Abstract
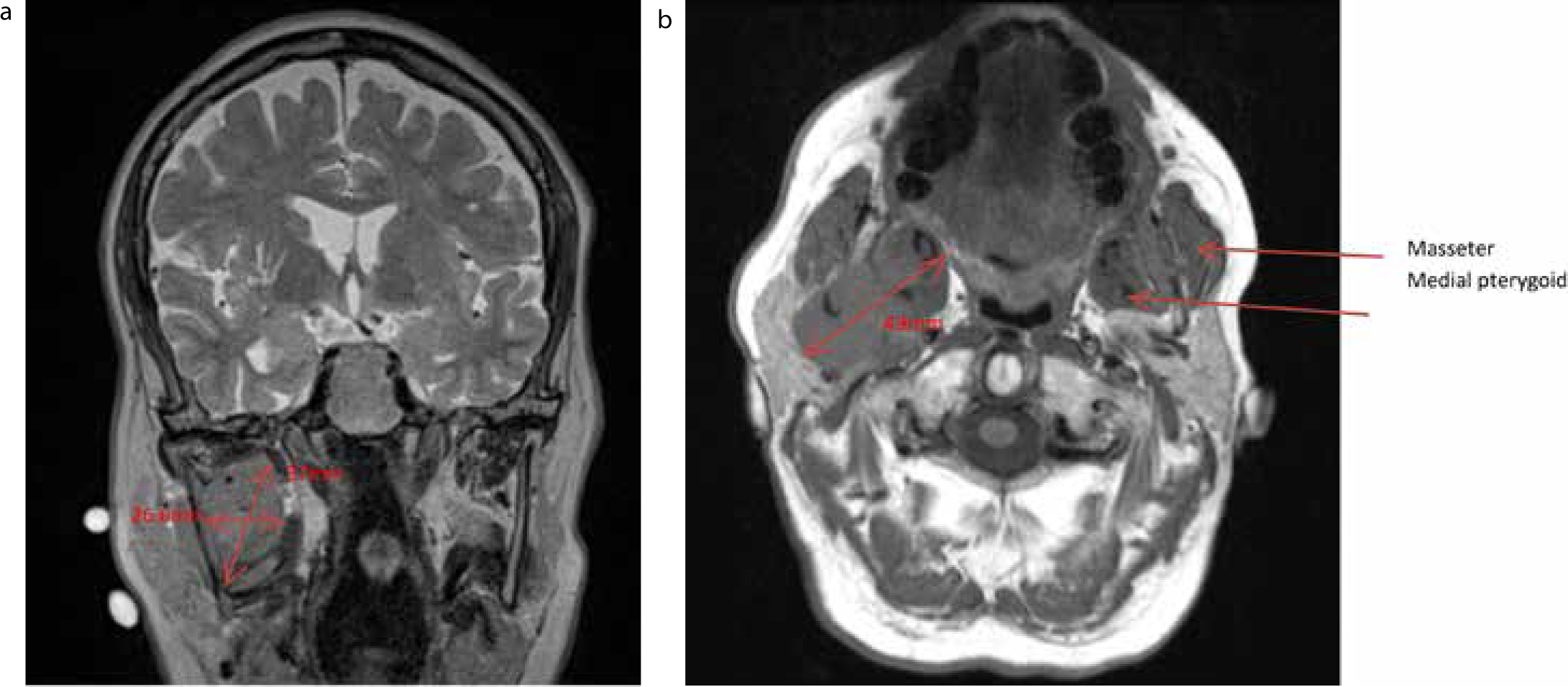
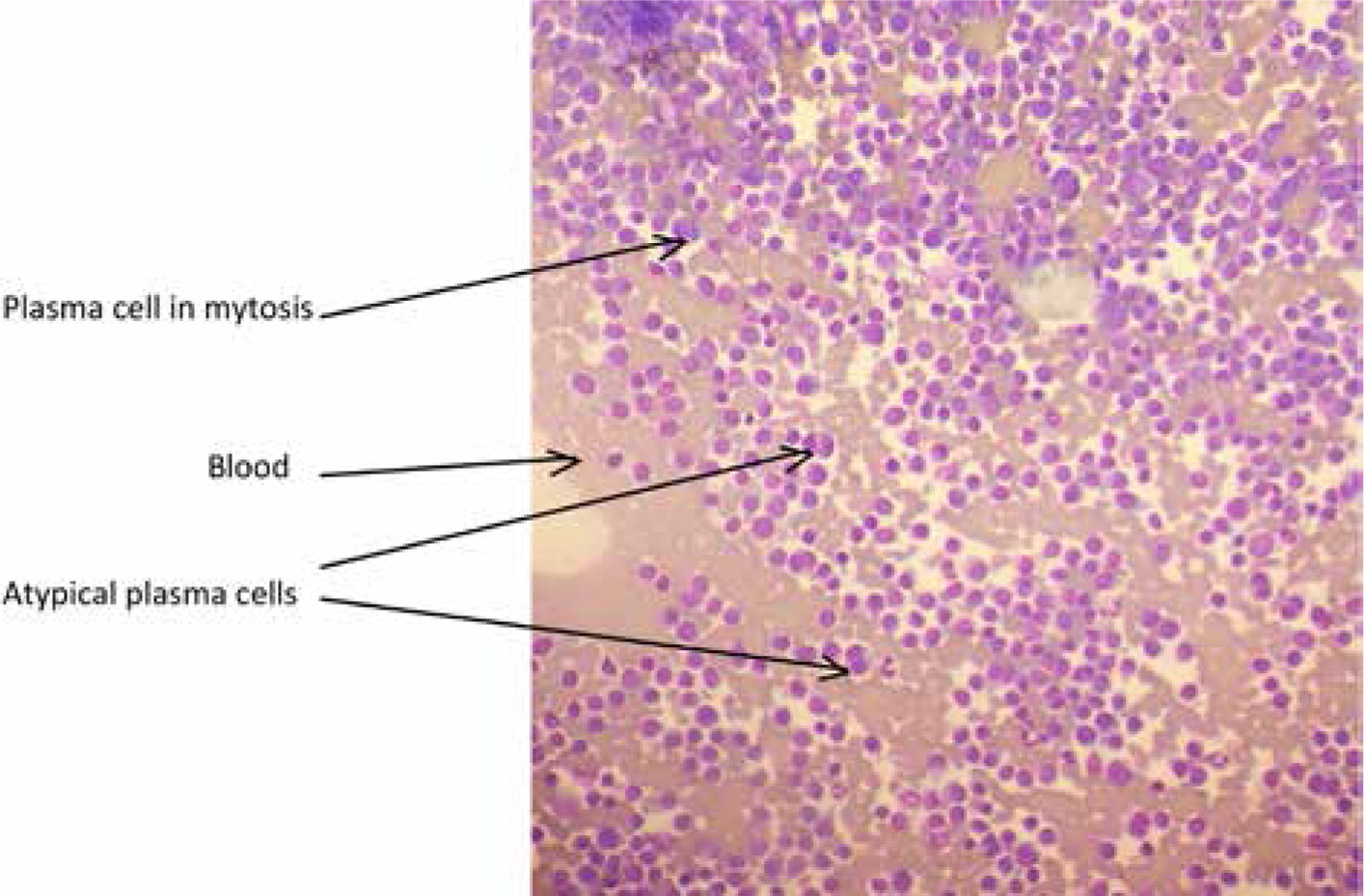
This is a case of a patient presenting to his general dental practitioner (GDP) with altered sensation in his lower lip with no obvious cause. Due to a prompt referral, the patient was investigated and diagnosed with an extramedullary presentation of multiple myeloma. A numb lip can present in general dental practice, although this is not common. There are several causes, for example, dental infection or fractured mandible.