Abstract
Interproximal reduction (IPR) has become particularly popular with the use of removable aligners. Clinical and ethical factors concerning the use of interproximal reduction to facilitate orthodontic alignment are discussed.
From Volume 42, Issue 10, December 2015 | Pages 922-924
Interproximal reduction (IPR) has become particularly popular with the use of removable aligners. Clinical and ethical factors concerning the use of interproximal reduction to facilitate orthodontic alignment are discussed.

Are you performing Interproximal Reduction (IPR)? Can you answer the following questions?:
Andrews 6 Keys: The significant characteristics shared by all of the non-orthodontic normals are as follows:
Ethics involves the application of a moral code to your clinical practice. Each patient has the right to choose his or her treatment. If you are providing the treatment you must completely understand the aetiological factors of the malocclusion so that you can fully discuss the risks and benefits, or the alternatives to it – if not, are you truly providing ethical treatment?
Sheridan1 first formally described interdental stripping, although it had been employed in orthodontics for many years. It is also known as interproximal reduction, stripping, slenderizing, selective enamel reduction, interdental enamel reduction or enamel reproximation. It is the mechanical removal of interproximal enamel that reduces the mesio-distal width of a tooth. It has become particularly popular recently, with the burgeoning use of removable aligners.
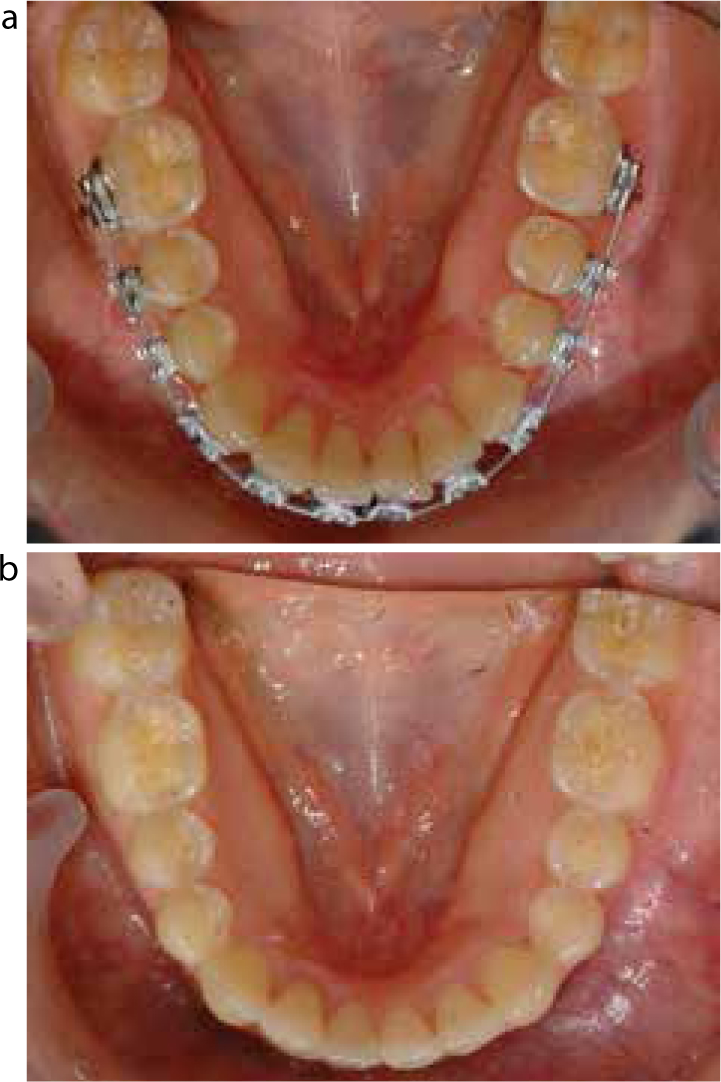
Interdental reduction may be carried out for various reasons in orthodontics. It can be done to treat crowding without recourse to extraction, to reshape teeth, to create contact points that are potentially more stable by flattening curved contact surfaces and to reduce the size of unsightly black triangles between teeth after attachment loss. Figure 1 shows a case where, following successful orthodontic treatment, the effects of gingival recession and tooth morphology issues not considered before treatment have left unsightly spaces at the gingival margin. Interproximal reduction can be used to eliminate these.

Mild malocclusions requiring minor tooth alignment and those where the arch perimeter should not be changed may well benefit from interdental enamel reduction. When resorting to extractions, there is no way of removing tooth tissue that equates to exactly the amount of crowding. There can be an excessive amount of space created which will need to be closed which necessarily increases the treatment time and can potentially lead to relapse issues of space re-opening. It is common to use IPR to allow realignment of the labial segments of adults who otherwise have a good posterior occlusion; this is an attractive option offering quick and simple treatment, but it is often limited by the amount of enamel in the incisor region that can safely be removed.
The canines and premolars have considerably more enamel than the incisors and therefore are a more appropriate tooth for interdental reduction. The molars have more enamel thickness still.2 It has been suggested that approximately 50% of the interproximal enamel can safely be removed,1,3 which provides a potential 2.5 mm anteriorly and 6.4 mm posteriorly. There is individual variation in enamel thickness between ethnic groups, individuals and tooth type; bitewing radiographs will provide information about the amount of enamel at individual sites.4 However, if IPR is done on the posterior teeth, then the orthodontics is much more complex because it requires distal movement of a number of teeth in order to manage the normal labial segment crowding (Figure 2).
A very careful space analysis is required before any treatment is carried out using interdental reduction, to ensure that the symmetry of the dentition is maintained and optimal aesthetics and occlusion are obtained. Over 20% of orthodontic patients present with a tooth size discrepancy (TSD)5,6 and, in order to ensure that the functional occlusion is maintained post treatment, it is also advisable to do a Bolton Analysis.7 If a TSD exists then IPR can be used to correct the Bolton ratio, so benefiting the aesthetics and occlusion. Once an understanding of the tooth sizes has been obtained, interdental reduction can be used to manage the crowding without having to change the arch perimeter drastically. It must be remembered, however that, if enamel is removed only in one arch when there are no tooth size discrepancies, then a perfect Class I interdigitation, and therefore Andrews Six Keys, may not be achievable; some form of compromise of the posterior occlusion or the overjet will be necessary.
If multidisciplinary restorative work is contemplated, a full discussion with the patient and the other specialists must be taken before treatment with a clear treatment plan is agreed by both patient and practitioners. This basis of valid consent is essential prior to any orthodontic treatment with particular reference to treatment that involves irreversible actions.
Once interdental reduction is agreed as part of the treatment plan, its timing should be carefully considered so that the appropriate space is created at the correct site, and tooth movement and anchorage is well managed throughout the orthodontic process. Proposed enamel reduction should be specifically planned before treatment starts, utilizing calibrated radiographs, if appropriate. A diagnostic set-up can be undertaken to ensure that the proposed tooth movements are feasible. The timing of the IPR should also be planned; separation or alignment may be required prior to IPR to improve access, so that reduction is carried out safely in the appropriate place and access to the contact points is easy.
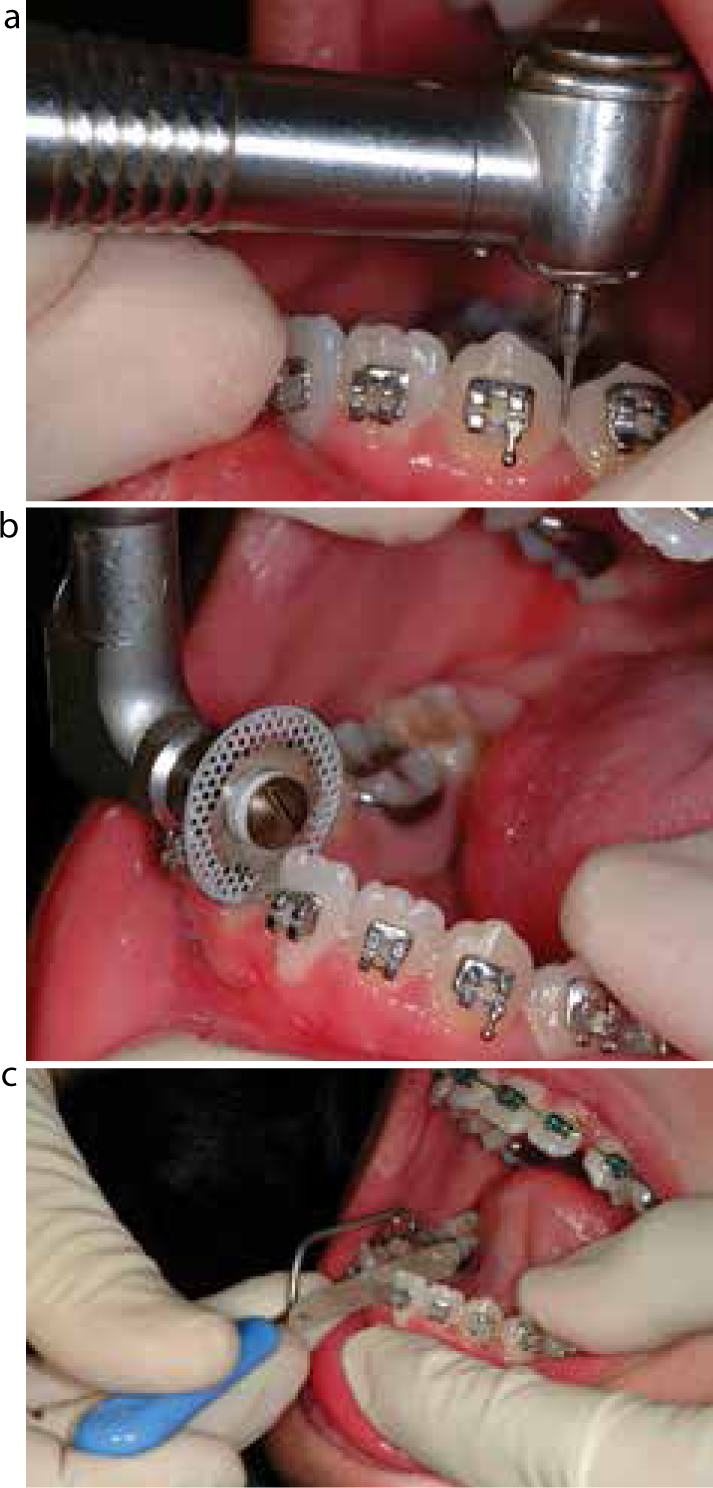
There are a number of methods of reducing enamel interdentally ranging from hand-held abrasive and polishing strips to mechanical polishing burrs and diamond wheels (Figure 3). Diamond wheels and burrs are potentially very destructive and it is essential that the operator understands the implement he/she is using and the amount of interdental reduction that will be achieved by using it. Soft tissues must be completely protected and great care must be taken at the gingival margin level to avoid any form of step that could subsequently become a place of plaque retention and subsequent demineralization, decalcification and decay.
A common IPR protocol will be described briefly below in a stepwise fashion.
The possible iatrogenic results of IPR include:
There are, however, instruments and techniques to ensure minimization of these risks. The mechanical instruments should be water- or air-cooled to reduce/eliminate thermal sensitivity and the lips, tongue and gingival tissues protected as necessary.
There is little evidence to suggest that removing enamel interproximally is deleterious to the dentition. Crane and Sheridan8 did not find any increase in the incidence of caries or periodontal disease 2–5 years after IPR, and Zacchrison et al9 have shown that there are no detrimental periodontal effects after 10 years. Some protocols advise the application of a topical fluoride or casein phosphopeptide-amorphous calcium phosphate (CPP-ACP) to support the remineralization of stripped enamel, however, studies have shown spontaneous remineralization of hard tissues after 9 months without this.10
Each case chosen for IPR must be assessed on its merits; the practitioner is duty bound to be competent to manage the entire malocclusion. As with all treatments, a cautious practitioner acting within his/her competency level, with clear objectives and a conservative approach, is unlikely to cause any long-term damage. It must be understood that IPR is a legitimate part of comprehensive treatment and does not mean that the treatment time will necessarily be shorter. Where there is severe crowding, thin labial gingival attachment or minimal overjet to allow the lower incisors to procline, extraction of one incisor may be a preferable treatment. Often in orthodontics there is more than one way to treat a given malocclusion; a full understanding of patients' motives, their occlusion, the skeletal base relationship and tooth size is essential to guide you towards the most appropriate treatment.