of Osseointegration recommends that ‘a dentist involved in CBCT imaging for implant dentistry undergoes a period of additional theoretical and practical training that has been validated by an academic institution (university or equivalent).'26
Finally, the clinician should consider the need for any additional investigations, the simplest and most common of which is vitality testing of teeth adjacent to the proposed implant site(s).
Having thoroughly assessed the patient and identified the salient features of the case, the clinician is then in a position to begin the treatment planning process and to consider treatment options, eventually arriving at a definitive treatment plan and informed consent.
Ensuring that the clinician has the appropriate knowledge and skills to undertake dental implant treatment is of paramount importance. The first step towards treating the patient is case assessment where attention to detail and identification of the salient features of the case are essential. Even if a general practitioner does not wish to undertake the provision of implant treatment, it is almost certain that he or she will be caring for patients with implant-supported restorations. A component of that care will be assessment of the health of the implant restoration(s) for which an understanding of implant dentistry is essential.
In the second article of this series treatment planning will be considered in depth with reference to the case assessment features highlighted in this article.