Aggressive periodontitis (AgP) is considered a complex periodontal disease affecting the dentition with pronounced and rapid destruction of the periodontium and may result in loss of teeth and/or formation of advanced periodontal defects.1
Advantages in the use of systemic antibiotics in the therapy of AgP have been published,2 and studies have indicated that subjects with AgP significantly benefit from the adjunctive use of amoxicillin and metronidazole.3,4,5
Periodontal therapy should ideally not only resolve inflammation and arrest disease progression, but also regenerate lost periodontal attachment (ie formation of cementum, periodontal ligament and alveolar bone). The use of enamel matrix derivatives (EMD) proteins in the therapy of periodontal defects has demonstrated promising clinical outcomes for the treatment of periodontal lesions, such as intra-bony defects6 and furcation involvement.7 Additionally, histological findings have supported the use of enamel matrix derivative proteins to promote tissue regeneration in periodontal defects.8
Considering that periodontal maintenance is recognized as an integral part of periodontal therapy, and taking into account that it has a significant impact on periodontal prognosis and eventual tooth survival,9,10 the present case report aimed to treat a patient with generalized AgP, presenting advanced osseous defects, by using a regenerative therapy with EMD in combination with antibiotic therapy and, subsequently, performing a systematic periodontal supportive therapy.
Therapeutic approach
Initially, the patient was treated with a non-surgical scaling and root planing performed in four sessions with weekly intervals. Then, at the end of the non-surgical therapy, the patient received an adjunctive combination of systemic amoxicillin (500 mg) and metronidazole (400 mg). Both antibiotics were administered 3 times per day for 7 days.
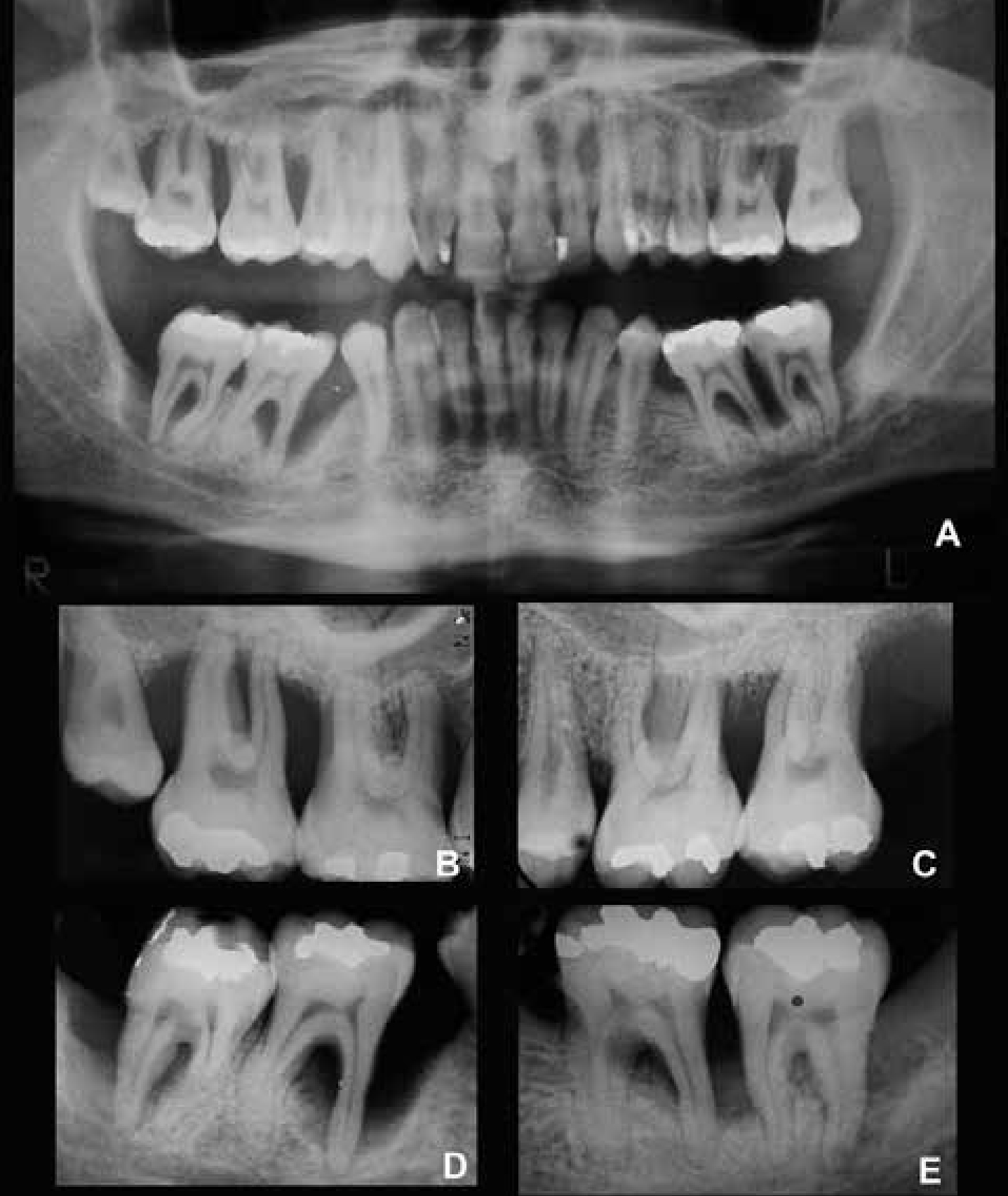
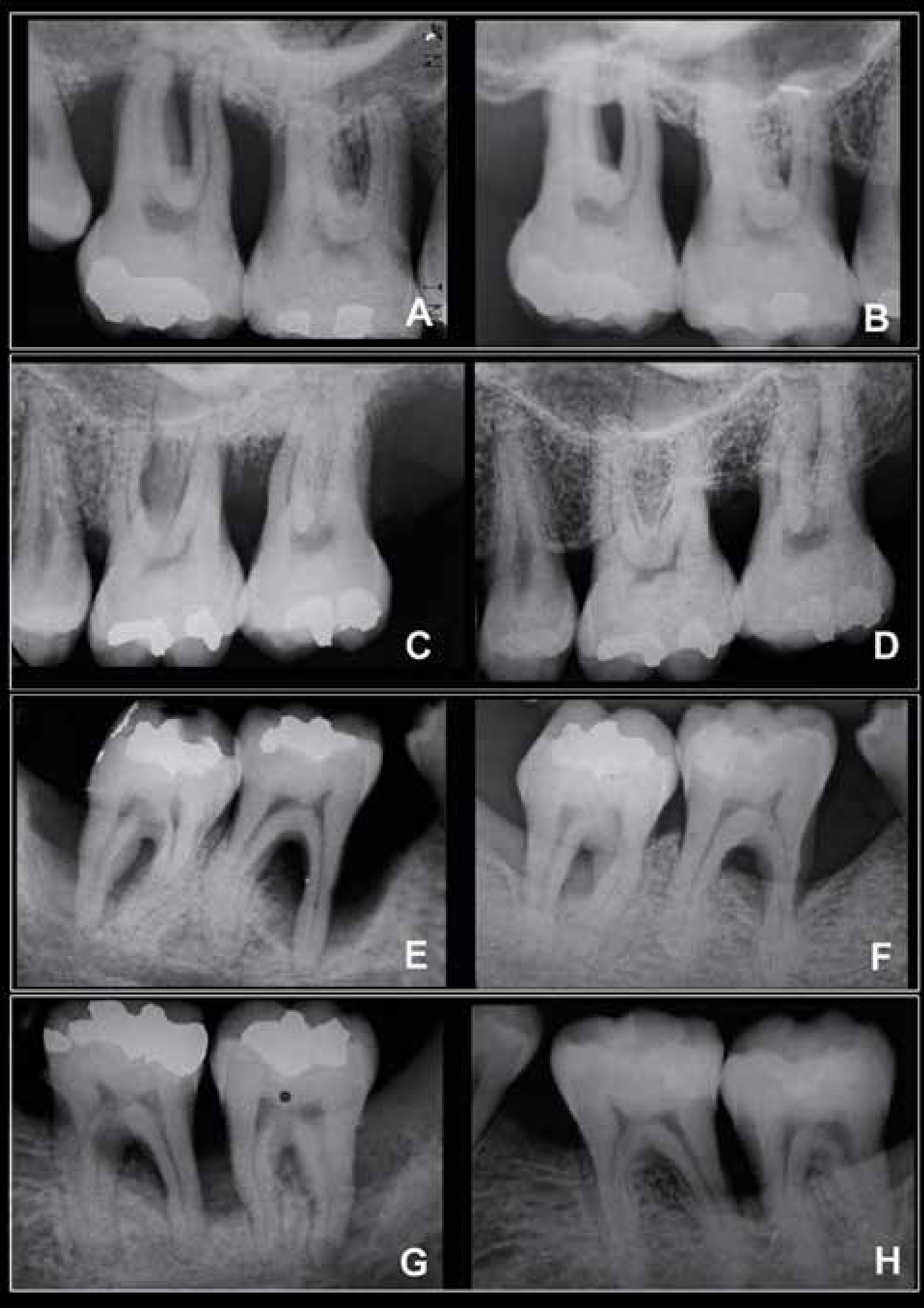
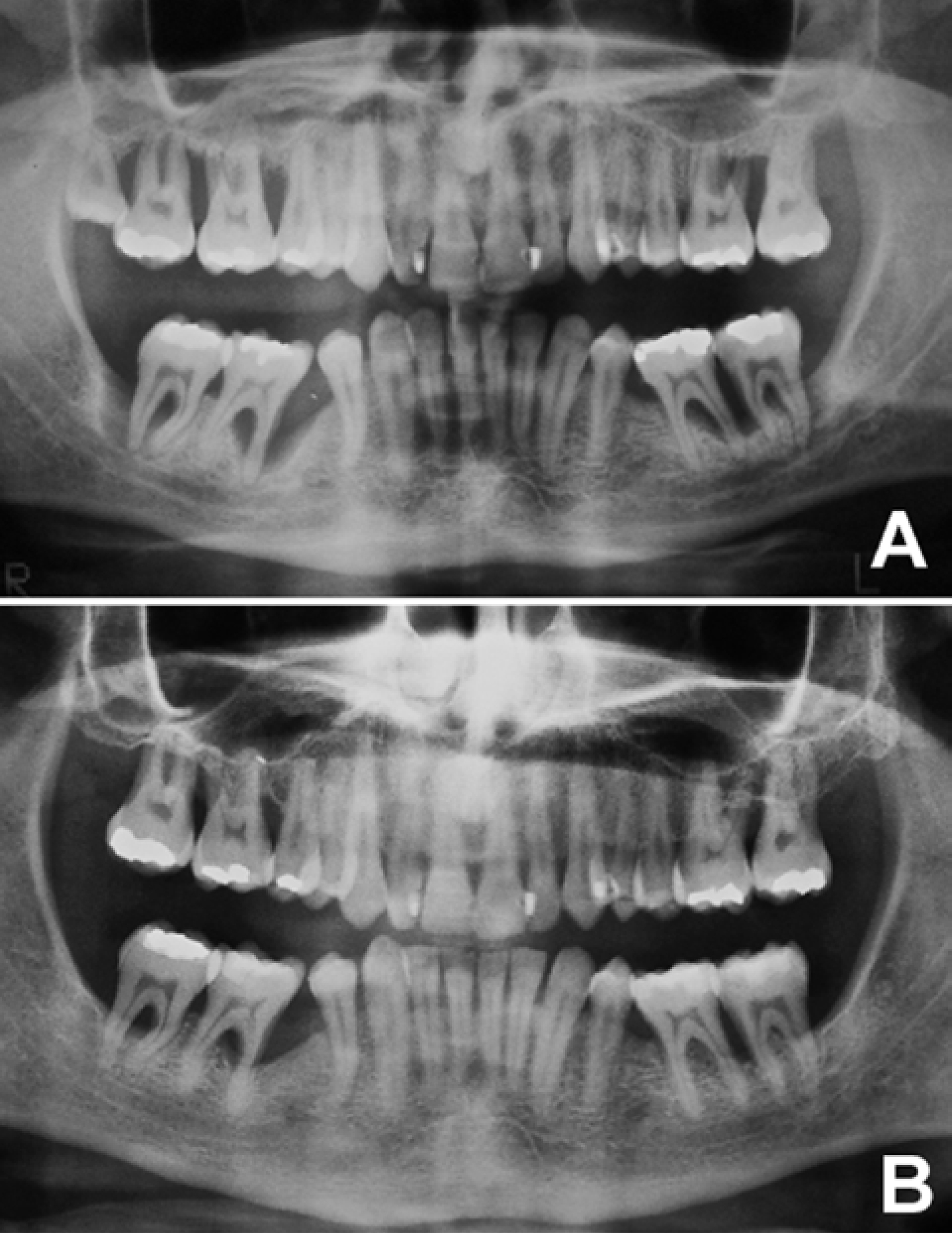
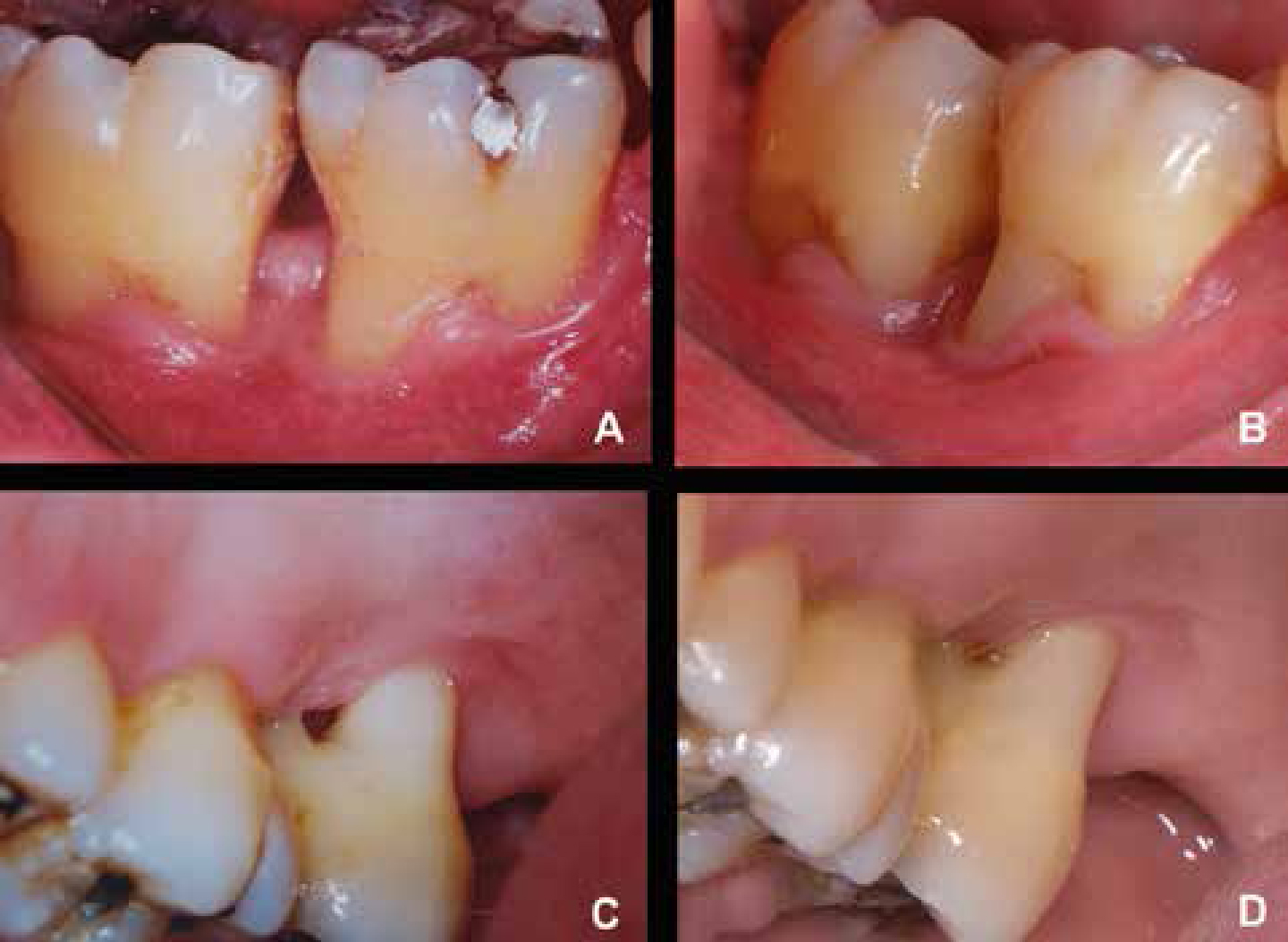
After three months, all mandibular and maxillary first and second molars presented residual pockets with PD and CAL >5 mm with bleeding on probing (BOP) and radiographic evidence of intra-bony defects and furcation lesions. In the maxillary molars, the degrees of furcation involvement were recorded as Class II furcation at mesial, distal and vestibular of tooth UR6 and UL6 and Class III furcation at mesial, distal and vestibular of tooth UR7 and UL7. In the mandibular molars, the degrees of furcation involvement were recorded as Class II furcation at vestibular of tooth LR7 and LL7 and vestibular and lingual of tooth LR6 and Class III furcation at tooth LL6. At this time, FMPS and FMBS were <20%.
These sites were treated by a regenerative surgical approach by using EMD.
Regenerative surgical procedure
One hour before therapy, the patient received a dose of 4 mg dexamethasone (Roche, São Paulo, Brazil). Intra-oral antisepsis was performed with 0.12% chlorhexidine rinse solution and extra-oral antisepsis was carried out with iodine solution. Following local anaesthesia, periodontal defects were accessed by intrasulcular incisions and vertical-releasing incisions were avoided. Full-thickness flaps were elevated and granulation tissues, as well as the visible calculus, were removed with curettes (Gracey, Hu-Friedy, Chicago, EUA). The root surfaces were conditioned with EDTA 24% for 2 minutes and then irrigated with saline solution. The sites then received an application of EMD (Emdogain®, Biora AB, Malmo, Sweden), according to the manufacturer's recommendations. The protein gel was applied from the farthest end of the involved defect until all the space was covered with EMD. The flaps were then repositioned and passive internal mattress sutures were placed (6.0 polygalactin-A; Vicryl, Johnson & Johnson, São Paulo, Brazil) to obtain primary closure of the inter-dental tissues.
At the end of the surgery, the patient received analgesic paracetamol medication (Tylenol®, 750 mg, Janssen-Cilag Farmacêutica Ltda, São Paulo, Brazil) and was instructed to take the medication every 6 hours, only if he experienced pain. For biofilm control, the patient was instructed to rinse with a 0.12% chlorhexidine solution twice a day for 30 days. The sutures were removed 10 days post-surgery.
Re-assessment evaluations
After the regenerative procedure, re-assessment visits were given every 15 days during the first month and monthly until the third month following the surgical procedure. After that, re-assessment visits occurred every year. During these appointments, the examiner recorded the clinical periodontal parameters and checked any change in the medical or health status. At the end of the appointments, a session of supragingival prophylaxis was performed, as necessary.
Discussion
Generalized aggressive periodontitis patients may have an imbalance in the host response, with reduced levels of anti-inflammatory cytokines and immunoglobulin, and increased periodontal pathogens.13 The treatment and long-term maintenance of the therapeutic outcomes in these patients represent a challenge for clinicians. The aim of this case report was to illustrate the clinical and radiographic improvements obtained following a 10-year periodontal supportive therapy after an antibiotic and regenerative approach to treat generalized AgP. It was demonstrated that successful outcomes may be achieved following this therapeutic approach, since satisfactory supportive periodontal therapy has been maintained.
As performed in other profiles of periodontal disease, the primary therapeutic approach during the treatment of AgP is based on mechanical means by using non-surgical and surgical techniques. However, it is known that the use of mechanical approaches alone has presented limitations to achieve and maintain predictable periodontal health in an extended period of time. It may be hypothesized that the bacterial recolonization could not be prevented through mechanical techniques alone,4 indicating that the adjunctive use of antibiotics may be important to promote benefits in the clinical improvements and also to provide a better outcome of attachment levels compared to mechanical therapy alone.4,14 The combined use of systemically administered amoxicillin and metronidazole has been suggested as a regimen with increased bactericidal profile and spectral efficacy.14
In addition to the use of systemic antibiotic therapy, in the current case report, osseous periodontal defects were also treated with EMD and the use of this regenerative procedure may have contributed to the clinical improvements verified in this report. Harrel et al showed that the EMD yielded significant reductions in probing depths and improvements in attachment levels after 6 years.15 Similar results were also obtained by other studies, in different follow-up periods, showing the benefits of EMD therapy in the treatment of intra-bony and furcation defects.16,17 In addition to the clinical improvements observed in this case report, radiographic assessments suggest an important bony fill in the periodontal defects treated by EMD after 10 years. In addition, Casarin et al have revealed that EMD therapy promoted a reduction in the number of Class II proximal furcations after 2 years of treatment compared with open flap debridement therapy.7 According to the results observed in this case report, it may be suggested that the bony fill detected in consequence of EMD use could contribute to the stability of periodontal treatment outcome over a longer period, promoting an improvement in the prognosis of teeth presenting periodontal osseous lesions.
Although numerous studies have revealed positive outcomes following the therapy with enamel matrix derivative proteins,6,7,15,16,17 the regenerative results promoted by the use of EMD in periodontal defects present a high variability and the extent of tissue regeneration which can be predicted after EMD use has not yet been established.16,18 It may be speculated that this heterogeneity could be partly promoted by variations in the defect configuration and characteristics,16,18 such as baseline probing depths, number of walls and defect angle of intra-bony defects or degree of furcation involvement.19,20 Among other factors, these characteristics of the defects may interfere in the response following EMD use, and these anatomical features need to be considered during the decision-making process about therapies to treat periodontal defects with regenerative approaches.
With the advent of osseointegrated implant therapy, a treatment alternative to periodontal regenerative approaches in teeth presenting advanced lost attachment apparatus has been considered. When placed in an adequate position, with satisfactory prosthesis design and ideal maintenance, implants may achieve high long-term survival rate.21,22 However, biological and technical complications may be frequent and a number of limitations, including bone density and quantity and areas requiring sinus floor or osseous grafts, must be considered. In addition, patients with a history of periodontitis may have lower implant survival rates than patients without a history of periodontitis and be more prone to biological complications such as peri-implantitis.22 In this context, it is essential to bear in mind that maintenance of the natural dentition in adequate function and aesthetics remains the main aim of any periodontal therapy, as supported by the present case report.
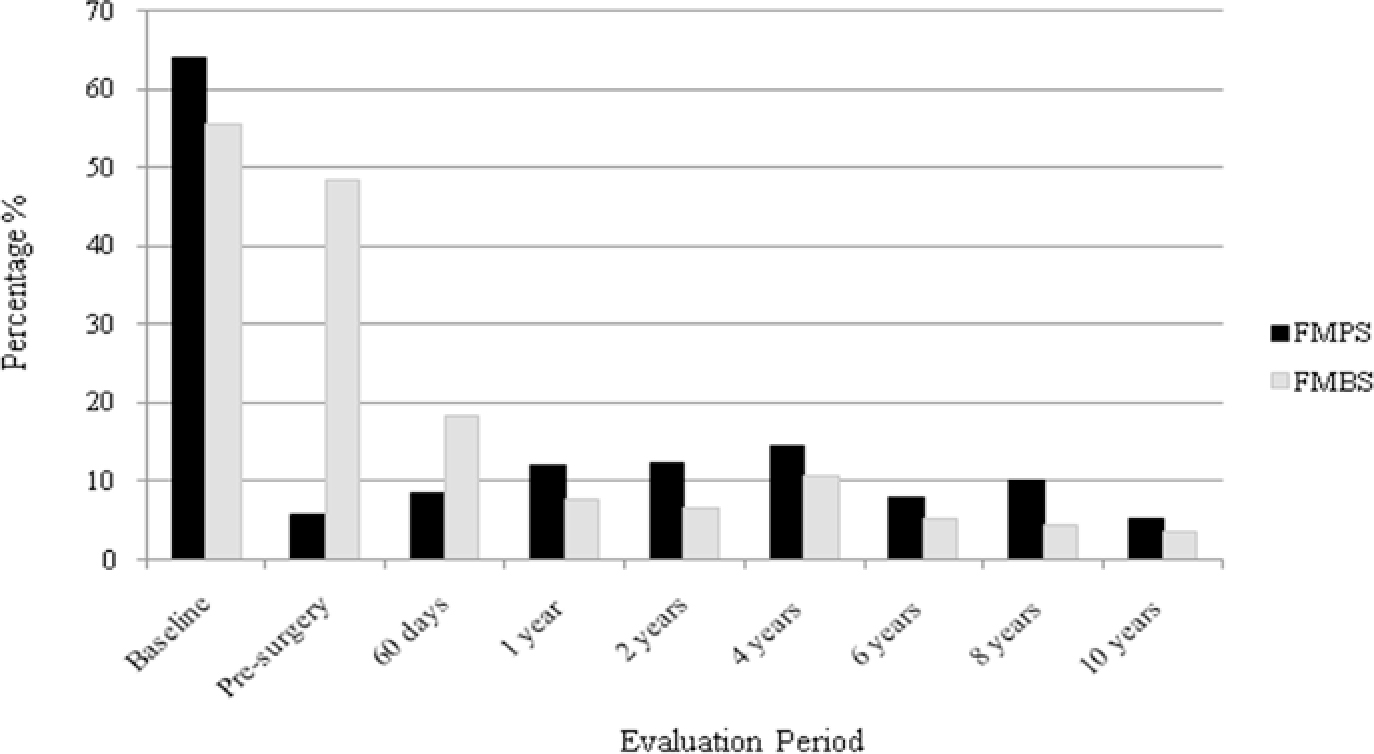
Thus, when faced with advanced periodontal defects, especially in subjects with generalized AgP, the clinician's decision about whether to save or extract a compromised tooth should consider a large number of factors, which include tooth type, furcation lesions involvement and presence of angular defects, tooth mobility, degree of alveolar bone loss, and mainly, patient compliance with the periodontal supportive therapy.9,10,23 An essential aspect to be considered when evaluating the findings of this report is that the positive results obtained in terms of PD reduction and CAL gain could be attributed to the rigorous periodontal maintenance (professional plaque control and reinforcement of oral hygiene instructions) carried out at periodic intervals and confirmed by the satisfactory FMPS and FMBS achieved at the re-evaluations during 10 years. Accordingly, studies have shown that, in conjunction with professional maintenance and acceptable plaque control, periodontal therapeutic approaches, including regenerative surgical therapies using EMD, are effective for efficiently improving clinical and radiographic parameters, even in the presence of periodontal bony defects.7,24 In line with these findings, Miyamoto et al suggested that patient compliance with periodontal maintenance can be substantially important for tooth retention among molars.25 These aspects reinforce the premise that adequate supportive care in a periodontal office is mandatory to maintaining the long-term success of periodontal therapy.9,10
Additionally, other important aspects to be considered during the decision-making process, about how to treat advanced periodontal bony defects in subjects presenting AgP, should take into account the cost-benefit ratio for both clinicians and patients from biological and economic viewpoints and the patient profile. Moreover, the strategic value of teeth in relation to overall treatment plan, patient's age, patient's functional and aesthetic demands, general health conditions and smoking habits need to be considered.
Of additional interest, considering the complex pathogenesis of AgP, there is a consensus that the use of adjunctive antibiotics provides a better therapeutic outcome.14 It is established that the periodontal bacterial profile is ample, requiring a combination of multiple antibacterial agents. Thus, the regime of antibiotic used in the present case report, by means of a combination of distinct antibiotics, is well established in the literature.2 In this context, combined use of amoxicillin and metronidazole has been proposed as a useful regimen with increased bactericidal and spectral efficacy compared to monotherapy with each drug.2,14
Also of note is that the high-risk profile of the patient at baseline was subsequently changed to a low-risk profile, reflecting the non-recurrence of periodontitis, the maintenance of teeth, and the preservation of alveolar bone.