Article
Centric Relation (CR) is the reference position of the jaws (which is not dependent on the teeth) when the mandibular condyles are in their uppermost position in the glenoid fossa, involving the least stress being placed on the jaw muscles. It is a natural, physiological position that is repeatable, reproducible and transferable for the purpose of mounting study casts on an articulator.
The author has found the bimanual manipulation technique¹ to locate CR often difficult to use, the Lucia Jig² method somewhat time-consuming, and the leaf gauge³ method manually tricky with respect to keeping the gauge held in situ whilst taking a jaw registration. The ESIPC jig has overcome these difficulties for the author because it is easy and quick to make and is self-retentive (but still easily removed when required). The ESIPC jig is also versatile as it can subsequently be removed, replaced, remade or repositioned, if necessary, without losing the captured CR position (this is particularly useful when it is used during the provision of direct composite build-ups in toothwear cases).
The method of making the ESIPC jig is shown in Figure 1 and described as follows:
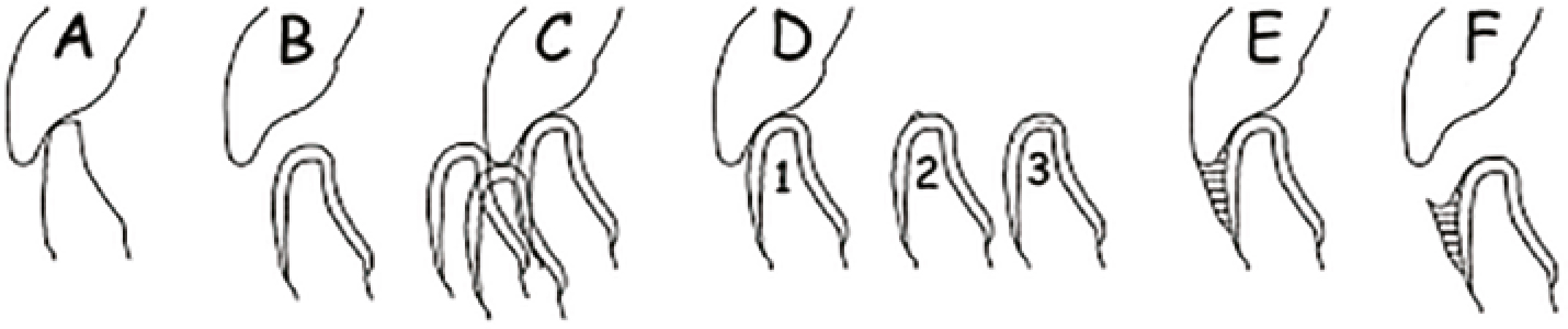
Subsequently, the fabricated ESIPC Jig can be used as follows:
It is understandable that some colleagues will have concerns regarding the use of an ESIPC jig. It was suggested by the reviewer that a comparison be made of the occlusal contacts on completion of a case with those at a review visit in order to help confirm the effectiveness, or otherwise, of the ESIPC jig in locating CR. To this end, the author can report that, with three moderate-to-severe wear cases, the occlusion was checked at review by an independent clinician, very experienced in the re-organization of occlusions, who confirmed that CR was indeed coincident with CO in each case. Consequently, he has and continues to have every confidence that this strongly suggests that the ESIPC jig can be a simple, accurate, effective and reliable method in helping clinicians to locate CR.
Indeed, this confidence has been confirmed and reinforced by the encouragement, support and positive feedback from colleagues who have already incorporated the ESIPC jig into their clinical practices with great enthusiasm, having been shown its clinical fabrication and use by the author.
Please note that if, in a very difficult case, the retruded arc of closure cannot be achieved using this method, an alternative device, such as a Lucia jig, may be employed.
The traditional Lucia jig, which has served dentists well, is designed to present a smooth palatally-facing inclined plane (to control the OVD) while the angle of the slope encourages the mandible to move posteriorly and superiorly (which is usually what's needed) and it also permits lateral repositioning. It can be made very quickly using heat-softened brown compound (Compound stick, various types, Keystone Industries, Myerstown, PA 17067).
Clinicians may well consider the ESIPC jig to be less able to allow these movements, nevertheless, it has (in the author's opinion) the advantage of simplicity and, since its inception, continues to serve the author well, demonstrating a particularly delightful degree of clinical efficacy, so much so that he now considers it to be an indispensable tool for use in his clinical practice (even though it's being presented in this article as an option that's available for colleagues to consider as an alternative to the available conventional approaches).
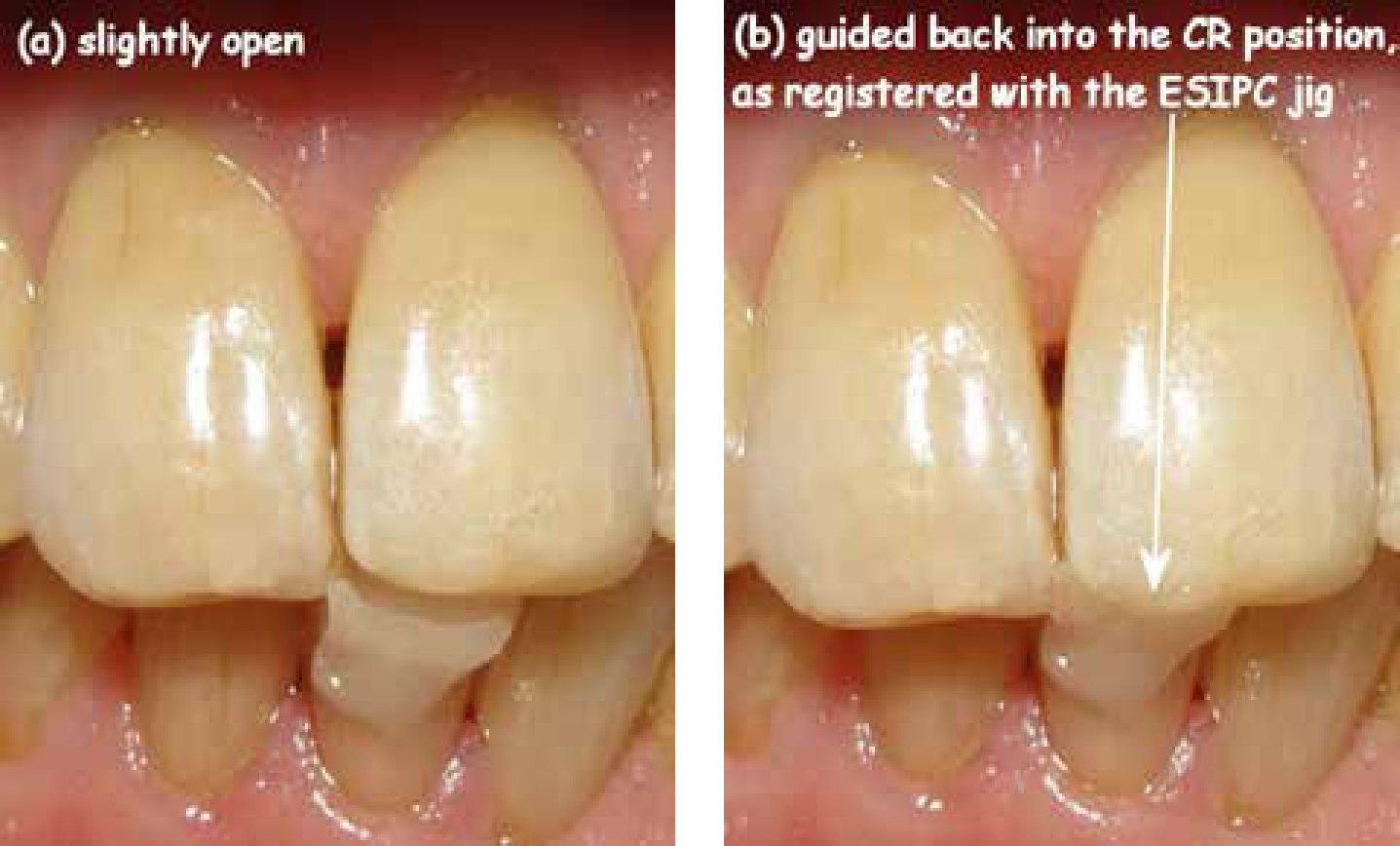
In Figure 2 it is possible to see the ease with which the fully formed ESIPC jig can be used to show the captured CR position repeatedly, consistently and accurately, once the second increment has fully set.
Addendum
The aim of this article was to describe the clinical fabrication and use of a novel jig to help locate, capture and subsequently record CR. It has been commented that the traditional anterior Lucia jig has been used for doing the same job (ie locating CR) in an evidence-based way for many years (the author certainly would not disagree with this), making the ESIPC jig effectively redundant. It is with regards to this latter comment that the author's opinion, with respect, is vehemently at variance (even though the comment does, at the same time, appear to suggest a degree of acceptance, however limited, that the premise of this article holds true).
To clarify, the ESIPC jig, in the author's opinion (and that of many of his colleagues) has significant advantages in its utility when compared to the traditional Lucia jig, other than just the ease of fabrication. For example, with the completed ESIPC jig, the clinician has the option to:
The author would also like to point out that, with its intra-oral use in toothwear cases, the ESIPC jig allows the clinician to use the patient's dentition as ‘mounted study casts’ (for direct rather than indirect restoration placement), and the patient's jaws as a fully self-adjustable, self-setting, articulator and thus no complex measurements or settings are required. Please note that the author has the confidence to say this is based on a background of many years' experience re-organizing the worn dentition adhesively. Thus, whatever he may be lacking in terms of academic knowledge on occlusion or toothwear (and he would not deny this), he personally feels that this is more than amply compensated for by 18 years of invaluable, hands-on, clinical experience in general dental practice.
The author hopes that this helps to demonstrate the fundamentally important, different, valid and novel role now occupied by the ESIPC jig. Far from being unnecessary or redundant, for the author (along with some enlightened colleagues), the unique advantages conferred by the ESIPC jig have already made it an absolute pre-requisite for use in the treatment of toothwear cases, adhesively.
There were also concerns that frequent late changes in the mandibular position could occur whilst the inter-occlusal record is made, but the author has already stated that he has simply not experienced this. If, and when, he does, it should be noted that the use of an additive (composite resin) adhesive approach would allow any corrective adhesive re-treatment to be carried out with consummate ease, particularly as the underlying healthy tooth tissue is still available. To help illustrate the point, Figure 3 shows a summary of the ESIPC jig being used in the re-treatment of a failed toothwear case (the original treatment had been provided elsewhere).

If, perhaps, there is an interest expressed by colleagues as a result of reading this article, it is my intention to produce a follow-up article, giving more detailed information regarding the technique to utilize the ESIPC jig as effectively as shown below in Figure 3.

